Why Home Visiting?
The evidence base for home visiting, including its cost effectiveness, is strong and growing. Below are examples of home visiting's demonstrated impact on critical needs and why home visiting is a key service strategy for improving infant, maternal, and family outcomes.

Home visiting has measurable benefits.
By meeting families where they are, home visiting programs have demonstrated short- and long-term impacts on the health, safety, and school-readiness of children; maternal health; and family stability and financial security. Home visitors are able to meet with families in their home and provide culturally competent, individualized needs assessments and services. This results in measured improvements in the following outcomes:
Healthy Babies
Home visitors work with expectant mothers to access prenatal care and engage in healthy behaviors during and after pregnancy. For example—
- Pregnant participants are more likely to access prenatal care and carry their babies to term.
- Home visiting promotes infant caregiving practices like breastfeeding, which has been associated with positive long-term outcomes related to cognitive development and child health.
Safe Homes and Nurturing Relationships
Home visitors provide caregivers with knowledge and training to reduce the risk of unintended injuries. For example—
- Home visitors teach caregivers how to “baby proof” their home to prevent accidents that can lead to emergency room visits, disabilities, or even death.
- They also teach caregivers how to engage with children in positive, nurturing ways, thus reducing child maltreatment .
Optimal Early Learning and Long-Term Academic Achievement
Home visitors offer caregivers timely information about child development and the importance of early childhood in establishing the building blocks for life. For example—
- They help caregivers recognize the value of reading and other activities for early learning. This guidance translates to improvements in children’s early language and cognitive development, as well as academic achievements in grades 1 through 3 .
Supported Families
Home visitors make referrals and coordinate services for children and caregivers, including job training and education programs, early care and education services, and— if needed—mental health and domestic violence resources. Research shows that—
- Compared with their counterparts, caregivers enrolled in home visiting have higher monthly incomes, are more likely to be enrolled in school , and are more likely to be employed .
Home visiting is cost effective.
Studies have found a return on investment of $1.80 to $5.70 for every dollar spent on home visiting. This strong return on investment is consistent with established research on other types of early childhood interventions.
Learn more in our Primer and annual Yearbook .
Home Visiting

Stay up to date on the latest home visiting information.

- Copy/Paste Link Link Copied
What happens during prenatal visits?
What happens during prenatal visits varies depending on how far along you are in your pregnancy.
Schedule your first prenatal visit as soon as you think you are pregnant, even if you have confirmed your pregnancy with a home pregnancy test. Early and regular prenatal visits help your health care provider monitor your health and the growth of the fetus.
The First Visit
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1
You've probably heard pregnancy discussed in terms of months and trimesters (units of about 3 months). Your health care provider and health information might use weeks instead. Here's a chart that can help you understand pregnancy stages in terms of trimesters, months, and weeks.
Because your first visit will be one of your longest, allow plenty of time.
During the visit, you can expect your health care provider to do the following: 1
- Answer your questions. This is a great time to ask questions and share any concerns you may have. Keep a running list for your visit.
- Check your urine sample for infection and to confirm your pregnancy.
- Check your blood pressure, weight, and height.
- Calculate your due date based on your last menstrual cycle and ultrasound exam.
- Ask about your health, including previous conditions, surgeries, or pregnancies.
- Ask about your family health and genetic history.
- Ask about your lifestyle, including whether you smoke, drink, or take drugs, and whether you exercise regularly.
- Ask about your stress level.
- Perform prenatal blood tests to do the following:
- Determine your blood type and Rh (Rhesus) factor. Rh factor refers to a protein found on red blood cells. If the mother is Rh negative (lacks the protein) and the father is Rh positive (has the protein), the pregnancy requires a special level of care. 2
- Do a blood count (e.g., hemoglobin, hematocrit).
- Test for hepatitis B, HIV, rubella, and syphilis.
- Do a complete physical exam, including a pelvic exam, and cultures for gonorrhea and chlamydia.
- Do a Pap test or test for human papillomavirus (HPV) or both to screen for cervical cancer and infection with HPV, which can increase risk for cervical cancer. The timing of these tests depends on the schedule recommended by your health care provider.
- Do an ultrasound test, depending on the week of pregnancy.
- Offer genetic testing: screening for Down syndrome and other chromosomal problems, cystic fibrosis, other specialized testing depending on history.
Prenatal Visit Schedule
If your pregnancy is healthy, your health care provider will set up a regular schedule for visits that will probably look about like this: 1
Later Prenatal Visits
As your pregnancy progresses, your prenatal visits will vary greatly. During most visits, you can expect your health care provider to do the following:
- Check your blood pressure.
- Measure your weight gain.
- Measure your abdomen to check your developing infant's growth—"fundal height" (once you begin to "show").
- Check the fetal heart rate.
- Check your hands and feet for swelling.
- Feel your abdomen to find the fetus's position (later in pregnancy).
- Do tests, such as blood tests or an ultrasound exam.
Talk to you about your questions or concerns. It's a good idea to write down your questions and bring them with you.
Several of these visits will include special tests to check for gestational diabetes (usually between 24 and 28 weeks) 3 and other conditions, depending on your age and family history.
In addition, the Centers for Disease Control and Prevention and the American Academy of Pediatrics released new vaccine guidelines for 2013 , including a recommendation for pregnant women to receive a booster of whooping cough (pertussis) vaccine. The guidelines recommend the shot be given between 27 and 36 weeks of pregnancy. 4
- Centers for Disease Control and Prevention. (2013). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (TDAP) in pregnant women―Advisory Committee on Immunization Practices (ACIP), 2012. Retrieved September 20, 2013, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6207a4.htm
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Prenatal visits: What to expect and how to prepare
Regular prenatal visits are an important part of your pregnancy care. Find out how often you'll see a healthcare provider, what to expect at each appointment, and smart ways to prepare.

When to schedule a prenatal visit
Prenatal visitation schedule, how should i prepare for a prenatal visit, what happens during prenatal visits, how can i make the most of my pregnancy appointments.
Make an appointment for your first prenatal visit once you're aware you are pregnant – when you receive a positive home pregnancy test, for example. Booking it around week 8 of pregnancy is typical.
You'll come back regularly in the weeks and months following that initial appointment. Most people have between 8 and 14 prenatal visits throughout the course of their pregnancy.
During this time, you'll see a lot of your healthcare practitioner. That's why it's so important to choose someone you like and trust. If you're not comfortable or satisfied with your provider after your first visit or visits, don't be afraid to find someone with whom you have a better connection.
Typically, a pregnant woman will visit their doctor, midwife , or nurse practitioner every four weeks during the first and second trimesters. In the third trimester, you'll be seen more often – usually every other week until 36 weeks, and then every week until the baby is born.
For more information on what happens at these visits, see:
Your first prenatal visit
Second trimester prenatal visits (14 weeks to 27 weeks)
Third trimester prenatal visits (28 weeks through the end of pregnancy)
The specific number of scheduled appointments you'll have depends on if your pregnancy is considered to be high-risk. This is determined by your medical history and whether you have any complications or conditions that warrant more frequent checkups, such as gestational diabetes , high blood pressure , or a history of preterm labor . If you've had any medical problems in the past or develop any new problems during this pregnancy, you may need more prenatal visits than the average pregnant woman.
In the weeks before each visit, jot down any questions or concerns in a notebook or a notes app on your smartphone. This way, you'll remember to ask your practitioner about them at your next appointment. You may be surprised by how many questions you have, so don't miss the opportunity to get some answers in person.
For example, before you drink an herbal tea or take a supplement or an over-the-counter medication , ask your provider about it. You can even bring the item itself – or a picture of the label – with you to your next appointment. Then, your doctor, midwife, or nurse practitioner can read the label and let you know whether it's okay to ingest.
Of course, if you have any pressing questions or worries, or develop any new, unusual, or severe symptoms , don't wait for your appointment – call your practitioner right away.
In addition to your list, you may want to bring a partner, friend, family member, or labor coach with you to some or all of your prenatal visits. They can comfort you, take notes, ask questions, and help you remember important information.
The goal of prenatal visits is to see how your pregnancy is proceeding and to provide you with information to help keep you and your baby healthy. It's important that you go to all of your prenatal appointments, even if you're feeling just fine and believe that everything is progressing perfectly.
Your practitioner will start by asking how you're feeling physically and emotionally, whether you have any complaints or worries, and what questions you may have. They'll also ask you about your baby's movements once you begin to feel them, typically during the second trimester. Your practitioner will have other questions as well, which will vary depending on how far along you are and whether there are specific concerns.
Your midwife, doctor, or nurse practitioner will also:
- Check your weight , blood pressure , and urine
- Check for swelling
- Measure your abdomen
- Check the position of your baby
- Listen to your baby's heartbeat
- Perform other exams and order tests, as appropriate
- Give you the appropriate vaccinations
- Closely monitor any complications you have or that you develop, and intervene if necessary
Near the end of your pregnancy, your provider may also do a pelvic exam to check for cervical changes. You will also discuss your delivery plan in more depth.
At the end of each visit, your practitioner will review their findings with you. They'll also explain the normal changes to expect before your next visit, warning signs to watch for, and the pros and cons of optional tests you may want to consider. Lifestyle issues will likely be a topic of discussion, as well. Expect to talk about the importance of good nutrition , sleep, oral health, stress management, wearing seatbelts, and avoiding tobacco , alcohol , and illicit drugs.
Many people look forward to their prenatal appointments but are disappointed to find that, with the exception of the first visit, they're in and out of the office in 10 minutes. A quick visit is typical and is usually a sign that everything is progressing normally. Still, you want to make sure your concerns are addressed – and that you and your baby are being well cared for.
Here are some things you can do to ensure that your prenatal visits are satisfying:
- Speak up. Your practitioner isn't a mind reader and won't be able to tell what you're thinking just by performing a physical exam. So, if anything is bothering you, say your piece. Are you having trouble controlling your heartburn ? Managing your constipation ? Suffering from headaches ? This is the time to ask for advice. Consult the notebook of questions you've been compiling. In addition to physical complaints, let your practitioner know if you have emotional concerns or fitness or nutrition questions.
- Ask the staff about the administrative stuff. Save your questions about things like insurance and directions to the hospital for the office staff so your practitioner has more time to answer your health-related questions. Go to the admin staff with any inquiries about payments, scheduling, office policies, and your contact information.
- Be open-minded. When talking with your doctor, midwife, or nurse practitioner, you should feel comfortable speaking freely. But remember to listen, too. Take notes if you find it helpful.
Keep in mind, too, that some days are busier than others. This is especially true during the COVID-19 pandemic. That doesn't mean your practitioner doesn't have to answer your questions, but sometimes a discussion can be continued at the next visit if it's a really busy day or if your practitioner needs to head to the hospital to deliver a baby.
At the same time, don't tolerate a healthcare practitioner who won't give you thorough answers, doesn't show reasonable compassion, or barely looks up from your chart. You and your baby deserve more than that.
Now that you know what to expect during all those prenatal visits, you might like a sneak peek at what else is in store. Here's an overview of the next nine months .
Learn more:
- The ultimate pregnancy to-do list: First trimester
- 12 steps to a healthy pregnancy
- When will my pregnancy start to show?
- Fetal development timeline
Was this article helpful?
What happens at second trimester prenatal appointments

What to expect at your first prenatal appointment

What to expect from third trimester prenatal appointments

Prenatal testing

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
MedlinePlus. (2021). Prenatal care in your first trimester. https://medlineplus.gov/ency/patientinstructions/000544.htm Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2017). Prenatal Care Checkups. https://www.marchofdimes.org/pregnancy/prenatal-care-checkups.aspx Opens a new window [Accessed September 21, 2021.]
Office on Women’s Health. (2019). Prenatal Care and Tests. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What happens during prenatal visits? https://www.nichd.nih.gov/health/topics/preconceptioncare/conditioninfo/prenatal-visits Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What is a high-risk pregnancy? https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/high-risk Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2018). What are some factors that make a pregnancy high-risk? https://www.nichd.nih.gov/health/topics/high-risk/conditioninfo/factors Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2020). Over-the-Counter Medicine, Supplements, and Herbal Products During Pregnancy. https://www.marchofdimes.org/pregnancy/over-the-counter-medicine-supplements-and-herbal-products.aspx Opens a new window [Accessed September 21, 2021.]
Associates in Women’s Healthcare (2021). Preparing for Your First Prenatal Visit. https://www.associatesinwomenshealthcare.net/blog/preparing-for-your-first-prenatal-visit/ Opens a new window [Accessed September 21, 2021.]
National Health Service (UK). (2018). Your baby’s movements. https://www.nhs.uk/pregnancy/keeping-well/your-babys-movements/ Opens a new window [Accessed September 21, 2021.]
MedlinePlus. (2021). Prenatal care in your third trimester. https://medlineplus.gov/ency/patientinstructions/000558.htm Opens a new window [Accessed September 21, 2021.]
UCLA Health. (2021). Schedule of prenatal care. https://www.uclahealth.org/obgyn/workfiles/Pregnancy/Schedule_of_Prenatal_Care.pdf Opens a new window [Accessed September 21, 2021.]
UCR Health. (2021). Healthy Pregnancy: The Importance of Prenatal Care. https://www.ucrhealth.org/2018/07/healthy-pregnancy-the-importance-of-prenatal-care/ Opens a new window [Accessed September 21, 2021.]
Mayo Clinic. (2020). Prenatal care: 1 st trimesters visits. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20044882 Opens a new window [Accessed September 21, 2021.]

Where to go next


- Pregnancy Classes

Your First Prenatal Visit
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant!
Even if you are not a first-time mother, prenatal visits are still important since every pregnancy is different. This initial visit will probably be one of the longest. It will be helpful if you arrive prepared with vital dates and information. This is also a good opportunity to bring a list of questions that you and your partner have about your pregnancy, prenatal care, and birth options.
What to Expect at Your First Pregnancy Appointment
Your doctor will ask for your medical history, including:.
- Medical and/or psychosocial problems
- Blood pressure, height, and weight
- Breast and cervical exam
- Date of your last menstrual period (an accurate LMP is helpful when determining gestational age and due date)
- Birth control methods
- History of abortions and/or miscarriages
- Hospitalizations
- Medications you are taking
- Medication allergies
- Your family’s medical history
Your healthcare provider will also perform a physical exam which will include a pap smear , cervical cultures, and possibly an ultrasound if there is a question about how far along you are or if you are experiencing any bleeding or cramping .
Blood will be drawn and several laboratory tests will also be done, including:
- Hemoglobin/ hematocrit
- Rh Factor and blood type (if Rh negative, rescreen at 26-28 weeks)
- Rubella screen
- Varicella or history of chickenpox, rubella, and hepatitis vaccine
- Cystic Fibrosis screen
- Hepatitis B surface antigen
- Tay Sach’s screen
- Sickle Cell prep screen
- Hemoglobin levels
- Hematocrit levels
- Specific tests depending on the patient, such as testing for tuberculosis and Hepatitis C
Your healthcare provider will probably want to discuss:
- Recommendations concerning dental care , cats, raw meat, fish, and gardening
- Fevers and medications
- Environmental hazards
- Travel limitations
- Miscarriage precautions
- Prenatal vitamins , supplements, herbs
- Diet , exercise , nutrition , weight gain
- Physician/ midwife rotation in the office
Possible questions to ask your provider during your prenatal appointment:
- Is there a nurse line that I can call if I have questions?
- If I experience bleeding or cramping, do I call you or your nurse?
- What do you consider an emergency?
- Will I need to change my habits regarding sex, exercise, nutrition?
- When will my next prenatal visit be scheduled?
- What type of testing do you recommend and when are they to be done? (In case you want to do research the tests to decide if you want them or not.)
If you have not yet discussed labor and delivery issues with your doctor, this is a good time. This helps reduce the chance of surprises when labor arrives. Some questions to ask include:
- What are your thoughts about natural childbirth ?
- What situations would warrant a Cesarean ?
- What situations would warrant an episiotomy ?
- How long past my expected due date will I be allowed to go before intervening?
- What is your policy on labor induction?
Want to Learn More?
- Sign up for our weekly email newsletter
- Bonding With Your Baby: Making the Most of the First Six Weeks
- 7 Common Discomforts of Pregnancy
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Leg Cramps During Pregnancy

Prenatal Vitamin Limits

Skin Changes During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Prenatal care
Prenatal care is the health care you get while you are pregnant.
What is prenatal care?
Prenatal care is the health care you get while you are pregnant. Take care of yourself and your baby by:
- Getting early prenatal care. If you know you're pregnant, or think you might be, call your doctor to schedule a visit.
- Getting regular prenatal care. Your doctor will schedule you for many checkups over the course of your pregnancy. Don't miss any — they are all important.
- Following your doctor's advice.
Why do I need prenatal care?
Prenatal care can help keep you and your baby healthy. Babies of mothers who do not get prenatal care are three times more likely to have a low birth weight and five times more likely to die than those born to mothers who do get care.
Doctors can spot health problems early when they see mothers regularly. This allows doctors to treat them early. Early treatment can cure many problems and prevent others. Doctors also can talk to pregnant women about things they can do to give their unborn babies a healthy start to life.
I am thinking about getting pregnant. How can I take care of myself?
You should start taking care of yourself before you start trying to get pregnant. This is called preconception health. It means knowing how health conditions and risk factors could affect you or your unborn baby if you become pregnant. For example, some foods, habits, and medicines can harm your baby — even before he or she is conceived. Some health problems also can affect pregnancy.
Talk to your doctor before pregnancy to learn what you can do to prepare your body. Women should prepare for pregnancy before becoming sexually active. Ideally, women should give themselves at least 3 months to prepare before getting pregnant.
The five most important things you can do before becoming pregnant are:
- Take 400 to 800 micrograms (400 to 800 mcg or 0.4 to 0.8 mg) of folic acid every day for at least 3 months before getting pregnant to lower your risk of some birth defects of the brain and spine. You can get folic acid from some foods. But it's hard to get all the folic acid you need from foods alone. Taking a vitamin with folic acid is the best and easiest way to be sure you're getting enough.
- Stop smoking and drinking alcohol. Ask your doctor for help.
- If you have a medical condition, be sure it is under control. Some conditions include asthma , diabetes , depression , high blood pressure , obesity , thyroid disease, or epilepsy . Be sure your vaccinations are up to date.
- Talk to your doctor about any over-the-counter and prescription medicines you are using. These include dietary or herbal supplements. Some medicines are not safe during pregnancy. At the same time, stopping medicines you need also can be harmful.
- Avoid contact with toxic substances or materials at work and at home that could be harmful. Stay away from chemicals and cat or rodent feces.
I'm pregnant. What should I do — or not do — to take care of myself and my unborn baby?
Follow these do's and don'ts to take care of yourself and the precious life growing inside you:
Health care do's and don'ts
- Get early and regular prenatal care. Whether this is your first pregnancy or third, health care is extremely important. Your doctor will check to make sure you and the baby are healthy at each visit. If there are any problems, early action will help you and the baby.
- Take a multivitamin or prenatal vitamin with 400 to 800 micrograms (400 to 800 mcg or 0.4 to 0.8 mg) of folic acid every day. Folic acid is most important in the early stages of pregnancy, but you should continue taking folic acid throughout pregnancy.
- Ask your doctor before stopping any medicines or starting any new medicines. Some medicines are not safe during pregnancy. Keep in mind that even over-the-counter medicines and herbal products may cause side effects or other problems. But not using medicines you need could also be harmful.
- Avoid x-rays. If you must have dental work or diagnostic tests, tell your dentist or doctor that you are pregnant so that extra care can be taken.
- Get a flu shot. Pregnant women can get very sick from the flu and may need hospital care.
Food do's and don'ts
- Eat a variety of healthy foods. Choose fruits, vegetables, whole grains, calcium-rich foods, and foods low in saturated fat. Also, make sure to drink plenty of fluids, especially water.
- Get all the nutrients you need each day, including iron. Getting enough iron prevents you from getting anemia, which is linked to preterm birth and low birth weight . Eating a variety of healthy foods will help you get the nutrients your baby needs. But ask your doctor if you need to take a daily prenatal vitamin or iron supplement to be sure you are getting enough.
- Protect yourself and your baby from food-borne illnesses, including toxoplasmosis (TOK-soh-plaz-MOH-suhss) and listeria (lih-STEER-ee-uh). Wash fruits and vegetables before eating. Don't eat uncooked or undercooked meats or fish. Always handle, clean, cook, eat, and store foods properly.
- Don't eat fish with lots of mercury, including swordfish, king mackerel, shark, and tilefish.
Lifestyle do's and don'ts
- Gain a healthy amount of weight. Your doctor can tell you how much weight gain you should aim for during pregnancy.
- Don't smoke, drink alcohol, or use drugs. These can cause long-term harm or death to your baby. Ask your doctor for help quitting.
- Unless your doctor tells you not to, try to get at least 2 hours and 30 minutes of moderate-intensity aerobic activity a week. It's best to spread out your workouts throughout the week. If you worked out regularly before pregnancy, you can keep up your activity level as long as your health doesn't change and you talk to your doctor about your activity level throughout your pregnancy. Learn more about how to have a fit pregnancy .
- Don't take very hot baths or use hot tubs or saunas.
- Get plenty of sleep and find ways to control stress.
- Get informed. Read books, watch videos, go to a childbirth class, and talk with moms you know.
- Ask your doctor about childbirth education classes for you and your partner. Classes can help you prepare for the birth of your baby.
Environmental do's and don'ts
- Stay away from chemicals like insecticides , solvents (like some cleaners or paint thinners), lead, mercury, and paint (including paint fumes). Not all products have pregnancy warnings on their labels. If you're unsure if a product is safe, ask your doctor before using it. Talk to your doctor if you are worried that chemicals used in your workplace might be harmful.
- If you have a cat, ask your doctor about toxoplasmosis . This infection is caused by a parasite sometimes found in cat feces. If not treated toxoplasmosis can cause birth defects. You can lower your risk of by avoiding cat litter and wearing gloves when gardening.
- Avoid contact with rodents, including pet rodents, and with their urine, droppings, or nesting material. Rodents can carry a virus that can be harmful or even deadly to your unborn baby.
- Take steps to avoid illness, such as washing hands frequently.
- Stay away from secondhand smoke.
I don't want to get pregnant right now. Should I still take folic acid every day?
Yes! Birth defects of the brain and spine happen in the very early stages of pregnancy, often before a woman knows she is pregnant. By the time she finds out she is pregnant, it might be too late to prevent those birth defects. Also, half of all pregnancies in the United States are not planned. For these reasons, all women who are able to get pregnant need 400 to 800 mcg of folic acid every day.
How often should I see my doctor during pregnancy?
Your doctor will give you a schedule of all the doctor's visits you should have while pregnant. Most experts suggest you see your doctor:
- About once each month for weeks 4 through 28
- Twice a month for weeks 28 through 36
- Weekly for weeks 36 to birth
If you are older than 35 or your pregnancy is high risk, you'll probably see your doctor more often.
What happens during prenatal visits?
During the first prenatal visit, you can expect your doctor to:
- Ask about your health history including diseases, operations, or prior pregnancies
- Ask about your family's health history
- Do a complete physical exam, including a pelvic exam and Pap test
- Take your blood and urine for lab work
- Check your blood pressure, height, and weight
- Calculate your due date
- Answer your questions
At the first visit, you should ask questions and discuss any issues related to your pregnancy. Find out all you can about how to stay healthy.
Later prenatal visits will probably be shorter. Your doctor will check on your health and make sure the baby is growing as expected. Most prenatal visits will include:
- Checking your blood pressure
- Measuring your weight gain
- Measuring your abdomen to check your baby's growth (once you begin to show)
- Checking the baby's heart rate
While you're pregnant, you also will have some routine tests. Some tests are suggested for all women, such as blood work to check for anemia, your blood type, HIV, and other factors. Other tests might be offered based on your age, personal or family health history, your ethnic background, or the results of routine tests you have had. Visit the pregnancy section of our website for more details on prenatal care and tests .
I am in my late 30s and I want to get pregnant. Should I do anything special?
As you age, you have an increasing chance of having a baby born with a birth defect. Yet most women in their late 30s and early 40s have healthy babies. See your doctor regularly before you even start trying to get pregnant. She will be able to help you prepare your body for pregnancy. She will also be able to tell you about how age can affect pregnancy.
During your pregnancy, seeing your doctor regularly is very important. Because of your age, your doctor will probably suggest some extra tests to check on your baby's health.
More and more women are waiting until they are in their 30s and 40s to have children. While many women of this age have no problems getting pregnant, fertility does decline with age. Women over 40 who don't get pregnant after six months of trying should see their doctors for a fertility evaluation.
Experts define infertility as the inability to become pregnant after trying for one year. If a woman keeps having miscarriages, it's also called infertility. If you think you or your partner may be infertile, talk to your doctor. Doctors are able to help many infertile couples go on to have healthy babies.
Where can I go to get free or reduced-cost prenatal care?
Women in every state can get help to pay for medical care during their pregnancies. This prenatal care can help you have a healthy baby. Every state in the United States has a program to help. Programs give medical care, information, advice, and other services important for a healthy pregnancy.
To find out about the program in your state:
- Call 800-311-BABY (800-311-2229). This toll-free telephone number will connect you to the Health Department in your area code.
- For information in Spanish, call 800-504-7081.
- Contact your local Health Department.
Did we answer your question about prenatal care?
For more information about prenatal care, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- American College of Obstetricians and Gynecologists Phone: 202-638-5577
- American Pregnancy Association Phone: 972-550-0140
- Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, HHS Phone: 800-370-2943 (TDD: 888-320-6942)
- March of Dimes Phone: 914-997-4488
- National Center on Birth Defects and Developmental Disabilities, CDC, HHS Phone: 800-232-4636 (TDD: 888-232-6348)
- John W. Schmitt, M.D., Associate Professor of Clinical Obstetrics and Gynecology, University of Virginia Medical School
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

Your First Prenatal Appointment
Medical review policy, latest update:.
Medically reviewed for accuracy.
When should I schedule my first prenatal visit?
When will my first prenatal visit take place, read this next, how should i prepare for my first pregnancy appointment, what will happen at my first prenatal visit, will i see my baby on an ultrasound at my first prenatal visit, updates history, jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
Dosage Effect of Prenatal Home Visiting on Pregnancy Outcomes in At-Risk, First-Time Mothers
Neera k. goyal.
Divisions of a Neonatology and Pulmonary Biology,
b Hospital Medicine,
c Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, Ohio
Eric S. Hall
d Biomedical Informatics,
Jareen K. Meinzen-Derr
e Biostatistics and Epidemiology,
Robert S. Kahn
f General Pediatrics, and
Jodie A. Short
Judith b. van ginkel, robert t. ammerman.
g Behavioral Medicine and Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; and
BACKGROUND AND OBJECTIVE:
Home visiting programs seek to improve care management for women at high risk for preterm birth (<37 weeks). Our objective was to evaluate the effect of home visiting dosage on preterm birth and small for gestational age (SGA) infants.
Retrospective cohort study of women in southwest Ohio with a singleton pregnancy enrolled in home visiting before 26 weeks’ gestation. Vital statistics and hospital discharge data were linked with home visiting data from 2007 to 2010 to ascertain birth outcomes. Eligibility for home visiting required ≥1 of 4 risk factors: unmarried, low income, <18 years of age, or suboptimal prenatal care. Logistic regression tested the association of gestational age at enrollment and number of home visits before 26 weeks with preterm birth. Proportional hazards analysis tested the association of total number of home visits with SGA status.
Among 441 participants enrolled by 26 weeks, 10.9% delivered preterm; 17.9% of infants were born SGA. Mean gestational age at enrollment was 18.9 weeks; mean number of prenatal home visits was 8.2. In multivariable regression, ≥8 completed visits by 26 weeks compared with ≤3 visits was associated with an odds ratio 0.38 for preterm birth (95% confidence interval: 0.16–0.87), while having ≥12 total home visits compared with ≤3 visits was significantly associated with a hazards ratio 0.32 for SGA (95% confidence interval: 0.15–0.68).
CONCLUSIONS:
Among at-risk, first time mothers enrolled prenatally in home visiting, higher dosage of intervention is associated with reduced likelihood of adverse pregnancy outcomes.
Preterm birth (birth before 37 weeks’ gestation) is the single most challenging problem in modern obstetric practice and child health. The last 4 decades have seen a rise in preterm birth rates, with 12% of pregnancies, or 500 000 infants annually, delivering prematurely in the United States. 1 Decades of research demonstrate that this outcome occurs with profound sociodemographic disparities and is mediated by a complex matrix of biological, genetic, social, and environmental factors. 2 – 5
Home visiting is 1 strategy to improve maternal-child health outcomes through family education, training, and social support. 6 – 8 Recently, the Health Services and Resources Administration created the Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program, with 1 aim to improve care management for pregnant women at high risk for preterm birth and low birth weight (<2500 g). 9 However, existing studies of home visiting and pregnancy outcomes have yielded inconsistent results, likely in part due to limitations in approach, lack of a theoretical framework specific to pregnancy outcomes, and variation in content and delivery of the intervention. 10 – 12
An important component of home visiting may be “dosage,” or duration of enrollment and intensity of participation. Evidence suggests that benefits of home visiting, measured on a range of outcomes, are affected by extent of exposure. 13 – 15 This may be particularly important for preterm birth, where modifiable risk factors such as nutrition, physical or mental health, and lifestyle behaviors may only be amenable to intervention if exposure begins early and is sustained at a sufficiently high intensity. 11 The goal of our study is to evaluate the effect of dosage of home visiting on pregnancy outcomes by using a regional perinatal data resource containing linked administrative and community-based program data. We hypothesized that, after adjustment for clinical, social, and demographic factors, higher number of prenatal visits in the first and second trimester are associated with a reduced likelihood of adverse pregnancy outcomes.
Study Design and Population
This was a retrospective, cohort study to examine the dosage effect of prenatal home visiting on singleton pregnancy outcomes in a population of at-risk, first-time mothers enrolled in an established, regional home visiting program, Every Child Succeeds (ECS), in southwest Ohio from 2007 to 2010.
ECS is a large community-based, home visiting program managed by Cincinnati Children’s Hospital Medical Center. Eligible mothers must have at least 1 of 4 risk characteristics: unmarried, low income (up to 300% of poverty level, receipt of Medicaid, or reported concerns about finances), <18 years of age, or suboptimal prenatal care. Participants are enrolled during pregnancy or before their child reaches 3 months of age. Home visits are provided by social workers, child development specialists, nurses, or paraprofessionals, starting with weekly or more-frequent visits and tapering to fewer visits as the child ages. ECS agencies in Ohio use the Healthy Families America model of home visiting; program goals are to (1) improve pregnancy outcomes through nutrition education and substance use reduction, (2) support parents in providing children with a safe, nurturing, and stimulating home environment, (3) optimize child health and development, (4) link families to health care and other services, and (5) promote economic self-sufficiency.
Referrals to the program may be self-initiated, or come from clinics, hospitals, and other community sources. To avoid inclusion of women who would not have had time for an intervention to influence their risk of delivering preterm, analyses were restricted to women enrolled before 26 weeks’ gestation. Women with multiple gestation pregnancies were also excluded from analysis because of their higher expected incidence of preterm birth.
Data Sources
ECS data were abstracted from a Web-based data entry system used to collect service provision data and for billing. This system contains detailed information on each participant, including enrollment timing by weeks of gestation, prenatal home visit history, and maternal demographic and psychosocial screening information. 16 Enrolled participants were consented to data being used for the purpose of quality assurance benchmarking and research.
These data were linked to Ohio vital statistics, available from the Ohio Department of Health, and birth-related hospital discharge of both mother and infant, available from the Ohio Hospital Association. Because there is no common unique identifier, record linkage was accomplished by using LINKS (University of Manitoba), an SAS-based probabilistic matching program (SAS Institute, Inc, Cary, NC). Selected variables used for linking included maternal and infant dates of birth, hospital of birth, delivery method, gender, and maternal address. Further details of linkage of data sources is described elsewhere by Hall et al. 17 The resulting data set provides information regarding maternal-child health, including demographics, social factors, pregnancy-related conditions, and infant outcomes. The Ohio Department of Health and Cincinnati Children’s Hospital Medical Center Institutional Review Boards approved this study.
Preterm birth was defined as infant birth before 37 weeks’ gestation; gestational age measures were obtained from vital statistics and represented the best clinical estimates. Because risk factors attributable to preterm birth may differ based on gestational age grouping (ie, 32–34 weeks’ vs 35–36 weeks’ gestation), we also repeated analyses with preterm birth specified as gestational age <35 weeks. 18 Our second key outcome was infant birth weight, also obtained from vital statistics, which was categorized as small for gestational age (SGA) versus appropriate or large for gestational age by using validated growth curves. 19
As a sensitivity analysis, we repeated evaluations by using a combined gestational age estimate from vital statistics rather than the clinical gestational age estimate, since previous studies have demonstrated discordance between these measures and potential unreliability of either one for population-based research. 20 The combined gestational age estimate incorporates the clinical estimate but primarily relies upon a calculated estimate based on maternal report of last menstrual period.
The primary predictor was dosage of prenatal home visiting (ie, the amount of intervention received among enrolled participants). To measure timing of onset, dates of enrollment were extracted from ECS and used to calculate gestational age at enrollment on the basis of the date of birth and gestational age at birth. Intensity of participation was measured as the number of completed prenatal home visits, also extracted from the ECS data system.
Although previous work has demonstrated an association between prenatal home visiting duration and preterm birth, 15 one potential concern may be that duration of prenatal enrollment is tautologically related to length of pregnancy and thus gestational age at delivery. Similarly, total number of completed prenatal home visits may reflect length of pregnancy, thereby limiting the ability to infer causality for preterm birth. To offset this concern, we used number of home visits before 26 weeks’ gestation for the preterm birth analysis, whereas for the SGA analysis we used total number of home visits. These variables were categorized into groupings of visit counts on the basis of reasonable cutoffs for ease of interpretation, as well as on the basis of distribution of the data.
As described by Hall et al, 17 data for maternal covariates were obtained through a combination of linked vital statistics, hospital discharge records, and home visiting data. These included race, ethnicity, payer source, maternal age, employment status, marital status, and education level. In addition to maternal BMI, calculated from vital statistics measures, indicator variables for relevant maternal comorbidities and obstetrical risk factors were constructed by using International Classification of Diseases, Ninth Revision, Clinical Modification codes and vital statistics data. These included chorioamnionitis, previous poor birth outcome (defined as previous fetal loss, stillbirth, or neonatal death), placental abnormalities, cervical abnormalities, hypertension/preeclampsia, anemia, diabetes, oligohydramnios, and premature rupture of membranes. Measures of tobacco, alcohol, and other substance use, as well as maternal living arrangement and frequency of contact with the infant’s father, were also obtained.
In addition to individual-level covariates, we measured the percent of residents living below poverty level by census tract for each participant’s geocoded address by using 5-year estimates from the 2010 American Community Survey, 21 as poverty has been demonstrated to be an important area-level measure associated with a range of health outcomes, including preterm birth. 3 , 22
Statistical Analysis
Preterm birth.
Bivariate analyses by using χ 2 or t tests were used to identify covariates associated with preterm birth. Factors deemed to be empirically or statistically important ( P < .25) were considered and tested in multiple logistic regression analyses by using step-wise multivariable modeling to derive parsimonious models. Models were tested for goodness of fit by using Akaike Information Criterion values and link tests for model specification. Multicollinearity was also assessed, with variance inflation factors for all retained variables < 10. 23
The independent association of home visiting exposure with SGA status was assessed by using a Cox proportional hazards survival model because of differences in timing to the outcome (birth) on the basis of gestational age at delivery. As above, bivariate analyses were used to identify covariates associated with the outcome; factors were then considered and tested in multivariable analyses by using step-wise multivariable modeling. Models were tested for goodness of fit and multicollinearity. Testing for violation of proportional hazards assumption was performed by using Schoenfeld residuals, which were not statistically significant.
All statistical tests were 2-sided, and type I error was controlled at 0.05. Final models were adjusted for clustering by home visiting agency by using robust SEs for cluster-correlated data. Analyses were performed by using Stata 11.0 (Stata Corp, College Station, TX).
From the data set representing 2330 women with linked home visiting records and Ohio birth certificates for the years 2007–2010, we identified 918 prenatally enrolled first-time mothers with a single gestation pregnancy. Of these, 441 enrolled by 26 weeks’ gestation and were included in the final analytic sample. The preterm birth rate among the sample was 10.9%, and 17.9% of infants were born SGA. Sixty-one percent were African American and 32% were white, 98% were unmarried, 53% had not completed high school, mean maternal age was 20 years, and 84% were insured through Medicaid. Mean gestational age at enrollment was 18.9 weeks, and number of total completed prenatal home visits ranged from 1 to 26 visits. As expected, there were fewer visits completed before 26 weeks’ gestation, ranging from 1 to 16.
Bivariate Comparisons
Table 1 depicts comparisons of key predictors and covariates with preterm birth. In bivariate analyses, preterm birth was not significantly associated with gestational age at enrollment or categorized number of home visits before 26 weeks. A higher percentage of women delivering preterm had a history of previous poor pregnancy outcome (25.0% vs 10.7%), hypertension/preeclampsia (27.1% vs 12.0%), and disorders of placentation (4.2% vs 0.5%) compared with women delivering at full term gestations, all P < .05.
Clinical and Demographic Characteristics of Mothers Enrolled in Home Visiting Prenatally With and Without Preterm Birth
As shown in Table 2 , bivariate comparisons demonstrated that women delivering an SGA infant were not significantly different from women without SGA infants in mean gestational age at enrollment or categorized number of total prenatal home visits. A higher percentage of women delivering an SGA infant had a history of cigarette use (46.8% vs 31.5%) and other drug use (19.0% vs 10.8%) compared with women delivering non-SGA infants, P < .05. Mean maternal BMI was significantly higher in the group with SGA infants (25.7 vs 23.9, P < .01).
Clinical and Demographic Characteristics of Mothers Enrolled in Home Visiting Prenatally With and Without SGA infants
Multivariable Analyses
As shown in Table 3 , timing of enrollment in home visiting was not independently associated with preterm birth. However, number of home visits before 26 weeks was statistically significant; compared with the reference group of ≤3 home visits, completion of 8 or more home visits by 26 weeks was associated with an adjusted odds ratio (aOR) 0.38 for preterm birth (95% confidence interval [CI]: 0.16–0.87). This association was robust to re-specification of the outcome as delivery before 35 weeks’ gestation. Several maternal covariates were associated with a significantly increased AOR of preterm birth, including hypertension/preeclampsia (AOR, 2.99 [95% CI: 1.66–5.41]), previous poor pregnancy outcome (2.87 [95% CI: 1.52–5.44]), and placental disorders (6.77 [95% CI: 1.58–29.0]).
Multivariable Logistic Regression of Predictors With Preterm Birth, AORs
Overall models and coefficients for key predictors did not change significantly when combined versus clinical gestational age estimates were used; therefore, these data are not shown.
Table 4 depicts results of the multivariable proportional hazards analysis for SGA. After adjustment for all covariates, receipt of ≥12 prenatal home visits compared with the reference group of 1 to 3 prenatal home visits was significantly associated with a 0.32 hazard ratio (HR) of SGA status (95% CI: 0.15–0.68). This association was not detected for categories with fewer numbers of total prenatal home visits (ie, 4–7 visits or 8–11 visits). Maternal age <18 years was significantly associated with SGA status compared with age >18 years (HR: 1.37 [95% CI: 1.06–1.76]), as was maternal race classified as Other compared with white (HR: 3.06 [95% CI: 1.13–8.25]).
Multivariable Cox Proportional Hazards Analysis of Predictors With SGA Status, Adjusted HRs
Although the effectiveness of home visiting has been demonstrated for many outcomes, including child abuse, infant development, and parenting, the impact of this intervention for pregnancy outcomes is currently not well understood. 6 – 8 , 10 , 11 , 24 Given the importance of preterm birth to pediatric morbidity and health care spending, as well as the investment of federal funding in home visiting through MIECHV, further conceptualization and measurement of prenatal delivery of home visiting is critical to a comprehensive understanding of the utility and potential cost benefits of this intervention. The current study is a retrospective analysis of dosage of home visiting and singleton pregnancy outcomes in a regional population of at-risk, first time mothers. Results demonstrate that a significant reduction in the likelihood of preterm birth and SGA status is associated with receipt of the highest number of prenatal visits compared with women receiving the lowest number of visits.
This study builds on previous work evaluating the impact of ECS on infant outcomes at a population level, in which program enrollment as a dichotomous predictor was not associated with differences in infant gestational age. 25 Although many previous randomized controlled trials and quasi-experimental studies of community-based programs have revealed promise in improving preterm birth and infant birth weight, 26 – 31 several reviews of the existing body of literature have demonstrated an overall lack of consistent evidence to support the effectiveness of prenatal home visiting. 10 , 11 , 24 , 32 , 33 One cause for the overall low percent of positive findings may be lack of attention to dosage of the intervention (ie, the number or duration of home visits per participant). 11 , 15 Given the complexity of biological, genetic, social, and environmental factors influencing preterm birth, any intervention addressing modifiable risks like nutrition or health behaviors would seem to require adequate intensity and length of exposure to be effective. The importance of home visiting dosage has already been shown for other outcome domains, including child behavioral problems and maternal parenting. 13 , 14
Strengths of the current study include minimized selection bias associated with enrollment among an at-risk population by constraining analyses to women enrolled in home visiting prenatally. Furthermore, the sample was restricted to those enrolled before 26 weeks’ gestation to maximize the likelihood that participants had time for the intervention to influence their pregnancy. Rather than focus on total number of visits or duration of prenatal participation, which present a problem of tautology with regards to length of pregnancy and thus preterm birth, we measured only visits before 26 weeks for the preterm birth analysis, which is also consistent with our hypothesis that early intervention at a high intensity is required to address modifiable risk factors for preterm birth. An additional strength is our application of linked data systems to support policy relevant research in a “real world” setting, which may be particularly important given the requirement for evaluation of home visiting within existing, established programs as services are expanded.
There are several limitations related to use of administrative data in this retrospective analysis. Complications and comorbidities identified by using vital statistics and hospital discharge data may be undercoded or overcoded, resulting in a misclassification bias. 34 – 36 Another limitation may be generalizability of findings given the sample size and regional population represented. Although we attempted to maintain parsimonious regression models, the number of preterm cases is small relative to the number of retained covariates. Although the ECS prenatal curriculum provides guidance to home visitors for standardized content on the basis of the week of pregnancy, another limitation of this study is potential variation in the content of home visits across participants in this cohort, which is not included in analyses. Lastly, an important limitation of any observational study is the inability to infer causality from observed associations; differences in maternal risk because of nonrandom assignment into groups of higher and lower dosage of home visiting may in part account for the lack of significant association between visit number and outcomes in bivariate analyses. Although we attempted to minimize bias through study design and inclusion of important covariates in multivariate analyses, the extent to which findings were attributable to unmeasured confounding (ie, maternal motivation or self-efficacy) is unclear. This concern may be partially addressed by further omission of subgroups potentially contributing to bias from the analysis; as an example, when alcohol and other substance users ( n = 64) are omitted, the aOR of preterm birth associated with highest number of prenatal visits before 26 weeks remains statistically significant (0.35 [95% CI 0.19–0.64]).
Conclusions
Given the contribution of birth outcomes to pediatric morbidity and health care spending, as well as the federal investment in home visiting through MIECHV, further conceptualization and measurement of prenatal delivery of home visiting is critical to a comprehensive understanding of the utility and potential cost benefits of this intervention. Current findings support that high dosage of prenatal home visits is associated with reduced odds of preterm birth or SGA status. As programs expand services within at-risk populations, enrollment early in pregnancy and promotion of high levels of engagement in the first and second trimester may be important to achieving measurable benefits of this intervention.
Acknolwedgments
The authors acknowledge David Jones for assisting with the census tract-level data and Dr Louis Muglia, Dr James Greenberg, and Dr Rita Pickler for critical review of the article. We acknowledge the participation and support of the United Way of Greater Cincinnati, Kentucky HANDS, and Ohio Help Me Grow.
Dr Goyal conceptualized and designed the study, performed statistical analysis, and drafted the initial manuscript; Dr Hall coordinated and supervised administrative data collection and data linkages and reviewed and revised the manuscript; Dr Meinzen-Derr assisted with study design, supervised all statistical analysis, and reviewed and revised the manuscript; Dr Kahn assisted with design of the study and interpretation of the data and reviewed and revised the manuscript; Ms Short coordinated data collection for the home visiting program, assisted with interpretation of the data, and critically reviewed the manuscript; Dr Van Ginkel supervised data collection for the home visiting program and critically reviewed the manuscript; Dr Ammerman supervised the conceptualization of the study and designed the study, supervised interpretation of the data, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
Dr Goyal's involvement in this project was supported by the Building Interdisciplinary Research Careers in Women's Health (BIRCWH) program, co-funded by the Office of Research on Women's Health (ORWH) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Award Number 5K12HD051953-07. Dr Hall's and Dr Meinzen-Derr's participation was supported by the Place Outcomes Award from Cincinnati Children's Hospital Medical Center. Dr Ammerman was supported by Grant R01MH087499 from the National Institute of Mental Health (NIMH).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Mental Health, or the National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Goyal’s involvement in this project was supported by the Building Interdisciplinary Research Careers in Women’s Health program, cofunded by the Office of Research on Women’s Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, award number 5K12HD051953-07. Dr Hall’s and Dr Meinzen-Derr’s participation was supported by the Place Outcomes Award from Cincinnati Children’s Hospital Medical Center. Dr Ammerman was supported by grant R01MH087499 from the National Institute of Mental Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article

Treatment Conditions
Main outcomes, statistical models and methods of analysis, cognitive, language, achievement, and executive functioning outcomes, behavioral health, conclusions, acknowledgments, prenatal and infancy nurse home visiting and 18-year outcomes of a randomized trial.
POTENTIAL CONFLICT OF INTEREST: The Prevention Research Center for Family and Child Health, directed by Dr Olds at the University of Colorado School of Medicine, has a contract with the Nurse-Family Partnership (NFP) to conduct research to improve the NFP program and its implementation; this contract covers part of Dr Olds’s salary and part of Mr Knudtson’s salary. Dr Olds and Mr Knudtson were employed by this center at the time the study was conducted. Dr Olds is the founder of NFP and, with the University of Colorado, owns the NFP intellectual property. The University of Colorado receives royalties from governments and organizations outside of the United States that implement NFP and has contracts with those entities to guide the implementation of NFP with quality, but none of the royalties or fees go to Dr Olds personally; they are used to support the Prevention Research Center for Family and Child Health research and implementation guidance. Dr Miller performs economic analyses under contract for the nonprofit Nurse-Family Partnership National Service Office; the other authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: Dr Olds receives personal honoraria and travel expenses from philanthropies and organizations for speaking about the Nurse-Family Partnership and early intervention; the other authors have indicated they have no financial relationships relevant to this article to disclose, beyond those already listed in the Potential Conflict of Interest.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Harriet Kitzman , David L. Olds , Michael D. Knudtson , Robert Cole , Elizabeth Anson , Joyce A. Smith , Diana Fishbein , Ralph DiClemente , Gina Wingood , Angela M. Caliendo , Christian Hopfer , Ted Miller , Gabriella Conti; Prenatal and Infancy Nurse Home Visiting and 18-Year Outcomes of a Randomized Trial. Pediatrics December 2019; 144 (6): e20183876. 10.1542/peds.2018-3876
Download citation file:
- Ris (Zotero)
- Reference Manager
Video Abstract
Given earlier effects found in randomized clinical trials of the Nurse-Family Partnership, we examined whether this program would improve 18-year-old first-born youths' cognition, academic achievement, and behavior and whether effects on cognitive-related outcomes would be greater for youth born to mothers with limited psychological resources (LPR) and on arrests and convictions among females.
We enrolled 742 pregnant, low-income women with no previous live births and randomly assigned them to receive either free transportation for prenatal care plus child development screening and referral (control; n = 514) or prenatal and infant home nurse visit (NV) plus transportation and screening ( n = 228). Assessments were completed on 629 18-year-old first-born offspring to evaluate these primary outcomes: (1) cognitive-related abilities (nonverbal intelligence, receptive language, and math achievement) and (2) behavioral health (internalizing behavioral problems, substance use and abuse, sexually transmitted infections, HIV risk, arrests, convictions, and gang membership).
Compared with control-group counterparts, NV youth born to mothers with LPR had better receptive language (effect size = 0.24; 95% confidence interval [CI]: 0.00 to 0.47; P = .05), math achievement (effect size = 0.38; 95% CI: 0.14 to 0.61; P = .002), and a number of secondary cognitive-related outcomes. NV females, as a trend, had fewer convictions (incidence ratio = 0.47; 95% CI: 0.20 to 1.11; P = .08). There were no intervention effects on other behaviors.
The program improved the cognitive-related skills of 18-year-olds born to mothers with LPR and, as a trend, reduced female convictions but produced no other effects on youth behavioral health.
Two randomized trials of prenatal and infant home visit by nurses found effects on children’s behavioral problems, early adolescent substance use, and among children born to mothers with limited psychological resources, cognitive outcomes. One trial found fewer convictions among females.
This trial extends earlier estimates of intervention impact: compared with control-group counterparts, nurse-visited 18-year-olds born to mothers with limited psychological resources exhibited better cognitive functioning; females, as a trend, had fewer convictions. There were no significant effects on behavioral health.
The potential of early intervention to improve the lives of children born into disadvantaged families has gained considerable attention. 1 , 2 Pregnancy and the early years of life are opportune times to intervene because of significant neuroendocrine changes in mothers, developing fetuses, and young children. 3 , 4 Prenatal and early childhood exposures to toxicants, maltreatment, and stress are thought to amplify one another over time, contributing to compromised life-course development and making this an opportune time to intervene to improve vulnerable children’s development. 5 Our team has been conducting a series of pragmatic randomized clinical trials (RCTs) of a program of prenatal, infant, and toddler home visiting by nurses for low-income mothers and their children known as the Nurse-Family Partnership (NFP). 6 – 20 The current study assesses 629 primarily African American first-born 18-year-old youth whose mothers participated in the second RCT of NFP in Memphis, Tennessee. 11 – 17
Findings from the current trial 11 – 16 and NFP trials conducted earlier in Elmira, New York, 6 – 10 and later in Denver, Colorado, 18 – 20 led us to hypothesize that NFP would improve 18-year-old youth language, cognition, and math achievement and that effects in this broad domain would be most pronounced for youth born to mothers with limited psychological resources (LPR) to cope with adversity: in the lower half of the distribution on an index composed of maternal intellectual functioning, 21 mental health, 22 and sense of mastery 23 plus self-efficacy (mothers’ beliefs about the importance of and her confidence in accomplishing key NFP behavioral objectives) 24 measured at baseline. 11
Given NFP effects on substance use and antisocial behavior through age 15 among youth born to disadvantaged mothers in the Elmira trial 9 and substance-use and internalizing disorders in the current trial at age 12, 15 we hypothesized that the program would reduce 18-year-olds’ internalizing disorders, substance use, and abuse disorders. In light of intervention effects on the number of lifetime sex partners through age 15 among youth born to disadvantaged mothers in Elmira 9 and anticipated effects on substance abuse disorders in the current trial, we hypothesized that nurse visited (NV) 18-year-olds would have fewer pregnancies and births and a lower risk for HIV. Given NFP effects on arrests, convictions, and violations of probation among 15-year-olds born to disadvantaged mothers in the Elmira trial 9 and substance use at age 12 in the current trial, 15 we hypothesized that the program would reduce rates of gang membership, arrests, and convictions among 18-year-olds.
Before analysis of intervention-control differences, we found that program effects on arrests and convictions in Elmira were limited to females through age 19, 10 leading us to hypothesize the presence of corresponding female effects in Memphis. Also, given the presence of little meaningful variation in neighborhood disadvantage (2.4 SDs above the national mean 25 ), we eliminated, before analysis of intervention effects, a hypothesis that program effects would be greater among youth whose mothers lived in the most distressed neighborhoods at registration.
The basic features of this study have been reported earlier. 11 We conducted this RCT in a public system of obstetric and pediatric care in Memphis, Tennessee, with registration of the original sample completed between June 1990 and August 1991. Given that program effects were more pronounced for mothers and children from more disadvantaged families in the preceding trial, 6 – 10 we focused sampling in Memphis on those with overlapping sociodemographic risks. We enrolled women <29 weeks’ gestation with no previous live births and at least 2 sociodemographic risks (unmarried, <12 years of education, or unemployed). Ninety-two percent of the women were African American, and at enrollment, 98% were unmarried, 64% were <18 years of age, and 85% were from households with incomes below the federal poverty guidelines. For the current follow-up, participating mothers, other caregivers, and youth completed informed consent procedures approved by the University of Rochester Institutional Review Board.
Table 1 summarizes the Consolidated Standards of Reporting Trials information. Eighty-eight percent ( n = 1138) of 1289 eligible pregnant women who were offered participation completed informed consent and were randomly assigned to 1 of 4 treatment conditions following a procedure that concealed assignment from individuals involved in gathering participant data. 11 We assigned 742 participants to 2 treatment conditions created to estimate program effects on postnatal outcomes: 514 to Treatment 2 (control) and 228 to Treatment 4 (NV), both described below. Sample size and assignment ratios were derived from statistical power calculations in the original phase of the trial. 11 Table 1 shows those lost to follow-up because of miscarriage or child death, maternal or child refusal to participate at earlier phases, and the number evaluated with youth assessments and maternal and/or other-custodian interviews at youth age 18.
Consolidated Standards of Reporting Trials Information for Youth Enrolled in the Trial Through 18-Year Follow-up
There were 1290 subjects eligible to participate; 151 declined participation, and 1138 were randomly assigned. CBCL, Child Behavior Checklist; —, not applicable.
Treatment 1: prenatal transportation.
Treatment 2: prenatal transportation plus developmental screening and referral.
Treatment 3: prenatal transportation plus developmental screening and referral and prenatal nurse home visits.
Treatment 4: prenatal transportation plus developmental screening and referral and prenatal and infant and/or toddler nurse home visits.
Note that 1 mother was enrolled and randomly assigned twice by mistake after a miscarriage. We included her only once, with her original assignment, in the control group.
Some outcomes reported in Tables 4 and 5 show higher numbers than indicated in this table because they include repeated estimates of outcomes from earlier phases of follow-up, as indicated by “all” under “age at assessment” in those tables.
Some youth were unable or unwilling to complete the standardized psychological or achievement assessments or to provide urine to screen for STIs or substances, reducing the numbers shown in Tables 4 and 5 .
Youth arrests were derived from a detailed examination of self-report, maternal, and other-caregiver report, synthesizing data from all 3 data sources (when available); this shows the number of cases for which data were gathered from maternal and/or other-caregiver report. Estimates of arrest-related outcomes were made even if maternal and other-caregiver reports were unavailable.
Youth CBCL externalizing and total behavioral problems (borderline or clinical) were derived from a combination of youth self-report and either maternal or other-caregiver report. Maternal report was given priority over other-caregiver report.
Some youth were unable or refused to provide urine for substance-use or STI screening. One sample was unusable for STI screening.
Interviews for this follow-up were conducted between October 2008 and September 2014, and reviews of school records were conducted by December 2015 by staff masked to treatment assignment. Most assessments were conducted after youth 18th birthdays (mean age 18.67 years; SD = 0.95; range: 17.5–23.9). Repeated measures of some outcomes over time increased the numbers and are noted by “all” under the column "Child Age ge at Assessment” in Tables 3 and 4 .
Interviews were completed with 629 of the 669 available youth. Interviews were conducted with mothers and other caregivers to augment youth report of arrest outcomes ( n = 621) and externalizing and total behavior problems ( n = 615) and to determine Supplemental Social Security Income (SSI) for disability ( n = 619). High school graduation records were collected for 619 youth, and urine was collected for 606 youth.
Women in the control group ( n = 514) were provided with free transportation for scheduled prenatal care plus developmental screening and referral for children at 6, 12, and 24 months of age. Women in the NV condition ( n = 228) were provided with the same services as the control group plus prenatal and infancy home visitation through age 2.
NFP was designed to (1) improve pregnancy outcomes by promoting women’s prenatal health behaviors, (2) improve children’s health and development by promoting parents’ care of their children, and (3) enhance parents’ health and life course by encouraging women to plan the timing of subsequent pregnancies, complete their educations, and find work. Nurses linked families with needed services and, when possible, involved other family members (especially children’s fathers and grandmothers). 5 Program protocols were grounded in developmental epidemiology and theories of human attachment, human ecology, and self-efficacy and adjusted to families’ individual needs. 5
The program was implemented by the Memphis and Shelby County Health Department during a nursing shortage, leading to nurse turnover for 37% of the families. 11 Nurses carried a maximum caseload of 25 families each and relied on detailed visit-by-visit guidelines structured around 62 home visits. It is impossible for nurses to complete 62 visits for all families, and most families do not need this level of service. Nurses used their clinical judgment to adjust dosage and visit content, as well as telephone communications when in-person visits were not possible, to address individual needs revealed in the conduct of visits.
All families were scheduled to receive 4 weekly visits at the beginning of the program to facilitate nurses’ and mothers’ getting to know one another as early in the pregnancy as possible and to develop a trusting relationship founded on nurses’ understanding of mothers’ aspirations and concerns about their prenatal health, the developing fetus, birth, and the challenges of caring for a newborn. Newborn health and mother’s adjustment to caregiving were critical factors in nurses’ decisions about visit dose and content. Nurses recorded features of program implementation on every attempted and completed visit. 5 , 26 , 27
Overall, nurses completed a mean of 7 home visits during pregnancy and 26 visits during the first 2 years postpartum. 11 , 27 Mothers in the lowest quartile of psychological resources (PR) at baseline received the highest number of home visits (mean = 37.67; SE = 2.38), those in the middle 2 quartiles had the fewest (mean = 32.02; SE = 1.68), and those in the highest quartile of PR received an intermediate number of visits (mean = 34.26; SE = 2.38).
Table 2 shows that outcomes were divided into 2 broad categories: (1) cognitive-related outcomes (nonverbal intelligence, language, math achievement, sustained attention, working memory, emotion recognition, risky decision-making, SSI for disability, high school graduation, and graduation with honors) and (2) behavioral health (mental health [internalizing, externalizing, and total behavioral problems], substance use and abuse, sexually transmitted infections [STIs], HIV risk, arrests and convictions, and gang membership). Within these broad categories, we separated primary from secondary outcomes. Table 2 shows the specific measures used and bases for hypotheses. Primary outcomes were predicted from previous intervention effects on the same measures or constructs in earlier phases of the current trial or other NFP trials and, for some outcomes, from effects found at earlier phases. Secondary outcomes were selected on the basis of their epidemiological and theoretical associations with earlier effects in the Elmira, Memphis, or Denver trials. 5 – 9 , 11 – 16 , 18 – 20 We included 2 exploratory outcomes: high school graduation with honors and mother and/or caregiver report of youth receipt of SSI for disability.
Outcome Domains, Variables Measured, and Bases for Hypotheses
CIDI-SAM, Composite International Disease Interview–Substance Abuse Model; WAIS, Wechsler Adult Intelligence Scale; —, not applicable.
We show the bases for hypotheses in 3 categories: (1) an earlier effect on the same specific measure or construct in an earlier phase of the trial, (2) an effect on the same measure or construct in other trials, and (3) effects in earlier phases or trials that predict the current outcomes on theoretical or epidemiological grounds. When the prediction was made from the same measure, the basis for the hypothesis is shown on the same row; otherwise, it is shown on the construct row. Note that those outcomes hypothesized to be greater for particular subgroups are shown in the last column.
Outcome domain. Specific variables assessed are shown under each outcome domain. Outcomes were selected on the basis of their being affected in earlier phases of this trial or the preceding trial or on theoretical and epidemiological grounds, with attention paid to those aspects of functioning that are of clinical or public health importance and that could be assessed without overburdening respondents.
Subgroup defined by youths' mothers at registration 11 falling into the lower half of the distribution of an index composed of the average z scores of women’s intellectual functioning, 21 mental health, 22 and sense of mastery 23 plus self-efficacy (based on mothers’ confidence in their ability to accomplish key NFP behavioral objectives). 24
The intervention effect on nonverbal intelligence at age 6 was a trend overall and for the LPR group, derived from the Kaufman Assessment Battery for Children Mental Processing Composite. 29 The analysis of the whole-scale Kaufman Assessment Battery for Children Mental Processing Composite was significantly different for the treatment-control contrast, both overall and for the LPR group at age 6. 13 The nonverbal subscale trend was not reported in the earlier publication. 13 The Kaufman Brief Intelligence Test 2 administered at age 18 is a shortened version of intellectual functioning based on the full-scale Kaufman Assessment Battery for Children.
Exploratory outcome. Graduating with honors was not part of the original measurement design per se. The original plan called for gathering school records of grade point averages and disciplinary records, which were incomplete, leading us to eliminate them as part of the final measurement design. We discovered, however, that states sent information on graduation with honors, which aligns with the original measurement design and thus is included in this report. Note that all states to where participants moved record graduating with honors, with the exception of Mississippi. Seventeen participants graduated from Mississippi schools (10 control; 7 NV); they are included in the analysis as not having graduated with honors.
Exploratory outcome. SSI (disability) was based on parent and/or caregiver report and not included in the original measurement design. The question is relevant to this report and thus is included here.
Data analyses are reported on all cases randomized insofar as outcome data were available. The analysis adhered to a statistical analysis plan established before examination of data from the intervention group.
The primary statistical model for cognitive-related outcomes consisted of a 2-level treatment factor (control versus NV) and a 2-level factor reflecting mothers’ PR (above versus below the sample median), focusing on treatment differences for the LPR group, in models that included 3 covariates (household poverty index, maternal attitudes predictive of child abuse [CAA], 43 and youth sex). The first 2 covariates, consistent predictors of a range of outcomes, adjusted for treatment nonequivalence at registration; the third was added because of its strong relationship with some outcomes. The household poverty index incorporates 3 variables: discretionary household income, housing density, and head-of-household employment. For emotion-recognition analyses, we added age-18 nonverbal intelligence to the model to reduce the likelihood that intervention effects would simply reflect differences in intelligence.
For arrest and conviction outcomes, we examined NV-control differences in a model that included sex as a classification factor, examining treatment differences separately for females and males, in models that included 3 covariates: maternal PR, household poverty, and CAA. 43
Given that rates of pregnancies, births, and STI outcomes were operationalized differently for males and females, we examined NV-control differences separately for males and females and included 3 covariates: maternal PR, household poverty, and CAA. 43
For analysis of HIV risk, we examined NV-control differences in a model that included covariates for maternal PR, youth sex, youth age at assessment, household poverty, and CAA. 43
For all remaining behavioral health outcomes, we examined NV-control differences in models that included covariates for maternal PR, youth sex, household poverty, and CAA. 43
For continuous and dichotomous outcomes on which we had repeated assessments for each child over time, we analyzed outcomes using generalized mixed models that included, in addition to variables from the primary model, children as levels of a random factor, a fixed repeated-measures classification factor for time of assessment, and all interactions of time with the other fixed classification factors.
Continuous dependent variables were analyzed in the general linear model, and dichotomous outcomes were analyzed in the logistic linear model. For low-frequency count outcomes, we analyzed data in generalized linear models with negative binomial error assumptions. We examined low-frequency outcomes with rerandomization tests to determine model fit 44 and truncated 1 outlier for the count-of-convictions outcome. Substance-use disorders and timing to first pregnancy and birth were analyzed over time by using Cox proportional-hazards models. We present survival rates at age 18 along with hazard ratios.
Supplemental Tables 6 and 7 show estimates of NV-control differences without covariate adjustments.
The NV and control groups were similar on background characteristics for participants for whom 18-year follow-up assessments were conducted ( Table 3 ), with these exceptions: at intake, NV women, compared with controls, lived in households with less discretionary income, higher person-per-room density, higher scores on a household poverty index, and higher scores on CAA. 43
Background Characteristics at Randomization of Those Participants for Whom 18-Year Assessments Were Completed
T2, prenatal transportation plus developmental screening and referral.; T4, prenatal transportation plus developmental screening and referral and prenatal and infant and/or toddler nurse home visits.
Subgroup defined by youths' mothers falling into the lower half of the distribution for PR (LPR) described in the following footnote.
Average z scores of women’s intellectual functioning, 21 mental health, 22 and sense of mastery 23 plus self-efficacy 24 (mastery and self-efficacy measures were standardized and averaged; self-efficacy is based on participants’ beliefs about the importance of and confidence in accomplishing key NFP behavioral objectives).
Standardized to sample: mean = 100; SD = 10.
Annual household discretionary income is based on income subsistence standards for Medicaid eligibility, reported household income, and number of individuals in the household at registration.
Persons per room.
Locally developed scale that assesses degree to which the mother experiences conflict in her relationship with this person.
Adult-Adolescent Parenting Inventory. 43
Average z scores of household discretionary income, housing density, and whether the head of household was employed.
Average of variables calculated in SD units from the national means of components that comprise the index of concentrated social disadvantage (percentage of block group residents: [1] below federal poverty level, [2] receiving public assistance, [3] unemployed, [4] headed by single women, [5] age <18, and [6] African American). 25
Table 4 summarizes estimates of youth functioning in the cognitive, language, achievement, and executive functioning domains for the sample as a whole and for youth born to mothers with LPR. With the exception of NV youth having higher rates of graduation with honors (adjusted odds ratio [aOR] = 2.12; 95% confidence interval [CI]: 1.09 to 4.13; P = .028) and trends ( P < .10) of NV youth having higher math scores and better emotion recognition, there were no intervention-control differences for the sample as a whole. NV children born to mothers with LPR, on the other hand, had better receptive language (effect size [ES] = 0.24; 95% CI: 0.00 to 0.47; P = .048) and math achievement (ES = 0.38; 95% CI = 0.14 to 0.61; P = .002) at age 18. For both of these outcomes, there were longitudinal effects over time. There were no intervention-control differences in nonverbal intelligence.
Estimates of Cognitive, Language, Academic, and Executive Functioning Outcomes and SSI Benefit Received Among 18-Year-Old Youth in the Intervention and Control Conditions
The estimates of intervention-control differences averaged over all other fixed classification variables, including those within subjects, and the same treatment effect were restricted to the group defined by LPR. This table shows the least-squares means at 18 y and repeated measures over time (labeled “all” under “age at assessment”), which also are averaged over other fixed classification effects. For estimates of treatment effects based on repeated measures, we assumed an error structure with different variances at each time for a given child and a different covariance between pairs of times within each child. These were assumed to be the same for all children, and covariance between children was assumed to be negligible. Contrasts at specific, earlier time points are presented in earlier publications. 11 – 16 LS, least squares; T2, prenatal transportation plus developmental screening and referral.; T4, prenatal transportation plus developmental screening and referral and prenatal and infant and/or toddler nurse home visits.
Age 18 assessment denoted by 18 y; repeated-measures assessment denoted by “all.” The exact ages aggregated for repeated-measures estimates are given in footnotes.
Expressed in SD units.
Subgroup defined by youth mothers falling into the lower half of the distribution for PR (LPR).
Ages 6 and 18.
Ages 6, 12, and 18.
Ages 12 and 18.
Exploratory outcome.
P < .10; ** P < .05; *** P < .01.
NV children born to mothers with LPR also had better working memories (ES = 0.23; 95% CI = 0.01 to 0.46; P = .045) and emotion-recognition abilities (ES = 0.22; 95% CI: 0.01 to 0.44; P = .040), lower SSI for disability (aOR = 0.33; 95% CI: 0.13 to 0.84; P = .011), and higher rates of high school graduation with honors (aOR = 3.34; 95% CI: 1.19 to 9.34; P = .022) than their control-group counterparts.
There were no intervention-control differences in children’s sustained attention, risky decision-making, or high school graduation.
Table 5 shows that NV females, as a trend, had fewer criminal convictions than control females (incidence ratio [IR] = 0.47; 95% CI 0.20 to 1.11; P = .080). There were no intervention-control differences in internalizing, externalizing, or total behavioral problems or in substance use or substance use disorders. There was a marginally significant difference for NV males, compared with control males, to report more convictions for interpersonal violence (IR = 2.15; 95% CI 0.90 to 5.27; P = .082; data not shown). There were no overall NV-control differences in STIs, timing to first pregnancy, timing to first live birth, HIV risk, gang participation, counts of arrests, convictions, and arrests or convictions for interpersonal violence.
Estimates of Youth Substance-Use Disorders, Drug or Alcohol Use, STIs, Pregnancies, Births, Behavioral Problems, Arrests, Convictions, and Gang Activity
The estimates of intervention-control differences averaged over all other fixed classification variables, including those within subjects, and the same treatment effect was restricted to the group defined by females for arrest and conviction outcomes. This table shows the least-squares means at 18 y and repeated measures over time, which also are averaged over other fixed classification effects. For estimates of treatment effects based on repeated measures (labeled “all” under “age at assessment”), we assumed an error structure with different variances at each time for a given child and different covariance between pairs of times within each child. These were assumed to be the same for all children, and covariance between children was assumed to be negligible. Contrasts at specific, earlier time points are presented in earlier publications. 11 – 16 HR, hazards ratio; LS, least squares; SR, self-report; T2, prenatal transportation plus developmental screening and referral; T4, prenatal transportation plus developmental screening and referral and prenatal and infant and/or toddler nurse home visits.
Arrest-related outcomes were based on self-report combined with maternal and other-caregiver report (when available).
Survival rate at age 18 from Cox proportional hazard model.
Based on both self-report for all substances and urine assays for specific substances: phencyclidine, benzodiazepines, cocaine, amphetamines, tetrahydrocannabinol, opiates, and barbiturates.
Internalizing problems were based on youth self-report at ages 12 and 18 and maternal and/or other-caregiver report at child age 6, indicated by values exceeding the borderline or clinical threshold.
Externalizing and total problems were based on reports in which mothers and/or other caregivers (age 6); mothers and/or other caregivers, teachers, and children (2 of 3 at age 12); and youth and mothers and/or other caregivers (age 18) reported scores that exceeded the borderline or clinical threshold.
P < .10.
There were no overall intervention-control differences for any of the behavioral health outcomes, but the program improved the receptive language and math achievement of 18-year-olds born to mothers with LPR and, as a trend, reduced convictions among females. In addition, NV youth graduated with honors more frequently, and those born to mothers with LPR, compared with control-group counterparts, had better working memories and emotion-recognition skills and fewer disabilities leading to receipt of SSI. High rates of sample retention increase the validity of these findings.
The program effect on cognitive-related outcomes was, with the exception of graduation with honors, limited to youth born to mothers with LPR, conditional effects consistent with earlier phases of this trial, 11 – 15 and a subsequent trial. 18 – 20 Most of these effects, except for the twofold increase in graduation with honors overall and threefold reduction in SSI for disability in the LPR group, are small by conventional standards 45 but important because they reflect different aspects of cognition, disability, and academic success relevant to adult functioning. Moreover, most of these outcomes are based on directly measured abilities.
Program effects on emotion-recognition abilities and working memory, although not examined in other NFP trials, are consistent with a reduction in child maltreatment 46 , 47 and earlier program effects on maltreatment-related outcomes. 11 , 13 , 17 By age 2, for example, control children, compared with those visited by nurses, were hospitalized for fewer days for injuries and ingestions 11 ; all admissions for fractures and/or head trauma occurred in control infants born to mothers with LPR. 5 , 11 Control children born to mothers with LPR were less communicative and responsive to their mothers than those visited by nurses through 24 months 11 ; and through age 18, they exhibited more compromised development and achievement. 13 , 15 All preventable child mortality through age 20 occurred in the control group. 17
The improvements in cognitive outcomes and reductions in disability in the LPR group at age 18 suggest that the intervention may lead to additional functional and societal savings for this group, including possible reductions in Alzheimer disease and related disorders, given their relationship with adolescent cognitive functioning. 48 , 49
In interpreting the more pronounced program effect on the cognitive-related outcomes of children born to mothers with LPR, it is important to note that nurses visited the most vulnerable mothers more frequently, a consistent feature of NFP program design beginning with the Elmira trial. 26 Moreover, children born to mothers with LPR had greater room for improvement.
Note that families were not randomly assigned to different visitation schedules, so discerning the role of visit patterns on outcomes is challenging. In exploratory latent class analyses of home visits in the current trial, 3 patterns were uncovered: low attendance (33% of those visited), high attendance (48%), and increasing attendance (18%). Those in the low-visit group had the highest educations at baseline; those in the increasing group had low education, the lowest number of prenatal visits, and high rates of preterm delivery; and those in the high-visit group also had low education at baseline. These findings highlight the role that mothers, in addition to nurses, play in shaping visit attendance patterns and the methodologic challenges involved in estimating intervention effects for those with different visitation patterns. 27
In using the visit patterns found here to guide community replication, 5 it is important to emphasize that the dosage metric that the NFP is designed to achieve is the one actually delivered in the original RCTs and that nurses adjusted visit frequency and content in an effort to ensure that they address specific risks and guide responsive caregiving in the most vulnerable subgroups.
The program effect on convictions among females, although a trend, is consistent with a corresponding finding in the Elmira trial, 10 reduced physical aggression among females at age 2 in the current trial, 50 and intervention effects on trajectories of externalizing problems in the subsequent Denver trial among females, but not males, at ages 2, 4, 6, and 9. 51 These female-limited beneficial effects may be connected to females’ particular susceptibility to the effects of prenatal stress on androgen activity during gestation 52 and hormone-dependent endpoints, including conduct disorder. 53 Moreover, females, compared with males, are particularly susceptible to the effects of harsh parenting on health, 54 , 55 including the development of aggression. 56
There were no beneficial intervention effects in the current trial on 18-year-olds’ substance-use disorders, substance use, or internalizing disorders despite significant intervention effects in these domains at age 12 in the current trial 15 and on substance use, arrests, and convictions through age 15 in the Elmira trial. 9 The trend for NV males to report higher rates of conviction for interpersonal violence was not predicted. The absence of overall beneficial intervention effects on antisocial behavior at the end of adolescence, especially among males, is consistent with age-19 findings in the Elmira trial. 10 There are at least 2 possible explanations for this pattern of results.
The first is that NFP’s promotion of sensitive, responsive care and avoidance of harsh treatment may have decreased parents’ attention to setting effective limits, especially among noncompliant males. 56 The increase in NV males’ self-reported convictions for interpersonal violence found here, although not hypothesized, suggests that greater attention may be needed to address effective limit setting in NFP and to link this program to effective toddler and preschool parenting interventions. 57 – 60
Second, the nearly normative rise in male adolescent–limited antisocial behavior not linked to maltreatment or early adversity 61 may mask intervention effects on life-course–persistent antisocial behavior linked to early maltreatment that may become evident once adolescents assume adult roles. Note, however, that adolescents who become ensnared in substance abuse and criminal activity are at risk for long-term criminal involvement. 61 – 63
The current report has limitations. The first is that nearly all of the behavioral health findings were based on self-report, and some evidence suggests that NV women become more accurate reporters of socially undesirable behavior, such as smoking. 6 Although a case might also be made that NV youth were more attentive listeners and reporters (given program effects on verbal working memory), measurement of STIs and use of substances included urine assays, so this form of treatment-related report bias does not account for the absence of an intervention effect for these outcomes.
Second, we included 2 exploratory outcomes (high school graduation with honors and SSI for disability) that were not part of the original measurement design, so these findings need to be treated with caution.
Third, the age range for completing 18-year assessments was larger than anticipated but not different by treatment. Adjusting for youth age at assessment does not alter the findings (data not shown).
The fourth limitation is that the number of outcomes analyzed raises challenges with multiple comparisons. We have not adjusted for multiple comparisons in NFP trials. 64 – 67 We have focused instead on determining if findings replicate with different populations living in different contexts in separate trials. The long-term program effect on cognitive-related outcomes through the end of adolescence has not yet been tested in other trials, so particular caution is warranted in interpreting these outcomes.
This study found enduring program effects on the cognitive functioning of youth born to the mothers least capable of coping with the adversities that come with living in poverty and a trend for reduced convictions among females but no effects on other adolescent health behavior.
The current phase of this research was supported by the National Institute on Drug Abuse (1R01DA021624). Mr Knudtson had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the analysis. We thank Evelyn Collins for tracing and engaging the study participants and managing the Memphis study office since 1991, Benjamin Jutson (University of Colorado Anschutz Medical Campus) for helping prepare this article, and Wendy Gehring (University of Colorado Anschutz Medical Campus) for her help with data management. Evelyn Collins, Benjamin Jutson, and Wendy Gehring received compensation from research grants for their work.
Deidentified individual participant data (including data dictionaries) will be made available in addition to study protocols, the statistical analysis plan, and the informed consent form. The data will be made available on publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal. Please contact Michael Knudtson, the study biostatistician, at [email protected] or 303-724-3199 for additional details.
Dr Olds conceptualized and designed the study, drafted the manuscript, and supervised the study; Dr Kitzman conceptualized and designed the study, obtained funding, and supervised the study; Dr Cole conceptualized and designed the study and obtained funding; Mr Knudtson acquired data and performed statistical analysis on the data; Dr Smith and Ms Anson acquired data; Drs Fishbein, DiClemente, Wingood, Caliendo, Hopfer, and Miller conceptualized and designed the study; and all authors analyzed and interpreted data, critically revised the manuscript for important intellectual content, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00708695).
FUNDING: Supported by the National Institutes of Health (research grant R01DA021624). Funded by the National Institutes of Health (NIH).
COMPANION PAPER: Companions to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-2606 and www.pediatrics.org/cgi/doi/10.1542/peds.2019-3889 .
adjusted odds ratio
maternal attitudes predictive of child abuse
confidence interval
effect size
incidence ratio
limited psychological resources
Nurse-Family Partnership
nurse visit
psychological resources
randomized clinical trial
Supplemental Social Security Income
sexually transmitted infection
Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Pregnancy Checklist
Be prepared for the big day with this pregnancy to-do list by trimester and month.
This article is based on reporting that features expert sources.
With all the logistics that arise with planning for conception and pregnancy, it’s no surprise that the 40-week-long endeavor brings out many challenges.
Whether you’re hoping for a positive pregnancy test in the near future or already have a baby on the way, here’s a list of useful tips to help with how to prepare for pregnancy.
First Trimester Pregnancy Checklist

Getty Images
During the first trimester, you’ll experience hormonal changes as your body demonstrates the earliest signs of pregnancy.
You may not know you’re pregnant during the first month of pregnancy. The first probable signs of pregnancy may appear around 12 to 15 days after ovulation at the earliest. This is when levels of human chorionic gonadotropin (hCG), a hormone produced by the placenta, are high enough to become detectable on a pregnancy test .
At this time, you may experience other presumptive signs of pregnancy, such as:
- Sore breasts
- A missed period
- Nausea and vomiting
During the first month, check a few early pregnancy tasks off your list, including:
- Choose your pregnancy and birth provider, like an OB-GYN, midwife or family medicine OB provider
- Select which hospital you plan to give birth at, if your provider has delivery privileges at multiple locations
- Schedule your initial prenatal appointment
- Treat any comorbid conditions and review your current medications, as some may need to be changed during pregnancy
Dr. Kecia Gaither, a double board-certified OB-GYN and maternal-fetal medicine provider, suggests treating conditions like:
- Thyroid disease
- Hypertension
“Comorbid conditions, especially uncontrolled diabetes, can significantly increase the risk of congenital abnormalities,” explains Gaither, who also serves as director of perinatal services and maternal-fetal medicine at New York City Health + Hospitals, Lincoln in the Bronx.
Congratulations! Month two is when most women discover their pregnancies.
As soon as you learn you're pregnant, it’s important to stop smoking , drinking or using drugs. Talk with your medical provider about which prescription medications you may need to start, stop or change at this time.
You will also likely begin taking supplements under the direction of your medical provider. Gaither emphasizes the importance of optimizing your pregnancy meal plan and maintaining healthy iron and folate levels for optimal fetal development.
This is because key fetal development occurs during month two, such as:
- Development of the neural tube, which will later become organs in the nervous system, like the brain and spinal cord
- Digestive tract development
- Bone formation
Month three
Month three is often an exciting time in pregnancy, when most people have the first chance to hear the baby’s heart rate. The heart rate may be detectable as early as six weeks, but most initial prenatal appointments occur between eight and 12 weeks.
By this point, you may already be experiencing morning sickness, which is nausea or vomiting, most commonly during the first three months of pregnancy.
To combat these symptoms, try:
- Eating small, frequent meals
- Staying hydrated
- Eating a small snack, like a few crackers, before getting out of bed
While morning sickness is common, reach out to your provider if you experience the following:
- Nausea or vomiting that is preventing you from your daily activities
- Inability to stay hydrated
- Feeling faint, dizzy or confused due to your symptoms
- Vomiting multiple times a day, unrelieved by home care
You may need a hydration infusion to keep you hydrated, or your provider may prescribe medications to combat your symptoms.
Second Trimester Checklist
By the second trimester, the reality of preparing for a baby will start to set in. During this trimester, the early stages of nesting – a drive to prepare your home and lifestyle to accommodate your new addition – may begin.
Around week 10, you’ll have an opportunity to perform noninvasive prenatal genetic testing (NIPT), which uses the mother's blood to screen for chromosome balance and genetic conditions, such as Down syndrome.
By this time your pregnancy may also start to show. If you haven’t already, make sure to add some maternity and loose-fitting clothing to your wardrobe.
Dr. Andrea Braden, a board-certified OB-GYN and lactation consultant, suggests not to wait on purchasing new bras.
“Your breast size starts to increase during pregnancy and for preparation for nursing after," she explains. "Typically, you'll need to buy a new bra as it is, so I would say go ahead and buy bras that have the dual function of being a pregnancy bra in a nursing bra.”
Make sure that by month five, you have a stable exercise routine or movement plan to ensure a healthy pregnancy.
According to the American College of Obstetrics and Gynecology, exercise during pregnancy is essential to:
- Reduce aches and pains
- Relieve constipation
- Decrease the risk of pregnancy complications
Month five is also when you may feel some of the first signs of fetal movement.
Month six is a great opportunity to start the first stages of nesting.
Consider the following nesting activities:
- Planning baby purchases or creating a baby registry
- Planning for potential projects around the house or in the nursery
- If you are working, start to consider how you will handle medical leave and time off to recover after birth and bond with your baby
Third Trimester Checklist
You’re in the final stretch! The third trimester is a great time to finalize your plans and preferences for labor and delivery.
Month seven
Taking a hospital birth class? Best to take it in the third trimester so your memory is fresh, explains Kristin Revere, the owner and founder of Gold Coast Doulas in Grand Rapids, Michigan. If you’re opting for a birth without an epidural, she explains you may consider taking birth classes like hypnobirthing or Lamaze as early as six weeks into pregnancy if you want to get a head start. This will help you mentally prepare to cope with labor pain.
Since you're starting your third trimester, it's a good idea to start preparing for your baby to enter the world.
- Choose your baby's pediatrician .
- Purchase a car seat and have it inspected and properly installed.
- Build a crib or bassinet for the nursery.
Month eight
By month eight, you may be experiencing significant pregnancy-related aches and pains or having trouble sleeping. Ashley Mareko, surrogate program director at Surrogate First, says she used acupuncture and chiropractic services throughout her pregnancy but began going once a week in her third trimester.
Many pregnant women, like Mareko, share anecdotal evidence of acupuncture and chiropractic services helping with reducing pregnancy and labor pain or assisting with labor induction. Researchers acknowledge that the body of evidence supporting acupuncture is limited, but ACOG does not discourage acupuncture or acupressure use in pregnancy. The American Pregnancy Association shares that there are no major concerns with chiropractic care during pregnancy.
At the beginning of month nine, it’s helpful to start planning for birth and the postpartum period.
Here are a few tips:
- Cook some make-ahead freezer meals for nutritious, easy meals after birth.
- Start packing your hospital bag for delivery , just in case the baby comes a few weeks early.
- Finalize your birth plan, and ask the hospital about any pertinent birth or visitation policies.
Bottom Line
The course of your pregnancy will bring new challenges and learning experiences, and no two pregnancies are exactly the same. Consult with your pregnancy provider to get pregnancy advice tailored to your health and wellness.
Antidepressants During Pregnancy
Payton Sy June 1, 2023

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Braden is a board-certified OB-GYN based in Atlanta and a breastfeeding medicine specialist at Lybbie, a lactation innovation company.
Gaither is a double board-certified OB-GYN and maternal fetal medicine provider. She is also the director of perinatal services and maternal-fetal medicine at New York City Health and Hospitals, Lincoln in the Bronx.
Mareko is the surrogate program director at SurrogateFirst, a surrogacy matching service. She is based in Los Angeles.
Revere is the founder of Gold Coast Doulas in Grand Rapids, Michigan.
Tags: pregnancy , patient advice
Most Popular
Patient Advice

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
Early pregnancy signs.
Vanessa Caceres May 17, 2024
Prostate Cancer: Questions to Ask
Ruben Castaneda and Payton Sy May 16, 2024

Does Medicare Cover the RSV Vaccine?
Paul Wynn May 16, 2024
5 Types of Primary Care Doctors
Elaine K. Howley May 15, 2024
How to Tell You Have a Hernia?
Claire Wolters May 14, 2024

How to Treat Seasonal Allergies
Shanley Chien May 13, 2024

Questions to Ask About Diabetes
Toby Smithson and Elaine K. Howley May 13, 2024

ER, Urgent Care or Primary Physician?
Elaine K. Howley May 10, 2024

IUI vs. IVF
Christine Comizio May 9, 2024

Navigating Insurance and Costs at ASCs
Paul Wynn May 9, 2024


An official website of the United States government
Here’s how you know
The .gov means it’s official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
You’re not alone: 1-833-TLC-MAMA
- Programs & Impact
- National Maternal Mental Health Hotline
You’re not alone
Pregnant or just had a baby? The National Maternal Mental Health Hotline is free, confidential, and here to help, 24/7.
1-833-TLC-MAMA
We’re here for you
The Hotline is free, confidential, and available 24/7 in English and Spanish.

Contact the Hotline by texting or calling.

You’ll get a response quickly.

A trained counselor will listen and help.
Our trained Hotline counselors can:
Listen to what you’re going through
Connect you with local support groups and organizations
Refer you to other health care professionals if you need more care

Professional counselors answer Hotline calls and texts. They may be licensed health care professionals, certified educators, or specialists.
New parents: you're not alone

I suddenly don’t feel like I’m drowning. I’m going to be okay. I hope people understand that it does help.
Learn more about maternal mental health.

In 2023, counselors provided emotional support, resources, and referrals to tens of thousands of people.
Get more Hotline data.
You can get help right now
Reach out anytime - if you’re feeling overwhelmed, anxious, or if you just need someone to talk to.
Some common signs of postpartum depression are:
- Feeling sad or hopeless most of the time
- Having no interest in things you used to enjoy
- Not caring for yourself as well (dressing, showering)
- Trouble focusing
- Not managing daily chores
- Sleeping or eating too much or too little
Learn more about maternal mental health .
Yes. They’re trained to understand and respect your culture and any difficulties you’ve experienced.
Our counselors speak English and Spanish. You may use text telephone (TTY) or another relay service to contact the Hotline. We also offer interpreters who can support over 60 languages, including:
Yes. Pregnancy and the birth of a baby can affect the whole family. Partners and family of pregnant and postpartum people are encouraged to contact the Hotline.
Help spread the word
Use our promotional toolkit to share our Hotline. You can also order a limited number of printed products for free .
Share the Hotline with a friend
I just learned about the National Maternal Mental Health Hotline and wanted to share this free resource. Text 1-833-TLC-MAMA any time to talk with a trained counselor.
If you're a new or expecting parent, the Hotline is a text away. #MaternalMentalHealth #TLCMAMA
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Reproductive Health
- Depression Among Women
- Reproductive Health in Emergency Preparedness and Response
- Teen Pregnancy
- Infertility - Frequently Asked Questions
- Data and Statistics
- Women's Reproductive Health
- Contraception
- Health Care Providers
- CDC Contraceptive Guidance for Health Care Providers
- Unintended Pregnancy
- Emergency Preparedness and Response Tools and Resources
- Evidence-Based Teen Pregnancy Prevention Programs
- Teen Pregnancy Projects
- FROM DATA TO ACTION
- HEAR HER Campaign
- Maternal Mortality Prevention
For Providers: Teens Visiting a Health Clinic
At a glance.
As a health care provider, you can play a role in supporting adolescent health and well-being by providing equitable access to high-quality sexual and reproductive health (ASRH) services.
Ensure you are providing the recommended ASRH clinical services and youth-friendly practices. Also, check out the Infographic: A Teen-Friendly Reproductive Health Visit .
Confidentiality
- Teens receive clear information about their state's laws governing the rights of adolescent patients to confidentiality and to consent to care or treatment. A teen's health information cannot be shared with anyone—including parents or guardians—without the teen's written permission, unless required by law or if the health care provider is concerned the teen might harm him- or herself or someone else.
- Billing procedures should maintain teen's confidentiality. If this is not possible, the provider or billing staff advises the teen about the potential breach of confidentiality and provides options. For example, the patient might want to pay out of pocket or look for a health center that provides confidential care for teens.
- The provider has a counseling area to discuss sensitive topics with teens that provides visual and auditory privacy. It is important that other health care staff or clients cannot hear the conversation or see who is participating in the conversation.
- The health center has an examination room that provides visual and auditory privacy.
- At every visit, each teen patient has time alone with a provider to discuss or ask questions about contraceptive and reproductive health concerns, regardless of whether the visit is urgent or preventive.
- Staff members do not discuss teens' information in common office spaces.
- Medical records are kept secure and are accessible only to select health care staff, such as through the use of locked files, or password-protected electronic medical records.
- Teens receive clear information about informed consent. They know their right to complete and understandable information about their care and medical procedures, and their right to give permission to receive medical care related to contraceptive and reproductive health.
- Teens receive clear information that confidential contraceptive and reproductive health services are available without the need for parent or caregiver consent, consistent with state laws and regulations.
Cultural and linguistic appropriateness
- The health center environment and staff leave teen patients feeling respected and engaged in their health care.
- Culturally competent care is provided, meaning all care is sensitive to and respectful of each teen's culture, ethnicity, community values, religion, language, educational level, sex, gender, and sexual orientation.
- The care provided addresses the unique biologic, cognitive, and psychosocial needs of adolescents.
- Conversations between teens and providers are two-way, where teens feel respected and not judged.
Comprehensive services
- Teens are informed of all contraceptive and reproductive health services available at the specific health center; a referral is provided for any contraceptive or reproductive health services that are not available at the specific health center.
- Teens' contraceptive and reproductive health needs are assessed at every visit. Counseling is provided on all methods to prevent pregnancy using a patient-centered approach that is respectful of and responsive to patients' preferences, needs, and values.
- A wide range of contraception is available via prescription or dispensed on site, including intrauterine devices (IUDs), implants, pills, the shot, patch, and ring.
- The provider promotes "dual protection": using a condom for sexually transmitted infection/human immunodeficiency virus (STI/HIV) prevention—and an effective birth control method for pregnancy prevention at the same time.
- Quick Start methods are used for initiation of hormonal contraception and IUDs, such as starting the pill or inserting the IUD on any day of the month.
- Emergency contraception is available to male and female adolescents, either by prescription, dispensed on site, or prescribed for future use.
- Female teens can receive hormonal contraception without prerequisite exams or testing, such as Pap test, pelvic exam, breast exam, or STI testing.
- Teens receive STI/HIV counseling, testing, and treatment without having an exam.
- Human papillomavirus (HPV) vaccine is available and offered when appropriate.
- Mental health, substance use, violence, and other health concerns are assessed and appropriate referrals are made.
Parent/guardian involvement
- Each teen has an opportunity for examination and counseling without parents or guardians present, and the teen's privacy is respected.
- Parents and guardians are informed of the health center's standard procedure for the provider to spend time alone with teen patients to discuss their comprehensive health and wellness.
- The provider encourages the teen to involve parents or guardians in the teen's health care decisions.
- Parents receive clear information on their teen's right to confidentiality, privacy, and informed consent.
- Parents receive medically accurate information and resources on contraceptive and reproductive health, as needed or as requested.
- Parents receive resources on parent-teen communication and adolescent health and development.
Infographic
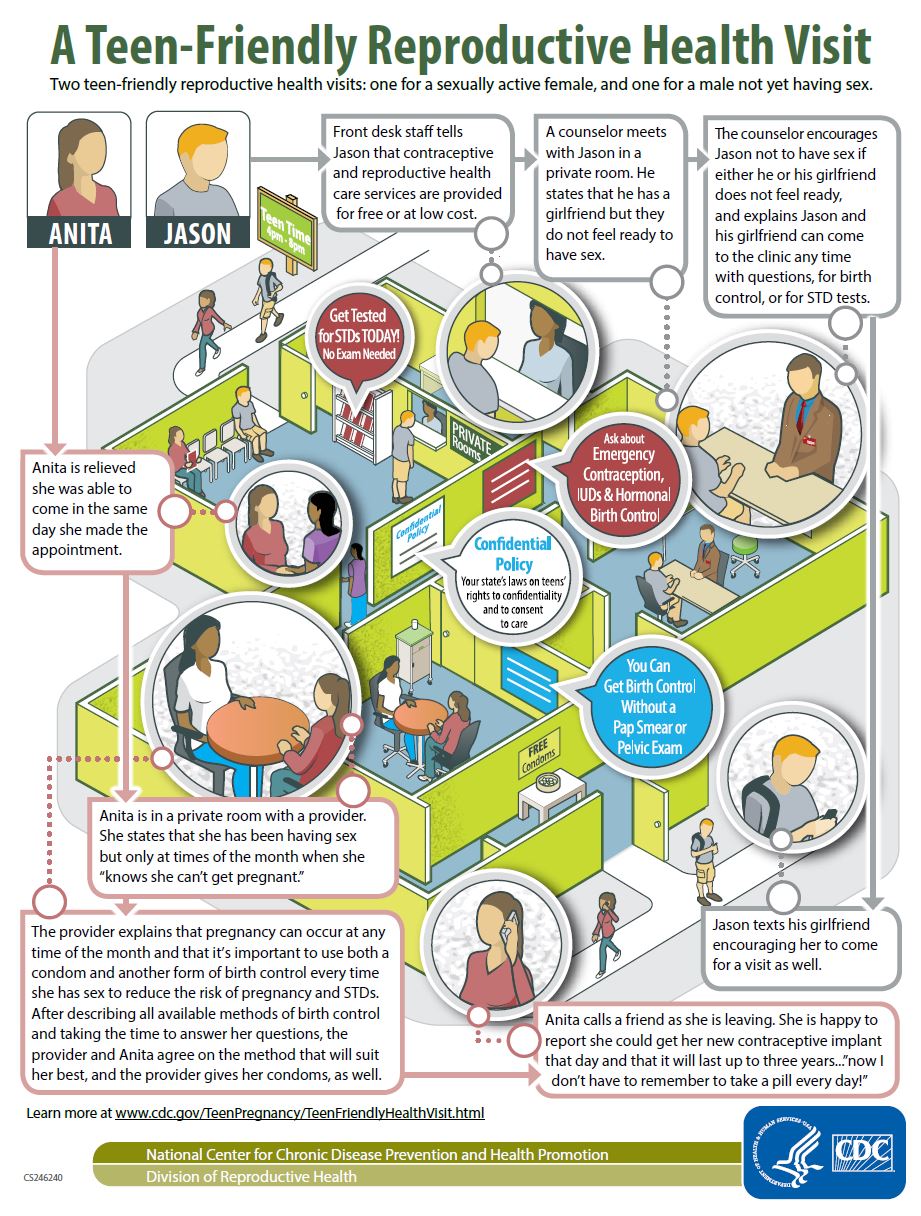
Infographic: A Teen-Friendly Reproductive Health Visit
- AAP Adolescent Sexual Health Resources for Providers
- AAP Equitable Access to Sexual and Reproductive Health Care for All Youth
- Long-Acting Reversible Contraception: Specific Issues for Adolescents
- ACOG Committee Opinion No. 735: Adolescents and Long-Acting Reversible Contraception: Implants and Intrauterine Devices
- ACOG Cervical cancer screening
- AAP Emergency contraception: policy statement
- Minors and the right to consent to health care
- An Overview of Minors' Consent Law
Reproductive Health
CDC’s Division of Reproductive Health focuses on issues related to reproductive health, maternal health, and infant health.
For Everyone
Public health.
- Skip to main content
- Keyboard shortcuts for audio player
The Picture Show
Perspective, a look at what could be the future for postpartum care in america.
Ali Lapetina

Farida Azizova-Such inside the nursery rocking her son to sleep. "He was 5 weeks when we started coming. It's just my husband and I taking care of him, so I was alone at home. I wanted to find new moms to connect with and a safe space to be able to come and learn about how to take care of a baby, and also my identity shifted when you become a mother." Ali Lapetina for NPR hide caption
Farida Azizova-Such inside the nursery rocking her son to sleep. "He was 5 weeks when we started coming. It's just my husband and I taking care of him, so I was alone at home. I wanted to find new moms to connect with and a safe space to be able to come and learn about how to take care of a baby, and also my identity shifted when you become a mother."
Today, I am the mother of twin 5-year-olds, but back during my postpartum period, also known as the "fourth trimester," I was incredibly overwhelmed and felt so alone. The transition into motherhood brings with it not just joy, but also numerous challenges — mental health struggles, nutritional needs, pelvic floor recovery, and the overarching need for self-care and community. During such a demanding time, when your baby — or in my case, babies — needs so much, who's there to take care of you?
Postpartum care in America is presented as fragmented support services with high costs, leaving most mothers and parents to face this in isolation. During a recent brunch, Sara Hutchins, a mother to a 2-month-old and a 3-year-old, shared her experience about a new postpartum care community she joined in Metro Detroit, known as Fourth Tri Sanctuary. "This place is for mothers to come where they are, come without a shower, take it there. You sit down to breastfeed and someone will approach and ask, 'What do you need?' I thought that, as a second time mom, I don't deserve this because this is a place for first-time moms. It took me a long time to come and explore it — I have found peace when I'm there and I feel at ease. When I come home, I'm a better mom, a better wife, and I'm more patient."

Sara Hutchins becomes emotional during a fireside chat with a mental health professional. Ali Lapetina for NPR hide caption

Sara Hutchins bathing her daughter. Ali Lapetina for NPR hide caption

Arielle Weiner, 32, and her 5-month-old daughter (left) participate in a baby-wearing dance class. Ali Lapetina for NPR hide caption
Fourth Tri Sanctuary offers up to 18 weeks of support for mothers and their babies from certified postpartum doulas and health professionals in an environment designed for healing, education and bonding, and addresses the critical and often overlooked "fourth trimester" of motherhood. Parents whose babies are beyond 18+ months can also receive mom-only support through their weekly programming and amenities.

Farida Azizova-Such nurses her son. "Seeing other moms and then sharing their stories and finding out that, oh, okay, they have this kind of challenge. I have this kind of challenge. It's very similar or I didn't even think about that and how they dealt with it. I learned from that and having experts here." Ali Lapetina for NPR hide caption

June Kelly, a certified postpartum doula and yoga teacher, uses a sound bowl to activate a baby's senses. Ali Lapetina for NPR hide caption

Mothers and their babies attend a baby music class facilitated by June Kelly, a postpartum doula and yoga instructor. Ali Lapetina for NPR hide caption
As I walked into the Fourth Tri Sanctuary for the first time, I felt myself holding back tears. What if a space like this existed when I needed it — would I have not faced such overwhelming challenges — from postpartum depression (PPD), to the critical need for self-care and community. Research conducted by Postpartum International Support shows that although perinatal mental health (PMH) disorders affect 800,000 people ayear, only 25% of them receive support. Each year, hundreds of thousands of parents suffer silently because they don't know what they are experiencing is common, or they feel embarrassed to share. Has essential support for new mothers been lost in our increasingly isolated society?

Mothers participate in an expressive art workshop where they are asked, "What do I need? What can I give?" Ali Lapetina for NPR hide caption

A mother writes an "I am doing enough" message to herself during an expressive art workshop. Ali Lapetina for NPR hide caption

Tiffany Yu pours her breast milk into a bottle after pumping. Ali Lapetina for NPR hide caption
Tiffany Yu, a working mother to two children, aged 14 months and 4.5 years, is a mom-only member at Fourth Tri Sanctuary. She enjoys that it is a mom-only workspace, she can pump in the open and it doesn't matter, she can work a bit and then go lay down before she has to return to being a mom. As a 1.5 generation Chinese American, Tiffany observed the traditional Chinese practice of confinement.
"I had three adults, my mother, my father and my grandmother, come take care of me during my postpartum — the level of support is not common in the West. They cooked every meal and sometimes spoon-fed me while I was nursing my baby. That's the kind of support a mother needs to be able to heal herself and then be there for the baby. I think this is going to affect the trajectory of a nation, how well you support the next generation and the current generation. I just hear people my age — I'm a millennial — say 'Absolutely not. I don't want kids. How can we afford it? Who's going to support us? Day care is so expensive. I don't want to give up my career.' And these problems are in place because there's no support. If there was support like that, it would be a non-issue. So for all those reasons, I talk about this place to everybody. Women here [in America] need this support. It shouldn't be a luxury. It really should be the standard of care — women make up over half our population."

While parents participate in a movement class, postpartum doulas care for their newborn babies. Ali Lapetina for NPR hide caption

Karianne Laurila takes a shower while her child is being cared for by postpartum doulas. Ali Lapetina for NPR hide caption

Karianne Laurila, a second-time mom, holds her child after taking a shower. Ali Lapetina for NPR hide caption
Today, postpartum care services in the U.S. can range from $35-$200 or more an hour for an in-home postpartum doula, mental health professionals, lactation consultants among other additional services women and new parents seek. According to a survey conducted by Lansinoh, 88% of moms said they weren't prepared for the postpartum period, and over 95% of moms think new mothers are not sufficiently supported by our society.
The model of Fourth Tri Sanctuary creates a shared environment where mothers who are in the same stage of life can build community rather than just offering brief, isolated or expensive care. Is Fourth Tri Sanctuary a glimpse into the future of postpartum care in America? And if so, how can we ensure it is accessible to everyone? I spent the week exploring the impact of Fourth Tri Sanctuary on postpartum mothers and parents to examine how this community-centric approach could reshape postpartum care across our nation.

A mother bonding with her child. Ali Lapetina for NPR hide caption
If you or someone you know needs help, call or text 833-852-6262 to reach the National Maternal Mental Health Hotline , which is offers free, around-the-clock, confidential services for pregnant and new moms. In the U.S., interpreter services are available in 60 languages.
Ali Lapetina is a photographer based in Detroit.
- postpartum depression
- childbearing
- postpartum recovery
- Open access
- Published: 15 May 2024
An online survey of women’s views of respectful and disrespectful pregnancy and early labour care in the Czech Republic
- Deirdre Daly 1 ,
- Natalie Sedlicka 2 ,
- Kateřina Švanderlíková 2 ,
- PetraAnn Ann Kovařčíková 2 ,
- Radka Wilhelmová 3 &
- Cecily Begley 1
BMC Pregnancy and Childbirth volume 24 , Article number: 370 ( 2024 ) Cite this article
39 Accesses
Metrics details
To ascertain and explore the views of women and their partners, giving birth in the Czech Republic, of the level of respectful or disrespectful care provided during pregnancy and early labour.
Ethical approval was granted for a descriptive, online anonymous survey of 65 questions, with quantitative and qualitative responses.
The Czech Republic.The survey was completed by 8,767 women and 69 partners in 2018.
Measurements and findings
Descriptive statistics and thematic analysis were used to present results. The majority of women were aged 26-35 years. Most had birthed in one of 93 hospitals, with 1.5% home births. Almost 40% never had an abdominal examination.in pregnancy. Quantitative data analysis revealed that less than half were given information on place of birth, or how to keep labour normal or non-interventionist. Almost 60% did not get information on positions for birth. Most (68%) commenced labour naturally, 25% had labour induced, 40% of them before term, and 7% had an elective caesarean section; 55% stated they had not been given any choice in the decision. Over half of those who had a membrane sweep said permission had not been sought. Half (54%) only had ‘checking’ visits from the midwife in labour.
Key conclusions
Findings reveal a lack of information-giving, discussion and shared decision-making from healthcare professionals during pregnancy and early labour. Some practices were non-evidenced-based, and interventions were sometimes made without consent.
Implications for practice
The examples of disrespectful care described in this study caused women distress during childbirth, which may result in an increased fear of childbirth or an increase in free-birthing.
Peer Review reports
The Czech Republic became a separate state in 1993, after 40 years of socialism and communism in Czechoslovakia ended in 1989. Under communism, the rights of the whole population were repressed and their freedom was restricted. Women, in particular, had little autonomy in what was a very patriarchal country. Since 1993, restrictions have been reduced and women are now more independent and autonomous. However, in the maternity care services, little has changed and the model of care is still one of hierarchy and paternalism, where midwives are not recognised or respected [ 1 ]. Midwifery as a profession was eliminated by the former regime and its reintroduction is a slow process. The professionalisation and the professional authority of midwives is part of the debate on structural health care system change in the context of resistance to giving up the dominant position of Czech gynaecologists and obstetricians in delivery rooms [ 2 ]. In many hospitals, normal births are conducted by obstetricians, with midwives assisting. Midwives are suppressed [ 2 ], not permitted to work autonomously, or to attend home births [ 3 ] and a recent Ministry of Health publication on perinatal care does not mention midwives as core care providers [ 4 ]. In their book, Games of Life, Šmídová et al. (2015) discuss biomedicine’s approach to childbirth in the Czech Republic as being as a state of emergency and high risk and dealt with as a highly medicalised event using routine interventions as precautions [ 2 ]. Although the Czech Republic joined the EU in 2004, midwives are precluded from using their full range of competencies or from offering private independent care [ 3 ]. In addition, the cost of midwifery care to women is not covered by the standard public health insurance and some women opt to give birth at home, either alone or with the help of a doula [ 3 ]. Set in the context of improving the quality of maternity care, the Ministry of Health sought ‘Experiences of Obstetrics’ from parents via their Facebook page in 2016. A total of 689 contributions from 486 original comments were posted and analysed to identify recommendations. Overall, the analysis showed clear requirements for changing the system which the authors described as medically-guided childbirth and care with a high level of intervention. The authors concluded that practically all proposed recommendations were aimed at enabling non-interventional births. Other recommendations referred to the choice of place of birth and using of the latest scientific evidence to inform practice [ 5 ]. In addition, some maternity hospitals have introduced radically different regimens of care and embraced practises such as gentle birthing, acupuncture, fathers in labour rooms, and other innovations that aimed humanise childbirth [ 6 ].
There were 93 maternity hospitals in the Czech Republic in 2018. Since 2019, pilot Centres of Midwifery (CPA) were opened. First, two birth apartments were built in Prague with midwives starting to provide prenatal care for women with no, or low, medical and obstetric risks, in addition to additional obstetric care provided elsewhere. However, an obstetrician must decide if the midwife can be the primary carer during birth. The second CPA opened in Brno in 2021, with midwives supporting and leading physiological birth. It is important to acknowledge that two midwifery centres existed in the early 2000s but, despite having favourable birth outcomes, the second of these was closed in 2007 ( http://www.biostatisticka.cz/jak-to-byvalo-ve-vrchlabi/ ).
Respectful maternity care is a human right [ 7 ]. In 2014, the World Health Organization (WHO) re-emphasised that being disrespected in childbirth not only infringed women’s rights but also discouraged women from using maternity care services [ 8 ], which could adversely impact on their health [ 9 ]. Disrespectful care can comprise physical abuse, discrimination, abandonment, or detention in facilities but also care that is non-consented, non-confidential, or non-dignified [ 10 ]. Miller et al. [ 11 ] associated evidence-based care with respectful care indicating that care that is non-evidence based is un-dignified, and disrespects women’s rights. More recently Lappeman and Swartz [ 12 ] suggested that silence between healthcare providers and the women in their care also can be a form of neglect. Findings from systematic reviews [ 13 , 14 ] and numerous empirical quantitative and qualitative studies demonstrate its widespread existence across the world [ 15 , 16 , 17 , 18 , 19 ]. Disrespectful care during childbirth is not a new phenomenon and, by exploring the long history of obstetric violence, O’Brien and Rich [ 20 ] locate biological reproduction as a site of social violence.
In the context of the post-socialist transformation in the Czech Republic, many women’s maternity care needs are still not paramount and many have no autonomy [ 1 , 3 ], shown by healthcare professionals not preserving women’s dignity or privacy during examinations or when in labour and, sometimes, ignoring women’s refusal of consent or interventions [ 1 , 21 ].
The Czech Republic does not publish complete data on maternity care practices, intervention rates or statistics either in individual hospitals, or on births at home. In 2017, a private statistician started a court case to seek access to data on care in all maternity hospitals, but her request has not yet been granted [ 22 ].
This paper presents results from an anonymous online survey of women’s, or their partners, views on the care experienced when pregnant with and giving birth to their first baby in the Czech Republic. It follows a similar study of healthcare professionals’ views [ 23 ], conducted following a television documentary shown in the Czech Republic that appeared to indicate the use of some poor practices in maternity care [ 21 ]. A later documentary, which included women’s narratives, also highlighted the continuing existence of malpractices and lack of evidence-based practices [ 24 ]. Apart from these documentaries, and anecdotal evidence, there are minimal data on women’s or couples’ experiences of maternity care and services in the Czech Republic.
The study aimed to ascertain and explore the views of women, and partners of women, who had given birth in the Czech Republic of the level of respectful or disrespectful care provided for them during pregnancy and early labour. A descriptive online anonymous survey containing 65 questions was designed (Additional file S1 ). Five questions related to respondents and the age of their child(ren). Thirteen questions related to specific antenatal and intrapartum actions/interventions (e.g., induction of labour, application of electronic fetal monitoring etc.) had ‘Yes/No/Not applicable’ responses and 47 questions included open text comments to enable respondents to elaborate on the care, intervention(s) experienced or interactions with healthcare professionals. The quantitative questions were based on evidence and recommendations from relevant Cochrane reviews which were used in a previous survey of maternity care professionals’ views of respectful and disrespectful maternity care in the Czech Republic [ 23 ]. We also incorporated questions relating to nine of the 12 domains identified in a review of 67 studies from 32 countries on women’s perspectives of respectful maternity care [ 25 ]. These included: being free from harm and mistreatment, maintaining privacy and confidentiality, preserving women’s dignity, prospective provision of information and seeking informed consent, ensuring continuous access to family and community support, engaging with effective communication, respecting women’s choices that strengthens their capabilities to give birth, and provision of efficient and effective care and continuity of care. We did not include questions on the physical environment or resources, equity of services or competence and motivations of personnel.
The survey content was developed with nine midwives, doulas and women who had birthed in the Czech Republic, and assessed for acceptability and face validity with 20 women. The survey was prepared in English by CB and DD and translated into the Czech language, and back-translated from Czech to English by NS, KS, PK. Consistency was also checked between the two versions by two other bilingual volunteers. Ethical approval was granted by the Research Ethics Committee, School of Nursing and Midwifery, Trinity College Dublin [14 November 2016].
Participants
Participants were women aged 18 years and over, or partners of women, who had given birth in the Czech Republic. All participants were informed about the study and given the opportunity to ask questions. All were asked to complete the survey in relation to their experiences while pregnant and giving birth to their first baby.
Recruitment
We identified volunteer representatives in each region, through national professional organisations, universities, midwifery schools, hospitals, other health/helping professional fields, participants at birthing seminars (APODAC, UNIPA, etc.), who advertised and provided information on the study in local places/services such as maternity centres, kindergartens, lactation advisors, doulas, associations concerned about birth topics or child education, national magazines and other media. The survey was mainly distributed through personal recruitment (emailing/facebook notices, messages and sharing), with women sharing it with others thereafter. The main channel was Facebook (APODAC pages, JakJinak and other personal profiles of the members of the association) but the survey was then also advertised by various maternal centres and mother and baby websites, and other professional organisations. Those willing to take part completed the survey online, between 1st March 2018 and 31st May 2018. At the start of the survey, participants were informed that the survey was anonymous and that submission of the survey was taken as giving consent to participate.
Data collection
The survey was anonymous, prepared in the Czech language, and administered via Survey Monkey®.
Participants were asked;
their age range, how old their youngest and oldest children were, the name of the hospital they gave birth in (or if they had a home birth);
to answer all questions in relation to their first-born baby;
what information they were given on aspects such as: choices available for place of birth, mode of birth or how to keep labour remaining natural or non-interventionist;
whether or not they had abdominal examinations performed in pregnancy;
whether or not they had, and whether or not they were offered choice regarding induction of labour or elective caesarean section.
Data analysis
Quantitative data were analysed using descriptive statistics, and the frequency with which care practices or interventions occurred are presented as proportions. Respondents’ open text comments were analysed by a team of four researchers applying descriptive codes, merging codes under category headings, followed by thematic analysis using a data-driven approach [ 26 ]. For example, comments relating to consenting to/declining an intervention were categorised as ‘Consent’, ‘Refusal’, or ‘Healthcare practitioners’ reaction’ when care was declined, etc., and comments relating to induction of labour were categorised as ‘Reasons given for induction’, ‘Reasons given for timing of induction’, etc. The team worked together initially to develop code definitions, and then independently, with a final phase of consensus-seeking to ensure comparability across all codes and categories. The first and last authors then acted as peer debriefers [ 27 ], adjudicating on the appropriateness of the thematic analysis, once translated into English. When appropriate, direct quotations (translated, as necessary, into English), are used to complement the quantitative data.
Characteristics of the sample
A total of 10,200 people completed part of the survey, and 8,920 completed the full survey. Data from one respondent aged less than 18 years was removed, under the terms of our ethical approval. Of the remaining sample, 8,767 (98.31%) were women who had had a baby in the Czech Republic, and 69 (0.77%) were partners of women who had birthed in the Czech Republic and were reporting in relation to their partner’s experiences. The remainder were ‘another person interested in maternity care’ ( n = 23), a midwife ( n = 43), a doula ( n = 6), and ‘other healthcare worker providing maternity care in the Czech Republic’ ( n = 11). Although all participants had been asked (if they were a healthcare professional) to answer about their own experiences, for the purpose of this arm of the study, these participants’ responses ( n = 83, 0.92%) were omitted, as we had published healthcare professionals’ views already [ 23 ]. This left a final sample size of 8,836. For half the participants, their first baby’s birth had taken place either within the month prior to completing the survey (5.25%, n = 462) or between one month to one year previously (43.70%, n = 3,846), with the remaining participants (51.05%, n = 4,493) completing the survey more than one year after the first birth.
Responses to questions varied according to question type and place in the survey. For example, response rates for the first 21 questions varied from 91% to 100%, while those for the more detailed questions on labour and birth (questions 22–35) varied from 80% to 89%. Later questions (36 to 65) had response rates from 76% to 80%, with question 39 (‘Were you allowed to eat light diet in labour?’) gaining the lowest response rate of 73%. In all questions, results are given as percentages of the actual number responding.
The majority of those who gave their age ( n = 8,817) were between 26 and 30 years old ( n = 3,258, 36.95%), with a further 33.33% ( n = 2,939) aged 31–35 years (Table 1 ). The average age was 30 years.
Half of the respondents had just one child ( n = 4,428, 50.23%) and the remainder had other children aged one to four years ( n = 2,500, 28.36%), five to eight years ( n = 1,023, 11.60%) or more than 8 years of age ( n = 864, 9.80%). Respondents were asked where they, or their partner, had given birth. A small number ( n = 132, 1.50%) had given birth at home. The remainder had birthed in one of 93 hospitals (Additional file S2 ).
The quantitative findings on experiences are presented in tables and complemented with illustrative direct quotes from respondents’ free-text comments. The proportion of comments are also given, when available, to show the frequency of their use.
Choice and care during pregnancy
Care in pregnancy included the obstetrician/gynaecologist, staff in the hospital (e.g., hospital midwife, nurse, other health care professionals – postnatal nurse, doctor etc., or private midwife permitted to provide care in hospital but as a doula only, or doula), or the woman’s ‘secret home-birth midwife’ performing an abdominal examination once or twice ( n = 2,227, 25.53%), on every visit ( n = 3,058, 35.06%) or never ( n = 3,438, 39.41%). Less than half of the women, when attending for care in their first pregnancy, were given information by staff caring for them on where or how they might give birth, and only a quarter were given information on how they might keep labour natural or avoid interventions (Table 2 ).
Mode of birth and gestation at birth
Table 3 shows mode of birth, method of induction of labour and gestation at birth. For the majority of women in their first pregnancy, labour started spontaneously at, or after, their due date ( n = 5,652, 63.96%). The overall induction of labour rate was 25.03% ( n = 2,077/8,299) and the overall elective CS rate was 7.04% ( n = 584/8,299). Half of all women who had labour induced said this occurred before term ( n = 944, 38.16%) or at term ( n = 282, 11.40%). Of those who had a CS, 835 women (49.29%) said this was performed before term, and 195 (11.51%) at term, with a further 21.84% ( n = 370) having their elective CS by 41 weeks’ gestation.
The majority ( n = 2,543, 94.71%) gave qualitative comments on why they or their carers had not waited for labour to start spontaneously. The reasons for inducing labour included, mainly, ‘pregnancy after term ’ ( n = 709, 27.88%), which had been explained to some women as being between 40 weeks and 40 weeks and 4 days to 41 weeks and 6 days. Very few women stated ‘after 42 weeks’ ( n = 14, 0.55%), and 191 women (7.51%) stated ‘before term’ without adding comments. Some women ( n = 126) said that they were informed by their doctors that it was illegal to permit pregnancy to go far over-due (sometimes as little as 40 weeks plus one day); for example, one woman said that her doctor had said: ‘C zech law does not allow us to wait more than 41 weeks and 3 days’ . Comments made by the women as to how ‘post-term’ had been described to them included: ‘Everything over 41 weeks may be dangerous for the baby, there is no more time for waiting ’; ‘ You are already a couple of days after term so we make it a bit quicker’; ‘You are overdue, it’s already after 38th week’ , or ‘ From week 40 it is post-term so we have to induce it’. One woman said: ‘ Doctor was afraid of overdue. That’s why she did Hamilton manoeuvre the 9th of March, the little one was born 10th. My expected date of birth was 17th’.
The second most common reason for induction was ‘Medical reasons due to maternal factors’ ( n = 583, 22.93%) (e.g., pre-eclampsia) and ‘ Medical reasons due to baby factors ’ was third ( n = 332, 13.06%). This included ‘ baby is too big ’ ( n = 167); ‘ position of the baby ’ ( n = 140 (92 women were induced because of fetal breech presentation and 29 of those were born by CS, 14 with fetal breech presentation as the primary reason for CS)); ‘ bad fetal heart tracing ’ ( n = 109) or ‘ baby is not growing ’ ( n = 46, of whom 11 had actual growth restriction diagnosed). Women often gave a combination of reasons therefore percentages are not given. One woman commented that ‘ the doctor said the placenta could be old already but I was not at term yet and after birth the midwife said it was perfectly ok’ , and a further 309 women (14.88%) stated that no reason was given for induction.
Women who had had an induced labour or a CS were asked if they felt the reason why this was necessary was discussed sufficiently with them (including all the positives and negatives). Just under half ( n = 1,624, 49.11%) thought that it had been discussed sufficiently and the remainder ( n = 1,683, 50.89%) did not. Less than half of women ( n = 1,472, 45.14%) felt they had been offered choice in the decision but 1,789 women (54.86%) stated that they had no choice. The majority had labour induced by rupturing the membranes, with or without use of drugs (Table 3 ). Of those who had a membrane sweep performed, 908 (56.33%) said the doctor had not asked for their permission before doing this.
Care provider and support during labour and birth
The quantitative data showed that women were usually cared for in labour with their first baby by an obstetrician/gynaecologist or doctor ( n = 6,778, 76.88%), and/or a hospital midwife ( n = 6,626, 75.16%). Small numbers of women were cared for by a private midwife who had a contract with the hospital (and was permitted to care for them in labour as a midwife) ( n = 212, 2.41%), or a private midwife without a contract with the hospital (who was permitted to care for them in labour as a doula only) ( n = 197, 2.24%). Doulas cared for 246 women (2.79%), and 388 (4.40%) were cared for by ‘other people’. No additional comments on ‘others’ were provided. Ninety-seven women (1.10%) were cared for by an obstetrician/gynaecologist or doctor who was given an extra payment directly by them.
A small minority of women ( n = 615, 7.57%) were not accompanied by any lay person in labour. The majority were supported by the baby’s father ( n = 6,617, 81.32%), a private midwife ( n = 276, 3.39%), doula ( n = 242, 2.97%), or another person ( n = 385, 4.73%). In general, these companions were allowed to stay with them (pre-Covid pandemic) for the whole of their labour (with short breaks) ( n = 5,911, 82.05%) or for about half the labour ( n = 502, 6.87%); however, 11% of women were only permitted to have their companions for a short time at the start, or end, of labour ( n = 475, 6.50%) or not at all ( n = 316, 4.35%). Almost three-quarters of the women ( n = 5,700, 71.12%) had no birth plan documented. Of the 2,315 women who had a birth plan, 1,035 (44.71%) said that it was respected, 601 (25.96%) said that it was not respected and 679 (29.33%) said that they were convinced by the doctor and/or midwife to change their birth plan during their labour. One-third of women ( n = 2,585, 34.89%) said that the health professional(s) who cared for them in labour introduced themselves when they entered the labour room or when they met them for the first time, and a further 49.61% ( n = 3,675) said that some of the health professional(s) did this; however, 1,148 of the women (15.50%) said that the health professional(s) looking after them never introduced themselves.
The majority of women were in labour (in hospital) on their first birth for more than 10 h ( n = 2,858, 38.56%), with a further 1,705 (23%) in labour for over six and up to 10 h and 2,071 women (28.34%) in labour for over two and up to six hours. Most women ( n = 5,811, 79.78%) felt that they were given privacy in the first stage of labour, but 1,473 women (20.22%) did not. Less than 40% of women had a midwife or other healthcare professional staying with them and supporting them during labour all of the time except for short breaks ( n = 1,245, 17.36%) or most of the time ( n = 1,565, 21.82%). The majority ( n = 3,846, 53.63%) said they only had visits from the midwife to check how they were and 284 (3.96%) said they did not have a midwife caring for them at all.
Data from the 8,836 women who had birthed in one of the 93 hospitals in the Czech Republic, or at home, shed light on women’s recent experiences of prenatal and early labour and birth care in the Czech Republic. Overall, our descriptive statistics show the frequency of aspects of care and interventions performed, and women’s qualitative comments provide rich context on these. The inclusion of the proportions of comments provided serves to show that many women’s experiences are, in some instances, common practices.
We asked women minimal information on the content of their pregnancy care because of the variation in the scheduling and content of care provided in the Czech Republic, but it was clear that abdominal examination was not performed regularly, with 39% of women stating that they never had one performed. It is possible that many of these women had ultrasound scans performed throughout their pregnancy, instead of clinical examination. Forty percent of women were never given information by staff caring for them on where or how they might give birth, a finding in common with a number of studies from other countries [ 28 , 29 ]. Information-giving on available places of birth has been identified as an essential component of women’s autonomy [ 30 ], a key tenet of respectful care. A study exploring satisfaction with maternity care in the Czech Republic, with 1,195 respondents, also found that ‘information giving’ and an ‘empathic and respectful approach’ were lacking, and the aspect rated lowest (34%) was ‘control and involvement in decision-making’ [ 31 ].Women who have had a poor previous childbirth experience may be driven away from formal healthcare to give birth alone, if they are not provided with, and are aware of, other possibilities such as homebirth, midwife-led care or birthing centres [ 32 ]. Even when women are aware of other options, it may be difficult, if not impossible, to find an alternative healthcare provider or facility because of limited options. It may also be prohibitively expensive for women to employ a private midwife when the fee is not covered by insurance. The lack of discussion, together with unsatisfying conditions in hospitals [ 31 ], are the main reasons why women choose homebirth in the Czech Republic [ 9 ].
Only one quarter of women in this study were given information on how they might keep their labour normal or non-interventionist as it progressed. Given the documented ill-effects of too much intervention given too soon in labour [ 11 ], this is a key area for the provision of information for women, to increase their empowerment and self-efficacy.
The overall induction of labour rate of 25% among this group of women is similar to many other European countries [ 33 ]. Induction of labour, when necessary, is a useful and important method of care. However, half of all women who had their labour induced said this occurred before or at term, with a further 25% having labour induced by 41 weeks’ gestation, despite the recommendation from the Czech Gynaecological and Obstetrical Society (CGOS) [ 34 ] that there ‘ should be steps taken to end pregnancy in between 41 and 42 weeks ’, so that ‘ pregnancy should be ended by 42 weeks + 0 days’ (not 41 weeks + 0 days). Interpretation of this recommendation by individual healthcare providers is permitted, and earlier definitions of ‘term’ appear to be used frequently.
Qualitative comments from the women also seemed to indicate confusion around the meaning of ‘term’ and ‘post-term’. It is questionable that 75% of all the women who had induction of labour before the ‘post-term’ period, as recommended by the CGOS, required it for a genuine medical, obstetrical or fetal reason. Considerable variation is seen across the world in induction of labour rates, with no difference in outcomes, indicating that some inductions are unnecessary [ 35 ], as seems to be the situation in the Czech Republic. Induction of labour for subjective, non-medical, reasons was also noted in research from the United States [ 36 ], and is linked in a number of countries with increasing CS rates [ 35 ].
Just over half of the women who had labour induced thought that the reason that this was necessary was discussed sufficiently with them, but 55% had not been given any choice in the decision. The greater involvement of obstetricians at all levels of care in the Czech Republic may account for this lack of choice, as other countries such as the US [ 37 ] have shown that midwifery care encourages women’s decision-making.
When labour is induced by artificial rupture of membranes and/or use of oxytocin infusion or prostaglandin pessaries, the woman is aware of the procedure in advance and, by presenting at the hospital on the date requested, has given tacit (and, usually, written) consent. Thirty-five percent of women in this study had labour induced by the Hamilton manoeuvre (sweeping the membranes) which can be effective in achieving a spontaneous onset of labour and can potentially reduce the incidence of a more formal method of induction of labour [ 38 ]. However, 56% of the 1,364 women who had the Hamilton manoeuvre performed said that the doctor had not asked for their permission beforehand. This is an example of very disrespectful care and may be occurring, unacknowledged, in many other countries as a recent systematic review [ 39 ] failed to find any research in this area. Not gaining women’s consent for interventions or procedures is not uncommon, as is shown in systematic reviews [ 40 , 41 ] and in studies conducted in a myriad of settings globally [ 15 , 16 , 17 , 41 , 42 , 43 ].
The majority of women had a companion of their choice with them throughout labour. However, 11% of women were only permitted to have their companion with them for a short time at the start, or end, of labour, a practice that should never occur; having a companion to support one in labour is a basic human right, upheld by the WHO [ 44 ]. An obstetrician/gynaecologist or doctor provided intrapartum care for 77% of women, and 75% said that they were cared for by a midwife instead of, or as well as, an obstetrician. However, the majority of women (54%) said that they ‘ only had visits ’ from the midwife to check how they were, with no-one present with them throughout the birth process, and 4% said that they did not have a midwife caring for them at all. Lappeman and Swartz’s [ 12 ] qualitative study, which used labour ward observations as the primary data collection method, revealed the ‘silence of the labour ward’ and the ‘neglect of the neglect’ where women in labour ‘lay in beds alone’, rarely with companions. Research findings from across the world show that women who receive continuous labour support (from midwives, doulas, or lay companions), especially from one or two known midwives, are more likely to have shorter labours with less use of pain medication, less intervention, birth spontaneously [ 37 , 45 , 46 ]and be more satisfied [ 47 , 48 , 49 ].
Other instances of non-respectful care are revealed in the responses from 16% of women who said that clinicians looking after them never introduced themselves when they entered the labour room or met them for the first time. Analysis of the psychosocial climate in maternity hospitals in the Czech Republic similarly indicates the need for enhanced communication skills by healthcare providers, especially when communicating consistent information [ 31 , 50 ]. Less than one-third of women had a birth plan but over half of those who had said their plan was not respected or that they were persuaded by the clinician to change their plan during labour. In addition, 20% were not given privacy in the first stage of labour, similar to findings from other studies in Jordan [ 51 ] and Turkey [ 52 ]. Experiencing privacy and healthcare provider courtesy in labour have been shown to be key determinants of maternal satisfaction, in a review of 54 research papers from low-income countries [ 53 ].
Overall, our quantitative and qualitative data reveal aspects of disrespectful prenatal and intrapartum care. Taken in their entirety, there was a considerable number of women who had no information on and no choice in their place of birth, procedures and interventions performed without explanation or consent and who were ‘persuaded’ to alter their plan for their care. Our qualitative comments very much resonate with those in Kuipers et al.’s [ 18 ] study which explored the experiences of women, including women who birthed in the Czech Republic, who had a negative or traumatic birth and the value, sense and meaning assigned to the social space of birth. The authors stated that women frequently experienced their birth environment as coercive and disrespectful, described being ‘physically forced into positions or spaces’ repeatedly (p4) and an environment that depicted ‘scenes of horror’ (p5).
Cohen Shabot [ 54 ] characterises obstetric violence, and any and all forms of disrespecting pregnant women, as a feminist issue which must be examined through feminist views on violence i.e., violence directed at women and part of a general patriarchal oppression of women. She describes it as gender violence because women are its main victims. According to Šmídová et al. (2015), the privately-held and shared convictions amongst obstetricians that change is needed in healthcare relating to childbirth contrasts markedly with their reluctance to say this publicly and be critical of the system. Whilst the opinions of the obstetricians, those who dominate and currently hold the power within the maternity hospitals and services, remain polarised and open discussions are absent, implementation of a woman-centred approach to care and service may be slow. On a more positive note, the Government’s Gender Equality Strategy for 2021–2030 acknowledges that there has long been a strong social demand for a respectful approach and humanisation of obstetrics care for women (acknowledged as being most women) who experience physiological pregnancy and birth (most women). It also states that the Ministry of Health has begun to respond to this by working on the concept for supporting the establishment of midwifery centres within maternity hospitals [ 55 ]. The Strategy also recognises the persistent legislative and restrictions that midwives have long faced and the resulting negative impact on women and their families in terms of choice of place, method and circumstances of childbirth. It also acknowledges that this is further complicated by the absence of national standards of care, the links between the various professions that offer peripartum care, and the repeated criticisms from international institutions and others.
Strengths and limitations
A strength of this study is that data were provided by a large sample: 8,836 women who had experienced birth in one of the 93 hospitals in the Czech Republic, or at home. The inclusion of women’s qualitative comments, including proportions when relevant, provide rich and detailed context on interventions and procedures. The main limitation is that surveys were completed by a self-selecting sample of women, or their partners, and are therefore potentially biased. Whilst we sought to recruit participants from a wide range of sources, including maternity hospitals, obstetric and gynaecology clinics, postnatal centres, kindergartens etc., it is possible that the experiences reported here may not be representative of women birthing in the Czech Republic. Whilst 51% of respondents had birthed their baby more than one year previously, which may raise issues of recall bias, the accuracy of women’s memories of their experiences, and their agreement with data recorded in their maternity care records [ 56 ] even up to five years after the birth, has been documented [ 57 ]. Whilst the views of 69 partners were included, partners answered the questions in relation to their partner’s experiences. We did not analyse these separately but including their information about their partners was deemed important.
Conclusions
Findings reveal a lack of information-giving, discussion and shared decision-making from healthcare professionals in the maternity care services. There are also some indications that some practices were not based on evidence. A thorough audit of clinical practices, in individual hospitals and nationally, and the open publication on labour and birth outcomes, and women’s experiences of care, is needed. Women described unacceptable aspects of care such as having procedures performed without their consent, and concerns around discourtesy of healthcare professionals and lack of privacy. Without doubt, these experiences cause women great distress during, and even after, childbirth. Our findings highlight areas in need of urgent improvement in maternity care services in the Czech Republic. Initiatives such as the Ministry of Health‘s 2015 call for comments from parents on their experiences of services are to be commended and continued, as is the implementation of the Government’s Gender Equality Strategy and other initiatives that target women-centred reformations within the maternity care system.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Hrešanová E. Nobody in a maternity hospital really talks to you: socialist legacies and consumerism in Czech women’s childbirth narratives. Sociologický časopis/Czech Sociol Rev. 2014;50(6):961–85. https://doi.org/10.13060/00380288.2014.50.6.150 .
Article Google Scholar
Šmídová I, Šlesingerová E, Slepičková L. Games of Life. Czech Republic: Masarykova Univerzita.201. Availabe at: https://www.perlego.com/book/3514299/games-of-life-czech-reproductive-biomedicine-sociological-perspectives-pdf .
Hořejší A. Analysis of the current situation in obstetrics with regard to the position of midwives and the possibility of free choice of women. 2020. https://www.unipa.cz/analyza-soucasneho-stavu-v-porodnictvi-s-ohledem-na-postaveni-porodnich-asistentek-a-moznosti-svobodne-volby-zen/ .
Ministry of Health. Methodical recommendation of Ministry of Health for providers of care in fields of gynaecology, obstetrics and neonatology 2020. https://www.mzcr.cz/metodicke-doporuceni-mz-pro-poskytovatele-zdravotnich-sluzeb-v-oboru-gynekologie-a-porodnictvi-a-neonatologie/ .
Vondráčková L, Šmídová I, Working Group on Obstetrics of the Government Council for Gender Equality. Analysis of the discussion Experiences from maternity hospitals established by the Ministry of Health on Facebook. Research report for the. 2015. Masaryk University: Czech Republic. https://vlada.gov.cz/cz/ppov/rovne-prilezitosti-zen-a-muzu/dokumenty/analyza-diskuse-_zkusenosti-z-porodnic_-zalozene-ministerstvem-zdravotnictvi-na-facebooku-146451/ .
Hrešanová E. The Island of Alternatives: power, Medical Science, and Gentle Birthing in Socialist Czechoslovakia. J Hist Med Allied Sci. 2018;73(1):73–95. https://doi.org/10.1093/jhmas/jrx056 .
Article PubMed Google Scholar
White Ribbon Alliance. Respectful Maternity Care: The Universal Rights of Childbearing Women. 2011. http://whiteribbonalliance.org/campaigns2/respectful-maternity-care/ .
WHO. The prevention and elimination of disrespect and abuse during facility-based childbirth. 2014. http://apps.who.int/iris/bitstream/10665/134588/1/WHO_RHR_14.23_eng.pdf?ua=1&ua=1
Durnová A, Hejzlarová E. Domácí porody v Česku: motivace, důvody a názory žen, které rodily plánovaně doma (2015–2020) [Data set]. Zenodo [Role of the intimacy in Czech controversy about home births (GAČR, 18-10042S)]. 2021. https://doi.org/10.5281/zenodo.4767126 .
Bowser D, Hill K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth Report of a Landscape Analysis. USAID-TRAction Project. Harvard School of Public Health. 2020. https://www.ghdonline.org/uploads/Respectful_Care_at_Birth_9-20-101_Final1.pdf .
Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comande D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–92. https://doi.org/10.1016/s0140-6736(16)31472-6 .
Lappeman M, Swartz L. Rethinking obstetric violence and the neglect of neglect: the silence of a labour ward milieu in a South African district hospital. BMC Int Health Hum Rights. 2019;19(1):30. https://doi.org/10.1186/s12914-019-0218-2 .
Article PubMed PubMed Central Google Scholar
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The mistreatment of women during Childbirth in Health facilities globally: a mixed-methods systematic review. PLoS Med. 2015;12(6):e1001847. https://doi.org/10.1371/journal.pmed.1001847 .
Watson HL, Downe S. Discrimination against childbearing Romani women in maternity care in Europe: a mixed-methods systematic review. Reprod Health. 2017;14(1):1. https://doi.org/10.1186/s12978-016-0263-4 .
Annborn A, Finnbogadóttir HR. Obstetric violence a qualitative interview study. Midwifery. 2022;105:103212. https://doi.org/10.1016/j.midw.2021.103212 .
Correa M, Klein K, Vasquez P, Williams CR, Gibbons L, Cormick G, et al. Observations and reports of incidents of how birthing persons are treated during childbirth in two public facilities in Argentina. Int J Gynaecol Obstet. 2022;158(1):35–43. https://doi.org/10.1002/ijgo.13938 .
Greely JT, Dongarwar D, Crear L, Adeyeye M, Reyna-Carrillo A, Salihu HM. Violence against pregnant women and adverse maternal/ fetal outcomes in the United States: racial/ethnic disparities. Women Health. 2022;62(6):513–21. https://doi.org/10.1080/03630242.2022.2074610 .
Kuipers YJ, Thomson G, Goberna-Tricas J, Zurera A, Hresanová E, Temesgenová N et al. The social conception of space of birth narrated by women with negative and traumatic birth experiences. Women Birth. 2022;S1871-5192(22):00079 – 8. https://doi.org/10.1016/j.wombi.2022.04.013 .
van der Pijl MSG, Verhoeven CJM, Verweij R, van der Linden T, Kingma E, Hollander MH, et al. Disrespect and abuse during labour and birth amongst 12,239 women in the Netherlands: a national survey. Reprod Health. 2022;19(1):160. https://doi.org/10.1186/s12978-022-01460-4 .
O’Brien E, Rich M. Obstetric violence in historical perspective. Lancet. 2022;399(10342):2183–5. https://doi.org/10.1016/s0140-6736(22)01022-4 .
Český Žurnál. Pět zrození, Žurnál Č. Editor. 2015. https://www.youtube.com/watch?v=f-CZgwTC5bk .
Hnilicová J. Jak se kde rodí? 2021. http://jaksekderodi.cz/soudni-spor-2/ .
Begley C, Sedlicka N, Daly D. Respectful and disrespectful care in the Czech Republic: an online survey. Reprod Health. 2018;15(1):198. https://doi.org/10.1186/s12978-018-0648-7 .
Formánková L, Hejzlarová E. Giving birth as a struggle between bodily needs and medical practice, in Making and Doing Exhibition Society for Social Studies of Science (4S). 2020. Available at; https://www.youtube.com/watch?v=5jHBw8NB_8Y .
Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Nogueira Pileggi V, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG. 2018;125(8):932–42. https://doi.org/10.1111/1471-0528.15015 .
Article CAS PubMed Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Kitto SC, Chesters J, Grbich C. Quality in qualitative research. Med J Aust. 2008;188(4):243–6. https://doi.org/10.5694/j.1326-5377.2008.tb01595.x .
Hinton L, Dumelow C, Rowe R, Hollowell J. Birthplace choices: what are the information needs of women when choosing where to give birth in England? A qualitative study using online and face to face focus groups. BMC Pregnancy Childbirth. 2018;18(1):12. https://doi.org/10.1186/s12884-017-1601-4 .
Naylor Smith J, Taylor B, Shaw K, Hewison A, Kenyon S. I didn’t think you were allowed that, they didn’t mention that.’ A qualitative study exploring women’s perceptions of home birth. BMC Pregnancy Childbirth. 2018;18(1):105. https://doi.org/10.1186/s12884-018-1733-1 .
Halfdansdottir B, Wilson ME, Hildingsson I, Olafsdottir OA, Smarason AK, Sveinsdottir H. Autonomy in place of birth: a concept analysis. Med Health Care Philos. 2015;18(4):591–600. https://doi.org/10.1007/s11019-015-9624-y .
Takács L, Seidlerová J. [Psychosocial climate in maternity hospitals from the perspective of parturients I. results from a national survey on perinatal care satisfaction using a representative sample of 1195 Czech parturients]. Ceska Gynekol. 2013;78(2):157–68. PMID: 23710980.
PubMed Google Scholar
Holten L, de Miranda E. Women׳s motivations for having unassisted childbirth or high-risk homebirth: an exploration of the literature on ‘birthing outside the system’. Midwifery. 2016;38:55–62. https://doi.org/10.1016/j.midw.2016.03.010 .
Amyx M, Philibert M, Farr A, Donati S, Smárason AK, Tica V, Velebil P, Alexander S, Durox M, Elorriaga MF, Heller G, Kyprianou T, Mierzejewska E, Verdenik I, Zīle-Velika I, Zeitlin J. Trends in caesarean section rates in Europe from 2015 to 2019 using Robson’s Ten Group classification system: a Euro-Peristat study. BJOG. 2023. https://doi.org/10.1111/1471-0528.17670 .
Czech Gynecological and Obstetrical Society. Post-term pregnancy. 2016. https://www.figo.org/czech-gynecological-and-obstetrical-society .
Seijmonsbergen-Schermers AE, van den Akker T, Rydahl E, Beeckman K, Bogaerts A, Binfa L, et al. Variations in use of childbirth interventions in 13 high-income countries: a multinational cross-sectional study. PLoS Med. 2020;17(5):e1003103. https://doi.org/10.1371/journal.pmed.1003103 .
Salahuddin M, Davidson C, Lakey DL, Patel DA. Characteristics Associated with induction of Labor and Delivery Route among Primiparous Women with Term deliveries in the listening to mothers III study. J Womens Health (Larchmt). 2018;27(5):590–8. https://doi.org/10.1089/jwh.2017.6598 .
Declercq ER, Belanoff C, Sakala C. Intrapartum Care and experiences of women with midwives Versus obstetricians in the listening to mothers in California Survey. J Midwifery Womens Health. 2020;65(1):45–55. https://doi.org/10.1111/jmwh.13027 .
Finucane EM, Murphy DJ, Biesty LM, Gyte GM, Cotter AM, Ryan EM, et al. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2020;2(2):Cd000451. https://doi.org/10.1002/14651858.CD000451.pub3 .
Roberts J, Evans K, Spiby H, Evans C, Pallotti P, Eldridge J. Women’s information needs, decision-making and experiences of membrane sweeping to promote spontaneous labour. Midwifery. 2020;83:102626. https://doi.org/10.1016/j.midw.2019.102626 .
Bohren MA, Mehrtash H, Fawole B, Maung TM, Balde MD, Maya E, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. Lancet. 2019;394(10210):1750–63. https://doi.org/10.1016/s0140-6736(19)31992-0 .
Khalil M, Carasso KB, Kabakian-Khasholian T. Exposing Obstetric Violence in the Eastern Mediterranean Region: a review of women’s narratives of disrespect and abuse in Childbirth. Front Glob Womens Health. 2022;3:850796. https://doi.org/10.3389/fgwh.2022.850796 .
Mayra K, Sandall J, Matthews Z, Padmadas SS. Breaking the silence about obstetric violence: body mapping women’s narratives of respect, disrespect and abuse during childbirth in Bihar, India. BMC Pregnancy Childbirth. 2022;22(1):318. https://doi.org/10.1186/s12884-022-04503-7 .
Smith-Oka V. Cutting women: unnecessary cesareans as iatrogenesis and obstetric violence. Soc Sci Med. 2022;296:114734. https://doi.org/10.1016/j.socscimed.2022.114734 .
WHO. WHO recommendation on companionship during labour and childbirth. 2018. https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/care-during-childbirth/who-recommendation-companionship-during-labour-and-childbirth .
Begley C, Devane D, Clarke M, McCann C, Hughes P, Reilly M, et al. Comparison of midwife-led and consultant-led care of healthy women at low risk of childbirth complications in the Republic of Ireland: a randomised trial. BMC Pregnancy Childbirth. 2011;11:85. https://doi.org/10.1186/1471-2393-11-85 .
Loewenberg Weisband Y, Klebanoff M, Gallo MF, Shoben A, Norris AH. Birth outcomes of women using a midwife versus women using a physician for prenatal care. J Midwifery Womens Health. 2018;63(4):399–409. https://doi.org/10.1111/jmwh.12750 .
Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7(7):Cd003766. https://doi.org/10.1002/14651858.CD003766.pub6 .
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2016;4:Cd004667. https://doi.org/10.1002/14651858.CD004667.pub5 .
Hildingsson I, Karlström A, Larsson B. A continuity of care project with two on-call schedules: findings from a rural area in Sweden. Sex Reprod Healthc. 2020;26:100551. https://doi.org/10.1016/j.srhc.2020.100551 .
Takács L, Seidlerová J. [Psychosocial climate in maternity hospitals from the perspective of parturients II. Predictors of womens satisfaction with perinatal care in the Czech Republic]. Ceska Gynekol. 2013;78(3):269–75. PMID: 23869834.
Hussein S, Dahlen HG, Ogunsiji O, Schmied V. Uncovered and disrespected. A qualitative study of Jordanian women’s experience of privacy in birth. Women Birth. 2020;33(5):496–504. https://doi.org/10.1016/j.wombi.2019.10.006 .
Deliktas Demirci A, Kabukcuglu K, Haugan G, Aune I. I want a birth without interventions: women’s childbirth experiences from Turkey. Women Birth. 2019;32(6):e515–22. https://doi.org/10.1016/j.wombi.2018.12.011 .
Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. Determinants of women’s satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy Childbirth. 2015;15:97. https://doi.org/10.1186/s12884-015-0525-0 .
Cohen Shabot S. Making loud bodies feminine: a Feminist-Phenomenological analysis of Obstetric Violence. Hum Stud. 2016;39(2):231–47. https://doi.org/10.1007/s10746-015-9369-x .
Office of the Government of the Czech Republic. Gender Equality Strategy for 2021–2030. 2021: Czech Republic. https://vlada.gov.cz/assets/ppov/gcfge/Gender-Equality-Strategy-2021-2030.pdf .
Gartland D, Lansakara N, Flood M, Brown SJ. Assessing obstetric risk factors for maternal morbidity: congruity between medical records and mothers’ reports of obstetric exposures. Am J Obstet Gynecol. 2012;206(2):e1521–10. https://doi.org/10.1016/j.ajog.2011.10.863 .
Takehara K, Noguchi M, Shimane T, Misago C. A longitudinal study of women’s memories of their childbirth experiences at five years postpartum. BMC Pregnancy Childbirth. 2014;14(1):221. https://doi.org/10.1186/1471-2393-14-221 .
Download references
Acknowledgements
We would like to thank all the respondents for taking the time to complete the survey and including their detailed comments. We thank Veronika Nezbedová for helping with the preparation of the questionnaire and translating the survey from English to Czech. We would like to thank Dominika Kůželová (APODAC) who contributed to the data analysis and the numerous other people who helped distribute the survey.
This study was unfunded.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Trinity College Dublin, 24 D’Olier Street, Dublin, DO2 T283, Ireland
Deirdre Daly & Cecily Begley
Association for Birth Houses & Centers (APODAC), Týnská ulička 1064/6, , Prague 1, 11000, Czech Republic
Natalie Sedlicka, Kateřina Švanderlíková & PetraAnn Ann Kovařčíková
Faculty of Medicine, Department of Health Sciences, Masaryk University, Brno, Czech Republic
Radka Wilhelmová
You can also search for this author in PubMed Google Scholar
Contributions
DD: contributed to the survey design, and manuscript writing/editing.CB: study development, survey design, data analysis, manuscript writing/editing. NS: contributed to the survey design, translated the study information and survey questions from English to the Czech language, data analysis, translated the qualitative data from Czech to English, manuscript writing/editing. KS: project administration in CZ, contributed to data analysis and review. PK: contributed to translation, data analysis, review and editing. RW: contributed to review and editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Deirdre Daly .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by the Research Ethics Committee, School of Nursing and Midwifery, Trinity College Dublin [14 November 2016]. At the start of the survey, participants were informed that the survey was anonymous and that submission of the survey was taken as giving consent to participate.
Consent for publication
Not applicable. The manuscript does not manuscript contain any individual person’s data in any form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Daly, D., Sedlicka, N., Švanderlíková, K. et al. An online survey of women’s views of respectful and disrespectful pregnancy and early labour care in the Czech Republic. BMC Pregnancy Childbirth 24 , 370 (2024). https://doi.org/10.1186/s12884-024-06448-5
Download citation
Received : 06 January 2023
Accepted : 26 March 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12884-024-06448-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Maternity care
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Families who received at least one home visit (86 percent of the program group) had an average of eight visits over four months before the woman gave birth. Families received a similar amount of home visiting as found in prior studies, including those that found reductions in the percentage of infants born preterm or with low birth weights.
Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife or group prenatal care, here's what to ...
Home visitors work with expectant mothers to access prenatal care and engage in healthy behaviors during and after pregnancy. For example—. Pregnant participants are more likely to access prenatal care and carry their babies to term. Home visiting promotes infant caregiving practices like breastfeeding, which has been associated with positive ...
When to schedule your first prenatal visit. As soon as you get a positive result on a home pregnancy test, book an appointment with an obstetrician, family physician, or midwife.Depending on the practice, it's normal for another provider in the office, like a nurse practitioner or physician assistant, to handle your first visit.
What happens during prenatal visits varies depending on how far along you are in your pregnancy. Schedule your first prenatal visit as soon as you think you are pregnant, even if you have confirmed your pregnancy with a home pregnancy test. Early and regular prenatal visits help your health care provider monitor your health and the growth of the fetus.
showing that home visits by a nurse, social worker, early childhood educator, or other trained professional during pregnancy and early childhood improve the lives of children and families. Home visiting helps prevent child abuse and neglect, supports positive parenting, improves maternal and child health, and promotes child development and school
When to schedule a prenatal visit. Make an appointment for your first prenatal visit once you're aware you are pregnant - when you receive a positive home pregnancy test, for example. Booking it around week 8 of pregnancy is typical. You'll come back regularly in the weeks and months following that initial appointment.
Prenatal care and tests. Medical checkups and screening tests help keep you and your baby healthy during pregnancy. This is called prenatal care. It also involves education and counseling about how to handle different aspects of your pregnancy. During your visits, your doctor may discuss many issues, such as healthy eating and physical activity ...
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant! Even if you are not a first-time mother, prenatal visits are still ...
During the third trimester, prenatal care might include vaginal exams to check the baby's position. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy, especially as your due date approaches. Your health care provider might ask you to schedule prenatal care appointments during your third trimester about every 2 or 4 ...
For a healthy pregnancy, your doctor will probably want to see you on the following recommended schedule: Weeks 4 to 28 — One prenatal visit every four weeks. Weeks 28 to 36 — One prenatal ...
Prenatal care is the health care you get while you are pregnant. Take care of yourself and your baby by: Getting early prenatal care. If you know you're pregnant, or think you might be, call your doctor to schedule a visit. Getting regular prenatal care. Your doctor will schedule you for many checkups over the course of your pregnancy.
During your first trimester, your provider will check your blood to determine your blood type and look for signs of: Blood issues, such as anemia (low iron). Immunity to rubella (German measles ...
For a healthy pregnancy, your doctor will probably want to see you on the following recommended schedule of prenatal visits: Weeks 4 to 28: 1 prenatal visit a month. Weeks 28 to 36: 1 prenatal ...
The most common tests at your first prenatal visit will likely include: [3] Urine test. Your urine may be checked for protein, glucose (sugar), white blood cells, blood and bacteria. Bloodwork. A sample of your blood will be used to determine blood type and Rh status and check for anemia. Trusted Source Mayo Clinic Rh factor blood test See All ...
1st Trimester: 1st Prenatal Visit. It's the first doctor visit of your pregnancy. Congratulations! During this visit, your doctor will check your overall health and determine your due date. They ...
Home visitors and families develop strong relationships and trust. They meet regularly to address families' needs. The Program aims to: Improve the overall health of mothers and children. Get children ready to succeed in school. Improve families' economic well-being. Connect families to other resources in their community (for example WIC.
The California Home Visiting Program (CHVP) is designed for overburdened families who are at risk for Adverse Childhood Experiences (ACEs), including child maltreatment, domestic violence, substance use disorder and mental health related issues. Home visiting gives parents the tools and know-how to independently raise their children.
During prenatal care visits, your doctor, nurse, or midwife may: update your medical history. check your urine. check your weight and blood pressure. check for swelling. feel your belly to check the position of your fetus. measure the growth of your belly. listen to the fetal heartbeat. give you any genetic testing you decide to do.
The quasi-experimental cohort study by Ichikawa et al. 11 compared a prenatal home visit program (at least one nurse home visit lasting more than one hour during mid- or late-term pregnancy) versus no home visiting program. Outcomes. Outcomes in Studies that Included Mothers, Newborns, and Babies up to Age Two ...
Mean gestational age at enrollment was 18.9 weeks; mean number of prenatal home visits was 8.2. In multivariable regression, ≥8 completed visits by 26 weeks compared with ≤3 visits was associated with an odds ratio 0.38 for preterm birth (95% confidence interval: 0.16-0.87), while having ≥12 total home visits compared with ≤3 visits ...
Prenatal care is an important part of staying healthy during pregnancy. Your doctor, nurse, or midwife will monitor your future baby's development and do routine testing to help find and prevent possible problems. These regular checkups are also a great time to learn how to ease any discomfort you may be having, and ask any other questions ...
We enrolled 742 pregnant, low-income women with no previous live births and randomly assigned them to receive either free transportation for prenatal care plus child development screening and referral (control; n = 514) or prenatal and infant home nurse visit (NV) plus transportation and screening (n = 228). Assessments were completed on 629 18-year-old first-born offspring to evaluate these ...
Learn about how early you can take a pregnancy test and the early signs and symptoms of pregnancy, including nausea, headaches and weight changes. Vanessa Caceres May 17, 2024
I just learned about the National Maternal Mental Health Hotline and wanted to share this free resource. Text 1-833-TLC-MAMA any time to talk with a trained counselor.
At every visit, each teen patient has time alone with a provider to discuss or ask questions about contraceptive and reproductive health concerns, regardless of whether the visit is urgent or preventive. ... Counseling is provided on all methods to prevent pregnancy using a patient-centered approach that is respectful of and responsive to ...
Today, postpartum care services in the U.S. can range from $35-$200 or more an hour for an in-home postpartum doula, mental health professionals, lactation consultants among other additional ...
Objective To ascertain and explore the views of women and their partners, giving birth in the Czech Republic, of the level of respectful or disrespectful care provided during pregnancy and early labour. Design Ethical approval was granted for a descriptive, online anonymous survey of 65 questions, with quantitative and qualitative responses. Setting The Czech Republic.The survey was completed ...