
Follow these four steps to code quickly and accurately, while reducing the need to count up data points.
KEITH W. MILLETTE, MD, FAAFP, RPh
Fam Pract Manag. 2021;28(4):21-26
Author disclosure: no relevant financial affiliations.

The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1 , 2 To ease the transition, previous FPM articles have laid out the new American Medical Association/CPT medical decision making guide 3 and introduced doctor–friendly coding templates (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), explained how to quickly identify level 4 office visits (see “ Coding Level 4 Visits Using the New E/M Guidelines ,” FPM , January/February 2021), and applied the new guidelines to common visit types (see “ The 2021 Office Visit Coding Changes: Putting the Pieces Together ,” FPM , November/December 2020).
After several months of using the new coding rules, it has become clear that the most difficult chore of coding office visits now is assessing data to determine the level of medical decision making (MDM). Analyzing each note for data points can be time-consuming and sometimes confusing.
That being the case, it's important to understand when you can avoid using data for coding, and when you can't. I've developed a four-step process for this (see “ A step-by-step timesaver ”).
The goal of this article is to clarify the new coding rules and terminology and to explain this step-by-step approach to help clinicians code office visits more quickly, confidently, and correctly.
The new evaluation and management office visit coding rules have simplified many things but are still a lot to digest, especially when it comes to counting data.
There are different levels of data and different categories within each level, which can make using data to calculate the visit level time-consuming and confusing.
By calculating total time, and then moving on to assessing problems and prescription drug management, most visits can be optimally coded without dealing with data at all.

OFFICE VISIT CODING RULES AND TERMINOLOGY
To make full use of the step-by-step process, we have to first understand the new rules, as well as coding terminology. Here is a brief summary.
Medically appropriate . Physicians and other qualified health care professionals may now solely use either total time or MDM to determine the level of service of an office visit. That means the “history” and “physical exam” components are no longer needed for code selection, which simplifies things. But your patient note must still contain a “medically appropriate” history and physical. So continue to document what is needed for good medical care.
New patient . A new patient is a patient who has not been seen by you or one of your partners in the same medical specialty and the same group practice within the past three years.
Total time and prolonged services . Total time includes all the time you spend on a visit on the day of the encounter (before midnight). It includes your time before the visit reviewing the chart, your face-to-face time with the patient, and the time you spend after the visit finishing documentation, ordering or reviewing studies, refilling medications, making phone calls related to the visit, etc. It does not include your time spent performing separately billed services such as wellness visits or procedures. Total time visit level thresholds differ for new patients vs. established patients. (See the total times in “ The Rosetta Stone four-step template for coding office visits .”)
The prolonged services code comes into play when total time exceeds the limits set for level 5 visits by at least 15 minutes.
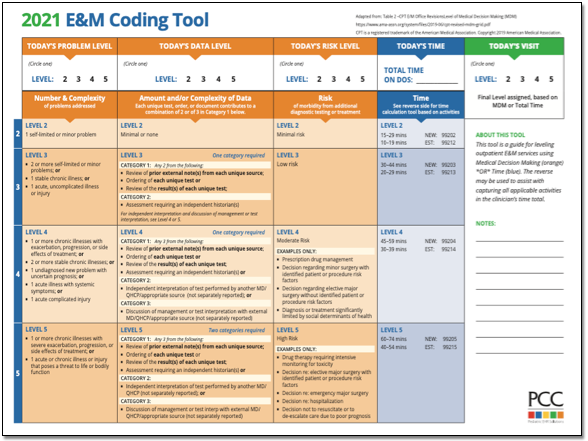
Medical decision making . MDM is made up of three components: problems, data, and risk. Each component has different levels, which correspond to levels of service (low/limited = level 3, moderate = level 4, and high/extensive = level 5). The highest level reached by at least two out of the three components determines the correct code for the level of service. MDM criteria is the same for new and established patients.
Problems addressed . This includes only the problems you address at that specific patient visit. It does not include all the patient's diagnoses and does not include problems that are exclusively managed by another clinician. Problems addressed are separated into low-complexity problems (level 3), moderate-complexity problems (level 4), and high-complexity problems (level 5). To code correctly, you need to know the coding value of the problems you address. It is helpful to think of problems in terms of levels of service (e.g., a sinus infection is usually a level 3 problem, and pneumonia or uncontrolled diabetes are usually level 4 problems).
The simplest way to summarize problems is this: Life-threatening problems are level 5; acute or chronic illnesses or injuries are level 3 or 4 depending on how many there are, how stable they are, and how complex they are; and if there's just one minor problem, it's level 2.
(For more specifics see “ What level of problem did I address? ”)
Risk . Risk is also separated into “low” (level 3), “moderate” (level 4), and “high” (level 5) categories.
Level 3 risk includes the use of over-the-counter (OTC) medications.
Level 4 risk includes the following:
Prescription drug management: starting, stopping, modifying, refilling, or deciding to continue a prescription medication (and documenting your thought process),
Social determinants of health that limit diagnosis or treatment (this is when patients' lack of finances, insurance, food, housing, etc., affects your ability to diagnose, manage, and care for them as you normally would).
Level 5 risk includes the following:
Decisions about hospitalization,
Decisions about emergency major surgery,
Drug therapy that requires intensive toxicity monitoring,
Decisions to not resuscitate or to de-escalate care because of poor prognosis.
Data analyzed . For purposes of MDM, data is characterized as “limited” (level 3 data), “moderate” (level 4 data), or “extensive” (level 5 data). But each level of data is further split into Categories 1, 2, and 3. This can make calculating data complicated, confusing, and time-consuming. Here are the data components and terms you need to know.
Category 1 data includes the following:
The ordering or reviewing of each unique test , i.e., a single lab test, panel, X-ray, electrocardiogram (ECG), or other study.
Ordering and reviewing the same lab test or study is worth one point, not two; a lab panel (e.g., complete blood count or comprehensive metabolic panel) is worth one point,
Reviewing a pertinent test or study done in the past at your own facility or another facility,
Reviewing prior external notes from each unique source, including records from a clinician in a different specialty or from a different group practice or facility as well as each separate health organization (e.g., reviewing three notes from the Mayo Clinic is worth one point, not three, but reviewing one note from Mayo and one from Johns Hopkins is worth a total of two points),
Using an independent historian, which means obtaining a history from someone other than the patient, such as a parent, spouse, or group home staff member. (This is included in Category 2 for level 3 data, but falls into Category 1 for level 4 and 5 data.)
Category 2 data includes the following:
Using an independent historian (for level 3 data only),
Independent interpretation of tests, which is your evaluation or reading of an X-ray, ECG, or other study (e.g., “I personally reviewed the X-ray and it shows …”) and can include your personal evaluation of a pertinent study done in the past at your or another facility. It does not include reviewing another clinician's written report only, and it does not include studies for which you are also billing separately for your reading.
Category 3 data includes the following:
Discussion of patient management or test interpretation with an external physician, other qualified health care professional, or appropriate source. An external physician or other qualified health care professional is someone who is not in your same group practice or specialty. Other appropriate sources could include, for example, consulting a patient's teacher about the patient's attention deficit hyperactivity disorder.
A STEP-BY-STEP TIMESAVER
The majority of office visits can be optimally coded by using time or by looking at what level of problems were addressed (see Steps 1 and 2 below) and whether a prescription medication was involved.
A level 3 problem can be coded as a level 3 visit if you address it with an OTC or prescription medication. A level 4 problem can be coded as a level 4 visit if you order prescription medication or perform any other type of prescription drug management (modifying, stopping, or deciding to continue a medication). Most level 2 and level 5 office visits are straightforward, and most level 5 visits will be coded by time. They will typically be visits in which you address multiple problems or complicated problems and the total time exceeds 40 minutes for established patients. This is much more common than seeing critically ill patients who may require admission, which is another level 5 scenario. The few remaining patient visits that have not already been coded require analyzing data (Steps 3 and 4). (See “ The Rosetta Stone four-step template for coding office visits .”)
Step 1: Total time . Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to Step 2.
Step 2: “Problems plus.” Don't be afraid to move on from time-based coding if you believe you performed a higher level visit using MDM. Many visits can be coded with MDM just by answering these two questions: What was the highest-level problem you addressed during the office visit? And did you order, stop, modify, or decide to continue a prescription medication?
If you addressed a level 2 problem and your total time was less than 20 minutes (or less than 30 for a new patient), then code level 2.
If you addressed a level 3 problem, plus you recommended an OTC medication or performed prescription drug management, then code level 3.
If you addressed a level 4 problem, plus you performed prescription drug management, then code level 4.
Chronic disease management often qualifies as level 4 work. For documentation, think “P-S-R”: problem addressed, status of the problem (stable vs. unstable), and prescription drug management (Rx). This trio should make it clear to coders, insurance companies, and auditors that level 4 work was performed.
For instance, if a patient has controlled hypertension and diabetes and you document that you decided to continue the current doses of losartan and metformin, that's level 4 (two stable chronic illnesses plus prescription drug management). If you see a patient with even one unstable chronic illness and document prescription drug management to address it, that's also level 4.
For a level 5 problem, if you see a really sick patient and decide to admit or consider admission (and you document your thought process in your note), then code level 5.
By starting with total time and, if necessary, moving on to “problems plus,” you will probably be able to optimally code 90% of your office E/M visits. But on the rare occasions when you see a patient for level 4 or 5 problems for less than the required time and don't do any prescription drug management, you may have to proceed to Steps 3 and 4.
Step 3: Level 4 problem with simple data or social determinants of health concerns . Code level 4 if you saw a patient for a level 4 problem and did any of the following:
Personally interpret a study (e.g., X-ray),
Discuss management or a test with an external physician,
Modify your workup or treatment because of social determinants of health.
Step 4: Level 4 or 5 problem with complex data . If you saw a patient for a level 4 problem and still haven't been able to code the visit at this point, you have to tally Category 1 data points:
Review/order of each unique test equals one point each,
Review of external notes from each unique source equals one point each,
Use of an independent historian equals one point.
Once you reach three points, code it as level 4.
For a level 5 problem, if you see a really sick patient, order/interpret an X-ray or ECG, and review/order two lab tests, then code level 5.
Following these steps should allow you to quickly identify the optimal level to code most any E/M office visit (for pre-op visits, see “ Coding pre-ops template .”)
Here's a catchy rhyme to remember the basic outline of the steps:
To finish fast ,
code by time and problems first ,
and save data for last .
By mastering the new coding rules and terminology and applying this four-step approach, you can code office visits more quickly, accurately, and confidently — and then spend more time with your patients and less time at the computer.
CPT Evaluation and Management (E/M) Office or Other Outpatient and Prolonged Services Code and Guideline Changes . American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
E/M Office Visit Compendium 2021. American Medical Association; 2020.
Table 2 – CPT E/M office revisions level of medical decision making. American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf
Continue Reading

More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

List With Office Visit CPT Codes (New & Established Patients)
The CPT codes for office visits can be found in the CPT manual; under range CPT 99202 until 99205 for office visits of new patients . For office visits of established patients, you can use range 99211 to CPT code 99215. We also included CPT 99070 in case you need to bill extra supplies/materials for office visits and CPT code 99072 if extra staff and supplies were needed during a Public Health Emergency.
CPT Code 99070
Long description of CPT 99070 : Supplies and materials [except spectacles] provided by the physician or other qualified health care professional over and above those usually included with the office visit or other services rendered [list drugs, trays, supplies, or materials provided].
Short description: Extra supplies/materials for office visit.
CPT Code 99072
Long description of CPT 99072 : Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service[s], when performed during a Public Health Emergency, as defined by law, due to respiratory-transmitted infectious disease.
Short description: Extra supplies and staff time for office visits during Public Health Emergency.
CPT Code 99202
Long description of CPT 99202 : Office or other outpatient visit for the evaluation and management of a new patient , which requires a medically appropriate history and/or examination and straightforward medical decision making. When using time for code selection, 15-29 minutes of total time is spent on the date of the encounter.
Short description: 15-29 minute office visit for new patient evaluation and management.
CPT Code 99203
Long description of CPT 99203 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.
Short description: 30-44 minute office visit for new patient evaluation and management.
CPT Code 99204
Long description of CPT 99204 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using time for code selection, 45-59 minutes of total time is spend on the date of the encounter.
Short description: 45-59 minute office visit for new patient evaluation and management.
CPT Code 99205
Long description of CPT 99205 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code+ selection, 60-74 minutes of total time is spent on the date of the encounter.
Short description: 60-74 minute office visit for new patient evaluation and management.
CPT Code 99211
Long description of CPT 99211 : Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional
Short description: Short office visit for established patient management.
CPT Code 99212
Long description of CPT Code 99212 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using time for code selection, 10-19 minutes of total time spent on the date of the encounter.
Short description: 10-19 minute office visit for established patient management.
CPT Code 99213
Long description of CPT 99213 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 20-29 minutes of total time is spent on the date of the encounter.
Short description: 20-29 minute office visit for established patient management.
CPT Code 99214
Long description of CPT 99214 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision-making. When using time for code selection, 30-39 minutes of total time is spend on the date of the encounter.
Short description: 30-39 minutes office visit for established patient management.
CPT Code 99215
Long description of CPT 99215 : Office or other outpatient visit for the evaluation and management of an established patient, which requires medically appropriate history and/or examination and high level of medical decision making. When using time for code selection, 40-54 minutes of total time is spent on the date of the encounter.
Short description: 40-54 minutes office visit for established patient management .
https://www.aapc.com/codes/cpt-codes-range/99211-99215/
https://www.aapc.com/codes/cpt-codes-range/99202-99205/
https://www.aapc.com/codes/cpt-codes/99070
https://www.aapc.com/codes/cpt-codes/99072
Similar Posts
How to use cpt code 01938.
cpt 01938 describes the anesthesia services provided by a healthcare professional during percutaneous image-guided injection, drainage, or aspiration procedures on the lumbar or sacral spine or spinal cord. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, and examples of cpt 01938. 1. What is cpt 01938?…
How To Use CPT Code 81252
CPT 81252 describes the analysis of the full gene sequence for GJB2, also known as gap junction protein, beta 2, 26kDa, connexin 26. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 81252? CPT 81252 is used…
How To Use CPT Code 29855
CPT 29855 describes the arthroscopically aided treatment of a tibial fracture, specifically the proximal (plateau) region. This article will cover the official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 29855? CPT 29855 is used to describe a specific procedure known as arthroscopically…
How To Use CPT Code 26450
CPT 26450 describes a surgical procedure known as tenotomy, specifically the open division of a flexor tendon in the palm. This article will provide an overview of CPT code 26450, including its official description, the procedure itself, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code…
How To Use CPT Code 85378
CPT 85378 describes the qualitative or semiquantitative testing of fibrin degradation products, specifically D-dimer, in patient blood or plasma. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 85378? CPT 85378 can be used to describe the…
How To Use CPT Code 49999
CPT 49999 describes a procedure performed on the peritoneum and omentum in the abdomen that does not have a specific code. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 49999? CPT 49999 can be used to…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.

Chart, Code, and Bill for E&M Office Visits
- See 6 Related Articles
- Share this article
Upon completion of encounters, a clinician selects billing codes. They often select an “Evaluation and Management” or E&M code, either for new or established patients. This is sometimes called the “office visit” code. E&M code selection is based on medical decision making and the amount of time spent.
This article collects resources and guidelines for E&M office visits, with some tips on implementation in PCC EHR.
On January 1st, 2021, the guidelines for coding and billing an office visit changed significantly.
Procedure Code Guidance: The procedure code recommendations in this article are intended only as examples. You should consult the AMA’s CPT Coding Guide and work with your insurance payers to verify what codes you should use on claims. Your practice updates and maintains your procedure list, codes, and prices in the Procedures table in the Table Editor on your PCC system.
- 1 Why is E&M Code Selection Important to a Pediatric Practice?
- 2.1 Select a Code Based on Medical Decision Making
- 2.2 Select a Code Based on Time
- 3 PCC’s 2021 E&M Coding Tool
- 4 Watch PCC 2021 E&M Coding Videos
- 5 Configure PCC EHR to Support Your Clinicians and Billers for E&M Level Selection in 2021
- 6 Additional Resources and Guides
- 7.1 Questions and Answers
Why is E&M Code Selection Important to a Pediatric Practice?
E&M services make up the bulk of the work you do as a pediatrician. They represent the cognitive work, information gathering, and decision making that goes into a patient encounter. A pediatrician’s time with patients is going to be classified as E&M more than often than with other medical specialties. Because most of the work you do falls under the umbrella of E&M, it’s vital that you code those services correctly. Many pediatricians under-code their encounters, resulting in significant lost revenue for their practice.
Coding your E&M services correctly is not only a matter of revenue. The requirements for documenting each level are also intended to provide appropriate and adequate information for continuity of care.
How Do I Select an E&M Code in 2021?
For encounters that occur after December 31st, 2020, a clinician no longer uses history or physical exam performed during the encounter as criteria for code selection. Instead, they select a code based on either medical decision making or time spent practicing care for the patient on the day of the visit.
Here’s a brief explanation of how you select a billing code level for an “evaluation and management” or “Office Visit” after January 1st, 2021. These guidelines apply to common visit billing codes, such as 99212, 99213, 99214, or 99215, as well as to the selection of codes 99202 through 99205.
Select a Code Based on Medical Decision Making
You can base your visit level code on medical decision making, which is comprised of three elements:
Problems Addressed: The number of problems you addressed for the patient during the day of the encounter.
Items Reviewed: The tests, chart information, and other data you reviewed in relation to the problems addressed today.
Risk: The level of risk presented to the patient.
Select a Code Based on Time
You can base your visit level code selection on the total time that the rendering clinician spent on the patient that day. That can include the time the pediatrician spent before, during, and after the actual encounter.
PCC’s 2021 E&M Coding Tool
PCC’s Jan Blanchard (CPC, CPEDC) developed a printable guide to E&M Coding in 2021.
Watch PCC 2021 E&M Coding Videos
You can get a quick understanding of how to level your E&M visits in 2021 by watching these videos:
- 2021 Evaluation and Management Updates: What changed? This 15 minute video explains the new way of selecting E&M codes in context with how you coded sick office visits before.
- PCC’s 2021 E&M FAQ&A: Frequently asked questions, and a live Q&A about 2021 E&M leveling.
- The Impact of 2021 E&M Coding Changes on Pediatrics: Learn about the E&M coding changes in context, and then hear PCC’s ideas about how these changes will affect the business of pediatrics.
- Pediatric Management Institute’s September COVID-19 Webinar: During the September 2020 session of the PMI’s ongoing webinar series, The Business Impact Of COVID19 On Pediatric Practices , this topic is covered along with other current topics. This recorded live webinar includes some additional Q&A.
- Attend a 2021 E&M Coding Workshop: Join PCC's Jan and come prepared with at least one complex (99214, 99215, 99205) E&M encounter note for review and/or analysis. Registration is required for this workshop and will be hosted on Zoom so that you, Jan, and your colleagues can collaborate effectively. ( Watch the Last Session )
- Attend a PCC Web Lab: PCC’s Jan Blanchard (CPC, CPEDC) hosts monthly web labs on pediatric practice management, billing, and coding.
- Watch Recorded Web Labs and More
Configure PCC EHR to Support Your Clinicians and Billers for E&M Level Selection in 2021
Your practice can add fields to your chart note protocols in order to track time spent before, during, and after the encounter by the clinician. You can also track the number of problems addressed, items reviewed for the problems, and the level of risk present.
As an example, this sample chart note protocol includes components designed to quickly note problems, time and risk.
For help customizing your protocols, check out Configure Chart Note Protocols , and get in touch with PCC Support for assistance.
Additional Resources and Guides
PCC has developed helpful blog posts that cover how to get started, frequently asked questions, and more.
Evaluate Your Practice's E&M Habits and Patterns: Your Practice Vitals Dashboard , available from within PCC EHR, provides a number of metrics, tools and recommendations related to E&M coding included on the “E&M Coding Distribution” measure.
Confessions of a Pediatric Practice Management Consultant: PCC’s Chip Hart runs a blog and podcast, covering many topics related to practice management, including E&M coding. You can find it here .
- E&M 2021 Updates: Preparing Your Pediatric Practice
- E&M Updates in 2021: Frequently Asked Questions
- AAP FAQ: E&M 2021 coding questions and answers by the American Academy of Pediatrics.
- AAP MDM Grid: A direct link to the AAP’s chart which illustrates levels of medical decision making. It includes several useful examples. (AAP hosts this file here .)
- MDM Tracker: An online tool for selecting visit level based on medical decision making in 2021.
Questions and Answers on Interpreting E&M 2021 Guidelines
PCC’s Jan Blanchard works with pediatric practices to help them interpret coding guidelines. Read below to see a selection of the 2021 E&M questions she’s received along with answers based on her current interpretation of the guidelines. As with any new way of doing things, this is a work-in-progress and will be updated as we learn more. These Q&As were updated on 2021-01-08 .
Questions and Answers
- Where can I find PCC’s 2021 MDM Tool? Here it is: PCC’s 2021 E&M Coding Tool .
- Where can I find the online MDM calculator Chip Hart shared? You can find it on the Confessions of a Pediatric Practice Management Consultant blog post entitled “Free E&M Medical Decision Making Calculator” .
CPT defines systemic symptoms this way: “Acute illness with systemic symptoms: An illness that causes systemic symptoms and has a high risk of morbidity without treatment. For systemic general symptoms, such as fever, body aches, or fatigue in a minor illness that may be treated to alleviate symptoms, shorten the course of illness, or to prevent complications, see the definitions for self-limited or minor problem or acute, uncomplicated illness or injury. Systemic symptoms may not be general but may be single system. Examples may include pyelonephritis, pneumonitis, or colitis.” (p12-14 2021 CPT Manual)
Fever had become a mainstay of complexity expression in E&M documentation. In 2021, not all fevers meet the definition of a systemic symptom. AMA says that in cases where the fever is a “general symptom in a minor illness”, it is *not* systemic. So using it to express visit complexity becomes a case-by-case determination for 2021. Things like age and other risks will be determining factors that clinicians will have to consider when they decide this point.
Furthermore, the AAP has interpreted the AMA’s position to be that you may not consider tests performed in your office in your MDM level determination. This interpretation is under review.
Maybe. “Problems” are the units of determination for MDM. So, if you treat three problems in a visit, but there are five ICDs listed, the ICDs do not inherently support higher complexity leveling. Some ICDs are reported because they represent circumstances and/or problems which complicate care but which are not specifically addressed at that visit. Documenting the role that those existing problems play in your thinking could support assigning higher Problem values to what *is* addressed.
- Can I really get credit every time a parent or guardian contributes history to a visit? Maybe. If you feel confident that the contribution they made is required for appropriate care to be rendered, yes. Document the reason for their perspective being necessary if it is not obvious. For example, little ones who can’t speak for themselves obviously require someone to give their history. But for teens, the necessity of another perspective in, say, behavioral or social concerns where objective input is valuable, document a statement to that effect and take the independent historian point(s).
Per the Elements of Medical Decision Making grid published by AMA in CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes, an example of Moderate risk of morbidity from additional diagnostic testing or treatment is “Diagnosis or treatment significantly limited by social determinants of health”. I interpret these references to suggest that any SDoH which significantly limits the patient’s ability to carry out the clinician’s plan meets the Level 4 risk requirement.
According to the U.S. Department of Health, Social Determinants of Health are economic and social conditions that influence the health of people and communities. Their examples include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
Some of these may be reported using ICD codes found in “Persons with potential health hazards related to socioeconomic and psychosocial circumstances Z55-Z65”
- Z55 Problems related to education and literacy
- Z56 Problems related to employment and unemployment
- Z57 Occupational exposure to risk factors
- Z59 Problems related to housing and economic circumstances
- Z60 Problems related to social environment
- Z62 Problems related to upbringing
- Z63 Other problems related to primary support group, including family circumstances
- Z64 Problems related to certain psychosocial circumstances
- Z65 Problems related to other psychosocial circumstances
The new MDM focus on visit leveling represents less subjectivity in discerning which parts of a service were part of the well care and which were part of the sick care.
- Do I need to document in the note the exact amount of time spent on each activity, or is it ok to just document total time? Full day totals are permissible, but I would feel better seeing at least time segments. Rough estimates for segments would do, but to expect that human brains can recreate a day’s worth of timed detail accurately for work that gets interrupted and broken up and then wrapped up after everyone else has gone home is a stretch which can be avoided.
- Is there still a Level 1 visit for nurse-only visits? Yes, for established patients only, a Level 1 nurse visit can be reported using 99211. New patient level 1 code 99201 expires on 12/31/20 and is not reportable thereafter. This is due to the identical MDM requirements for both 99201 and 99202. By 2021 standards, 99201 becomes redundant to 99202.
- If I continue to chart after hours, can I add that time for the purposes of leveling the visit? Yes. Caveat: The only after hours charting time (or any other clinical activity time) you may include in your billed time is the time spent *on the date of service*. If you chart any part of yesterday’s visit today, you may bill by time but you cannot include the time you spent today in the total you use for choosing your level. For example, if on Monday you see an established patient and spend 5 minutes reviewing records, 10 minutes in a visit, 5 minutes on a results call Monday night and 10 minutes charting on Tuesday morning, you may only bill a level 3 visit using Monday time: 5+10+5=20 minutes; Tuesday’s 10 minutes cannot count toward the leveling.
Discussions around this continue, but currently you should not expect to level using data points for test and labs you bill.
- Are a CBC and differential counted as more than 1 lab? Or for example COVID-19/Flu/RSV combo - is that 1 test or 4 tests? It depends on the number of CPTs. If CBC and differential are one CPT, it is one data point for either ordering or reviewing. If the COVID-19/Flu/RSV combo is one CPT, one point is its data value.
- Could I count one of several screenings towards data reviewed and bill for the other and not be double-dipping? This is not in the spirit of the requirement, but is still under discussion. Billing effects are impossible to explore here. The sheer variety of payers and policies means the outcome can not be predicted. Furthermore, carrier behavior makes predictions of future claim determinations little more than a guessing game.
- Do I get credit if some historians are in office and others participate over facetime, phone, etc., for the same visit? Yes. There is no cumulative credit for historians, but if someone other than the patient is required to participate that requirement is met.
- If you use a formal screen for SDoH that is scored and payable, then you can’t count that screening towards MDM, correct? Currently, that is correct.
Also, the question of whether in-house tests and labs may be used for data credit remains unanswered. I am undecided on this as yet and will count on the clinicians with whom I review encounters to help me arrive at a position on this point in future.
- We do our huddle and "run the schedule" (i.e. review referrals, lab results, vaccines, and consult notes) the day *before*, not the day of! Can we count that time when leveling each of those encounters? No. Currently, the only “billable” time is that spent by the clinician for that patient on the service date.
CPT 2021 is light on guidance on this point. “Undiagnosed new problem with uncertain prognosis: A problem in the differential diagnosis that represents a condition likely to result in a high risk of morbidity without treatment. An example may be a lump in the breast…” The AAP offered an additional example of a potentially malignant lesion in the Feb 2020 issue of the Coding Newsletter.
- If we bill for one Vanderbilt, could we then claim MDM credit for the ones from other sources? My sense of this is that doing so is *not* in the spirit of the guideline. Additionally, performing a service and not billing for it will run afoul of many insurance contracts. Also, please see above for information about Data credit for in-house labs and tests.
Example: Rash (insect bite) + been a little constipated (give some prune juice), been having stomach aches (few questions to make sure it’s nothing worrisome, asked to schedule another visit to evaluate further)…
Yes, but MDM is based on significance, not the number of problems. The total number of problems does not necessarily increase the credit you can claim for complexity in the Number and Complexity of Problems Addressed element. Rather, the most complex problem addressed (Minimal, Low, Moderate, High) in a given encounter typically represents the level of “problems addressed” which should be used for leveling. Exceptions include self-limited, minor problems (1 = Minimal while 2 = Low) and stable chronic illnesses (1 = Low, 2 = Moderate).
- Can concussion be considered an acute complicated injury - a head injury that gave other systemic symptoms? Described that way, absolutely. Be sure to familiarize yourself with the AMA’s definition of Systemic Symptoms.
From the AMA: “Trained clinicians apply common language usage meanings to terms such as high, medium, low, or minimal risk and do not require quantification for these definitions (though quantification may be provided when evidence-based medicine has established probabilities). For the purposes of MDM, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes MDM related to the need to initiate or forego further testing, treatment, and/or hospitalization.”
From the AMA: “… decision about hospitalization includes consideration of alternative levels of care…Examples may include a psychiatric patient with a sufficient degree of support in the outpatient setting or the decision to not hospitalize a patient with advanced dementia with an acute condition that would generally warrant inpatient care, but for whom the goal is palliative treatment.”
For example, if PCC EHR automatically records your time with a chart open, you would be required to close and reopen every chart every time you were interrupted while charting in order for it to be accurate. If you had to actively click a button to stop and start a timer, it would be an ever-present timer that required their attention. Users shared this would be distracting at best and annoying at worst. Most users were happier to state their own estimates of how much time was spent, either in total or in segments to be used for totaling when they were sure services were complete for the whole day.
Related Articles
- Here are some related articles in Other Pediatric Practice Resources > Coding and Documentation :
How to Code for Immunizations and Administration
ICD-10 Training Resources
Diagnostic Code Sets (SNOMED-CT, ICD-10, ICD-9) in PCC’s Software and Services
CPT II in PCC
PCC’s Billing Drop-In Sessions
2021 Evaluation & Management Workshop (11-17)
- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.
Video Visits Billing, Coding and Regulations Information
Many patients have utilized telemedicine for medical care during the COVID pandemic and will continue to seek this option going forward. These resources will help refine and improve your delivery of virtual care, and practical implementation tips are offered below.
E/M and Other Medicare Allowed Services
This is a list of eligible CPT/HCPCS codes .
- Use POS code 10 for telehealth services provided in the patient's home - The location where health services and health related services are provided or received, through telecommunication technology. Patient is located in their home (which is a location other than a hospital or other facility where the patient receives care in a private residence) when receiving health services or health related services through telecommunication technology. (This code is effective January 1, 2022, and available to Medicare April 1, 2022.)
- Use POS 02 for telehealth services provided other than in patient's home - The location where health services and health related services are provided or received, through telecommunication technology. Patient is not located in their home when receiving health services or health related services through telecommunication technology. (Description change effective January 1, 2022, and applicable for Medicare April 1, 2022.)
- Modifier -95 should not be used with virtual check-ins (G2012) or the digital evaluations (99421-99423). It is for use with all other telehealth codes that use synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system.
- During the current PHE, telehealth E/M levels can be based on Medical Decision Making (MDM) OR time (total time associated with the E/M on the day of the encounter). Likewise, CMS has also removed any requirements regarding documentation of history and/or physical exam in the medical record for Telehealth visits.
- -GQ: Clinicians participating in the federal telemedicine demonstration programs in Alaska or Hawaii must submit the appropriate CPT or HCPCS code for the professional service along with the modifier GQ, “via asynchronous telecommunications system.”
- -GO: Use of telehealth for purposes of diagnosing stroke.
- Note: Medicare stopped the use of modifier -GT in 2017 when the place of service code 02 (telehealth) was introduced. However, private payer may still be using the modifier -GT.
Virtual Check-In
This is a set of telehealth-specific codes for the following use-cases:
- Any chronic patient who needs to be assessed as to whether an office visit is needed.
- Patients being treated for opioid and other substance-use disorders.
- Can be any real-time audio (telephone), or "2-way audio interactions that are enhanced with video or other kinds of data transmission."
- Nurse or other staff member cannot provide this service. It must be a clinician who can bill E&M services.
- If an E&M service is provided within the defined time frames, then the virtual check-in is bundled in that E&M service. It would be considered pre- or post-visit time of the associated E&M service and thus not separately billable.
- Should be initiated by the patient since a copay is required. Verbal consent to bill and documentation is required.
- No modifier needed as these are technology based codes.
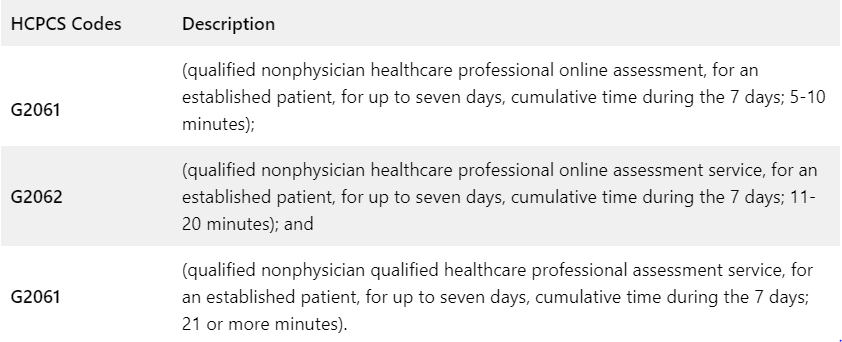
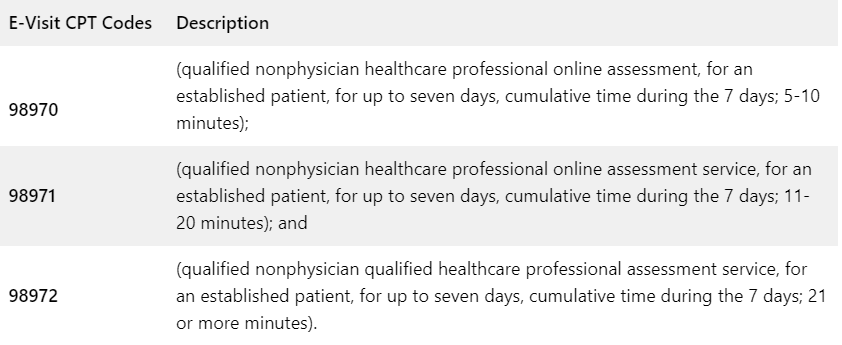
Online Digital Evaluation and Management (E/M)
Telehealth-specific codes for the following use-cases:
- Given the temporary approval of E/M visits via telehealth, these online codes would primarily be used for patient interactions via a portal.
- Can be done synchronously and asynchronously and audio/video phone can be used (but not a traditional telephone).
- The patient can initiate a virtual check-in, the practice can let the patient know about their options. If the patient calls back within 7 days, then the time from the virtual check-in can be added to the digital E/M code and only the digital E/M code is billed.
- If the patient initiates a call to the physician office this would qualify for the remote check-in code (G2012), the time for the remote (virtual) check-in can be counted toward 99421-3 only if and when the patient calls back, so it is important to document the time. (See CPT book for further details regarding when the 7 days begins, how to count time, which “qualified non-physician health professionals” it applies to, and other documentation requirements.)
- Must be patient initiated.
- Cost sharing applies.
- Use only once per 7-day period. If the patient presents a new, unrelated problem during the 7-day period of an online digital E/M service, then the time is added to the cumulative service time for that 7-day period.
- Clinical staff time is not calculated as part of cumulative time.
- Service time must be more than 5 minutes.
- Do not count time otherwise reported with other services.
- Do not report on a day when the physician or other qualified health care professional reports other E/M services.
- Do not report when billing remote monitoring, CCM, TCM, care plan oversight, and codes for supervision of patient in home, domiciliary or rest home etc. for the same communication[s]).
- Do not report for home and outpatient INR monitoring when reporting 93792, 93793.
Private Payer and State Policies
Many states have issued their own public health emergencies, and some have ended theirs, which results in changes to Medicaid, private payer, and licensure for telehealth.
- The Center for Connected Health Policy (CCHP) is an excellent resource to keep up with state regulations and has two toolkits that track COVID-19 Telehealth Coverage Policies and COVID-19 Related State Actions , which include Medicaid clarification, waivers, and telehealth guidance, prescription and consent waivers, private payer requirements, and cross-state licensing.
- The Alliance for Connected Care also has a chart showing state changes to licensure, coverage, and other changes during COVID-19.
- Full listing of all blanket waivers and flexibilities related to provider enrollment, telehealth, 1135 waivers, and other changes resulting from the COVID-19 public health emergency.
Other Resources
Many Medicare restrictions related to virtual visits have been lifted during the COVID public health emergency. ACP will update this information when the federal PHE ends. Some states have already ended their PHE.
Medicare policies during the emergency:
- Patients can be at home and non-HIPAA compliant communication technology is allowed.
- Practices are allowed to waive cost sharing (copays and deductibles) for all telehealth services All E/M and other services that are currently eligible under the Medicare telehealth reimbursement policies are included in this waiver. This is a list of eligible CPT/HCPCS codes , including which codes are allowed to use audio-only telephone.
- New or established patients.
- Rural and site limitations are removed.
- CMS has issued additional guidance regarding flexibilities specific to FQHCs and RHCs.
- Informed Consent for Telehealth: Although it is not always required, it is important that patients understand the risks and benefits of using telehealth. AHRQ has a simple, customizable consent form and how-to guidance for clinicians on how to explain telehealth. Document verbal consent prior to each telehealth visit until you can receive a signed consent (either digitally or on paper) from the patient.
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

An official website of the United States government
The .gov means it’s official. A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Billing and coding Medicare Fee-for-Service claims
Read the latest guidance on billing and coding Medicare Fee-for-Service (FFS) telehealth claims.
On this page:
Telehealth codes covered by medicare, coding claims, common telehealth billing mistakes, more information about ffs billing.
Medicare added over one hundred CPT and HCPCS codes to the list of telehealth services .
Telephone visits and audio-only telehealth
Medicare is temporarily waiving the audio-video requirement for many telehealth services. Codes that have audio-only waivers are noted in the list of telehealth services .
Place of Service codes
When billing telehealth claims, it is important to understand the place of service (POS) codes as it affects reimbursement.
The POS code (PDF) explains where the provider and patient are located during the telehealth encounter. There are currently two POS codes:
- POS 02: Telehealth provided other than in patient's home. Patient is not located in their home when receiving health services or health related services through telecommunication technology.
- POS 10: Telehealth provided in patient's home. Patient is located in their home (which is a location other than a hospital or other facility where the patient receives care in a private residence) when receiving health services or health related services through telecommunication technology.
Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience.
Incorrect billing codes
More than 100 telehealth services are covered under Medicare. However, some CPT and HCPCS codes are only covered temporarily.
Using the wrong code can delay your reimbursement. This can happen for a variety of reasons, such as a misunderstanding of what code applies to what service or input error.
Stay up to date on the latest Medicare billing codes for telehealth to keep your practice running smoothly.
Documentation
Post-visit documentation must be as thorough as possible to ensure prompt reimbursement.
While there are many similarities between documenting in-person visits and telehealth visits, there are some key factors to keep in mind.
Patient consent
Make a note of whether the patient gave you verbal or written consent to conduct a virtual appointment.
Code categories
Telephone codes are required for audio-only appointments, while office codes are for audio and video visits.
Time of visit
A common mistake made by health care providers is billing time a patient spent with clinical staff. Providers should only bill for the time that they spent with the patient.
Store-and-forward
Many states require telehealth services to be delivered in “real-time”, which means that store-and-forward activities are unlikely to be reimbursed. You can find information about store-and-forward rules in your state here .
Originating sites and distant sites
Learn about eligible sites as well as telehealth policies specific to Federally Qualified Health Centers and Rural Health Clinics.
If you are looking for detailed guidance on what is covered and how to bill Medicare FFS claims, see:
- Billing for Telehealth Encounters: An Introductory Guide on Fee-for-Service (PDF) – from the National Policy Center - Center for Connected Health Policy
Medicaid and Medicare billing for asynchronous telehealth
Learn how to bill for asynchronous telehealth, often called “store and forward".
Billing Medicare as a safety-net provider
Medicare billing and coding guidelines on telehealth for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs).
- Medical Billing Services
- Podiatry Billing Services
- Pain Management Billing Services
- ASC - Surgery Center Billing Services
- Physical Therapy Billing Services

- 5 Star Billing
- Billing Software
- 1st Providers Choice
- eClinicalWorks
- Greenway Prime Suite
- IMS - Intelligent Medical Software
- NextGen -Meditouch
- Office Ally
- Practice Fusion
- SIS - Surgical Information Systems
Best Guide to E-Visit Documentation, Coding, and Billing

Categories: Coding , CPT Codes , Medical Billing
Tags: billing code , coding , cpt code tips , e visits in healthcare , medical billing
The American Academy of Family Physicians (AAFP) encourages safe, secure online interactions between physicians and patients, such as electronic visits or “virtual e-visits.” In non-emergency situations, e-visits can substitute for office visits with primary care providers. It is a fast and easy online procedure for patients to receive a diagnosis and treatment plan.
This article will give you the best guide to e-visit documentation, coding, and billing.
What Should Providers Know About E-visits?
An encounter must meet the following criteria to be considered an e-visit:
- The practice must have a well-established relationship with its patients.
- E-visits require patient consent and a communication request.
- The patient must initiate non-face-to-face electronic communication. For example, patient portal systems.
- Patients must not have seen an office visit to a physician or therapist for the same clinical concern in the past seven days.
- It is only possible to report e-visits every seven days.
- An e-visit is not the same as typical therapy sessions.
For e-visits, the following documentation requirements are needed:
- The main complaint with all evaluation and management services (E/M).
- The specifics of treatments, assessment of diagnoses or symptoms, evaluation, and conversation.
- An official patient consent record is backed up by a signature and captured in the clinical note. Moreover, e-visit software platforms accept scanned copies of signed consents. Some systems allow electronic signatures.
- The total time recorded over the seven days supporting the billable service.
List of Current Procedural Terminology (CPT) Codes That Require Providers to Follow Policies Set by Payers
The codes for online digital evaluation services (e-visits) used by doctors are complex. Below are the codes used:
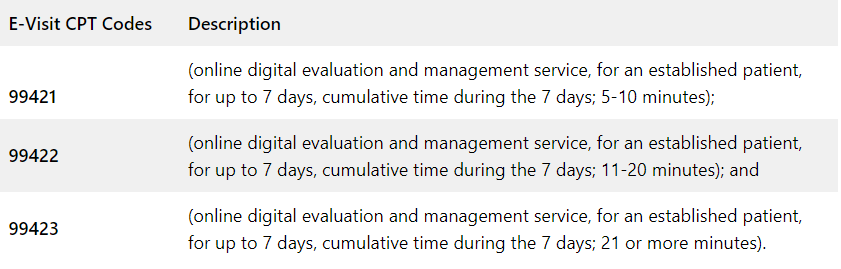
Medicare uses the following HCPCS codes and descriptors for qualified non-physician professionals for its online digital evaluation service (e-visit):
Private payers and workers’ compensation are using the following online digital evaluation service (e-visit) CPT codes and descriptors:
Do’s and Don’ts in Billing E-Visits
When the following conditions are met, you can bill an e-visit:
- The provider establishes a relationship with the patient.
- Response time by the provider is longer than five minutes.
- A provider responds through the patient portal to a message initiated by the patient.
- A visit meets the 2021 E/M guidelines.
- It has been seven days since the clinician last saw the patient.
- There is no global period for the same or similar condition for the patient.
- In this case, the provider is making a clinical decision that would normally be performed in the office (e.g., medication dose adjustment, ordering a test, or prescribing a new medication).
- A patient has consented to the e-visit and understands that he may be billed.
- For online digital E/M services, the service period includes all related work done within seven days by the reporting individual and other registered healthcare providers (RHPs) in the same group practice.
- The 7-day period begins when the reporting provider reviews the patient’s inquiry personally for the first time.
- A new/unrelated problem from the patient arises within seven days of the previous E/M visit for a different issue.
Do not bill an E-visit in the following situations:
- During the 7-day period, the provider may bill for other separately reported services (such as care management, INR monitoring, remote monitoring, etc.)
- The same or similar condition was billed to the patient for an e-visit within the past 7 days.
- The patient inquires about a surgical procedure that happens during the surgery’s postoperative period (global).
- Providers are simply disseminating results, processing medication requests, or scheduling appointments (for billing, E/M services must be performed).
- A separate face-to-face E/M service (either in person or via telehealth) happens (included in the E/M) during the 7-day period of the e-visit.
- Besides clinical staff time, only provider time can be included.
The AAFP published an algorithm in response to the growing number of virtual visits. It was developed by James Dom Dera, MD, FAAFP, to determine which code should be used for virtual services.
Tap Into Our Expertise
At 5 Star Billing Billing Services Inc , we offer the highest level of performance for high-quality medical billing and coding. Save your money by outsourcing to a professional billing service.
Schedule a call with our experts today!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- Phone: 1-480-999-0180
- Terms of Use
- Privacy Policy
- Copyright Notice
- © 2024 5 Star Billing Services, Inc.

Medicare Wellness Visits Back to MLN Print November 2023 Updates
What’s Changed?
- Added information about monthly chronic pain management and treatment services
- Added information about checking for cognitive impairment during annual wellness visits
- Added information about Social Determinants of Health Risk Assessments as an optional element of annual wellness visits

Quick Start
The Annual Wellness Visits video helps you understand these exams, as well as their purpose and claim submission requirements.
Medicare Physical Exam Coverage
Initial Preventive Physical Exam (IPPE)
Review of medical and social health history and preventive services education.
✔ New Medicare patients within 12 months of starting Part B coverage
✔ Patients pay nothing (if provider accepts assignment)
Annual Wellness Visit (AWV)
Visit to develop or update a personalized prevention plan and perform a health risk assessment.
✔ Covered once every 12 months

Routine Physical Exam
Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
✘ Medicare doesn’t cover a routine physical
✘ Patients pay 100% out-of-pocket
Together we can advance health equity and help eliminate health disparities for all minority and underserved groups. Find resources and more from the CMS Office of Minority Health :
- Health Equity Technical Assistance Program
- Disparities Impact Statement
Communication Avoids Confusion
As a health care provider, you may recommend that patients get services more often than we cover or that we don’t cover. If this happens, help patients understand they may have to pay some or all costs. Communication is key to ensuring patients understand why you’re recommending certain services and whether we cover them.

Initial Preventive Physical Exam
The initial preventive physical exam (IPPE), also known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. We pay for 1 IPPE per lifetime if it’s provided within the first 12 months after the patient’s Part B coverage starts.
1. Review the patient’s medical and social history
At a minimum, collect this information:
- Past medical and surgical history (illnesses, hospital stays, operations, allergies, injuries, and treatments)
- Current medications, supplements, and other substances the person may be using
- Family history (review the patient’s family and medical events, including hereditary conditions that place them at increased risk)
- Physical activities
- Social activities and engagement
- Alcohol, tobacco, and illegal drug use history
Learn information about Medicare’s substance use disorder (SUD) services coverage .
2. Review the patient’s potential depression risk factors
Depression risk factors include:
- Current or past experiences with depression
- Other mood disorders
Select from various standardized screening tools designed for this purpose and recognized by national professional medical organizations. APA’s Depression Assessment Instruments has more information.
3. Review the patient’s functional ability and safety level
Use direct patient observation, appropriate screening questions, or standardized questionnaires recognized by national professional medical organizations to review, at a minimum, the patient’s:
- Ability to perform activities of daily living (ADLs)
- Hearing impairment
- Home and community safety, including driving when appropriate
Medicare offers cognitive assessment and care plan services for patients who show signs of impairment.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), blood pressure, balance, and gait
- Visual acuity screen
- Other factors deemed appropriate based on medical and social history and current clinical standards
5. End-of-life planning, upon patient agreement
End-of-life planning is verbal or written information you (their physician or practitioner) can offer the patient about:
- Their ability to prepare an advance directive in case an injury or illness prevents them from making their own health care decisions
- If you agree to follow their advance directive
- This includes psychiatric advance directives
6. Review current opioid prescriptions
For a patient with a current opioid prescription:
- Review any potential opioid use disorder (OUD) risk factors
- Evaluate their pain severity and current treatment plan
- Provide information about non-opiod treatment options
- Refer to a specialist, as appropriate
The HHS Pain Management Best Practices Inter-Agency Task Force Report has more information. Medicare now covers monthly chronic pain management and treatment services .
7. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them to treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
8. Educate, counsel, and refer based on previous components
Based on the results of the review and evaluation services from the previous components, provide the patient with appropriate education, counseling, and referrals.
9. Educate, counsel, and refer for other preventive services
Include a brief written plan, like a checklist, for the patient to get:
- A once-in-a-lifetime screening electrocardiogram (ECG), as appropriate
- Appropriate screenings and other covered preventive services
Use these HCPCS codes to file IPPE and ECG screening claims:
Initial preventive physical examination; face-to-face visit, services limited to new beneficiary during the first 12 months of medicare enrollment
Electrocardiogram, routine ecg with 12 leads; performed as a screening for the initial preventive physical examination with interpretation and report
Electrocardiogram, routine ecg with 12 leads; tracing only, without interpretation and report, performed as a screening for the initial preventive physical examination
Electrocardiogram, routine ecg with 12 leads; interpretation and report only, performed as a screening for the initial preventive physical examination
Federally qualified health center (fqhc) visit, ippe or awv; a fqhc visit that includes an initial preventive physical examination (ippe) or annual wellness visit (awv) and includes a typical bundle of medicare-covered services that would be furnished per diem to a patient receiving an ippe or awv
* Section 60.2 of the Medicare Claims Processing Manual, Chapter 9 has more information on how to bill HCPCS code G0468.
Report a diagnosis code when submitting IPPE claims. We don’t require you to use a specific IPPE diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an IPPE when performed by a:
- Physician (doctor of medicine or osteopathy)
- Qualified non-physician practitioner (physician assistant, nurse practitioner, or certified clinical nurse specialist)
When you provide an IPPE and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
CPT only copyright 2022 American Medical Association. All rights reserved.
IPPE Resources
- 42 CFR 410.16
- Section 30.6.1.1 of the Medicare Claims Processing Manual, Chapter 12
- Section 80 of the Medicare Claims Processing Manual, Chapter 18
- U.S. Preventive Services Task Force Recommendations
No. The IPPE isn’t a routine physical that some patients may get periodically from their physician or other qualified non-physician practitioner (NPP). The IPPE is an introduction to Medicare and covered benefits, and it focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV during their IPPE. The Social Security Act explicitly prohibits Medicare coverage of routine physical exams.
No. The IPPE and AWV don’t include clinical lab tests, but you may make appropriate referrals for these tests as part of the IPPE or AWV.
No. We waive the coinsurance, copayment, and Part B deductible for the IPPE (HCPCS code G0402). Neither is waived for the screening electrocardiogram (ECG) (HCPCS codes G0403, G0404, or G0405).
A patient who hasn’t had an IPPE and whose Part B enrollment began in 2023 can get an IPPE in 2024 if it’s within 12 months of the patient’s Part B enrollment effective date.
We suggest providers check with their MAC for available options to verify patient eligibility. If you have questions, find your MAC’s website .
Annual Wellness Visit Health Risk Assessment
The annual wellness visit (AWV) includes a health risk assessment (HRA). View the HRA minimum elements summary below. A Framework for Patient-Centered Health Risk Assessments has more information, including a sample HRA.
Perform an HRA
- You or the patient can update the HRA before or during the AWV
- Consider the best way to communicate with underserved populations, people who speak different languages, people with varying health literacy, and people with disabilities
- Demographic data
- Health status self-assessment
- Psychosocial risks, including, but not limited to, depression, life satisfaction, stress, anger, loneliness or social isolation, pain, suicidality, and fatigue
- Behavioral risks, including, but not limited to, tobacco use, physical activity, nutrition and oral health, alcohol consumption, sexual health, motor vehicle safety (for example, seat belt use), and home safety
- Activities of daily living (ADLs), including dressing, feeding, toileting, and grooming; physical ambulation, including balance or fall risks and bathing; and instrumental ADLs (IADLs), including using the phone, housekeeping, laundry, transportation, shopping, managing medications, and handling finances
1. Establish the patient’s medical and family history
At a minimum, document:
- Medical events of the patient’s parents, siblings, and children, including hereditary conditions that place them at increased risk
- Use of, or exposure to, medications, supplements, and other substances the person may be using
2. Establish a current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including behavioral health care.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), and blood pressure
- Other routine measurements deemed appropriate based on medical and family history
4. Detect any cognitive impairments the patient may have
Check for cognitive impairment as part of the first AWV.
Assess cognitive function by direct observation or reported observations from the patient, family, friends, caregivers, and others. Consider using brief cognitive tests, health disparities, chronic conditions, and other factors that contribute to increased cognitive impairment risk. Alzheimer’s and Related Dementia Resources for Professionals has more information.
5. Review the patient’s potential depression risk factors
6. Review the patient’s functional ability and level of safety
- Ability to perform ADLs
7. Establish an appropriate patient written screening schedule
Base the written screening schedule on the:
- Checklist for the next 5–10 years
- United States Preventive Services Task Force and Advisory Committee on Immunization Practices (ACIP) recommendations
- Patient’s HRA, health status and screening history, and age-appropriate preventive services we cover
8. Establish the patient’s list of risk factors and conditions
- A recommendation for primary, secondary, or tertiary interventions or report whether they’re underway
- Mental health conditions, including depression, substance use disorders , suicidality, and cognitive impairments
- IPPE risk factors or identified conditions
- Treatment options and associated risks and benefits
9. Provide personalized patient health advice and appropriate referrals to health education or preventive counseling services or programs
Include referrals to educational and counseling services or programs aimed at:
- Fall prevention
- Physical activity
- Tobacco-use cessation
- Social engagement
- Weight loss
10. Provide advance care planning (ACP) services at the patient’s discretion
ACP is a discussion between you and the patient about:
- Preparing an advance directive in case an injury or illness prevents them from making their own health care decisions
- Future care decisions they might need or want to make
- How they can let others know about their care preferences
- Caregiver identification
- Advance directive elements, which may involve completing standard forms
Advance directive is a general term that refers to various documents, like a living will, instruction directive, health care proxy, psychiatric advance directive, or health care power of attorney. It’s a document that appoints an agent or records a person’s wishes about their medical treatment at a future time when the individual can’t communicate for themselves. The Advance Care Planning fact sheet has more information.
We don’t limit how many times the patient can revisit the ACP during the year, but cost sharing applies outside the AWV.
11. Review current opioid prescriptions
- Review any potential OUD risk factors
- Provide information about non-opioid treatment options
12. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them for treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
13. Social Determinants of Health (SDOH) Risk Assessment
Starting in 2024, Medicare includes an optional SDOH Risk Assessment as part of the AWV. This assessment must follow standardized, evidence-based practices and ensure communication aligns with the patient’s educational, developmental, and health literacy level, as well as being culturally and linguistically appropriate.
1. Review and update the HRA
2. Update the patient’s medical and family history
At a minimum, document updates to:
3. Update current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including those added because of the first AWV personalized prevention plan services (PPPS), and any behavioral health providers.
- Weight (or waist circumference, if appropriate) and blood pressure
5. Detect any cognitive impairments patients may have
Check for cognitive impairment as part of the subsequent AWV.
6. Update the patient’s written screening schedule
Base written screening schedule on the:
7. Update the patient’s list of risk factors and conditions
- Mental health conditions, including depression, substance use disorders , and cognitive impairments
- Risk factors or identified conditions
8. As necessary, provide and update patient PPPS, including personalized health advice and appropriate referrals to health education or preventive counseling services or programs
9. Provide advance care planning (ACP) services at the patient’s discretion
10. Review current opioid prescriptions
11. Screen for potential substance use disorders (SUDs)
12. Social Determinants of Health (SDOH) Risk Assessment
Preparing Eligible Patients for their AWV
Help eligible patients prepare for their AWV by encouraging them to bring this information to their appointment:
- Medical records, including immunization records
- Detailed family health history
- Full list of medications and supplements, including calcium and vitamins, and how often and how much of each they take
- Full list of current providers and suppliers involved in their care, including community-based providers (for example, personal care, adult day care, and home-delivered meals), and behavioral health specialists
Use these HCPCS codes to file AWV claims:
Annual wellness visit; includes a personalized prevention plan of service (pps), initial visit
Annual wellness visit, includes a personalized prevention plan of service (pps), subsequent visit
Report a diagnosis code when submitting AWV claims. We don’t require you to use a specific AWV diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an AWV if performed by a:
- Medical professional (including health educator, registered dietitian, nutrition professional, or other licensed practitioner) or a team of medical professionals directly supervised by a physician
When you provide an AWV and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
You can only bill G0438 or G0439 once in a 12-month period. G0438 is for the first AWV, and G0439 is for subsequent AWVs. Don’t bill G0438 or G0439 within 12 months of a previous G0402 (IPPE) billing for the same patient. We deny these claims with messages indicating the patient reached the benefit maximum for the time period.
Medicare telehealth includes HCPCS codes G0438 and G0439.
ACP is the face-to-face conversation between a physician (or other qualified health care professional) and a patient to discuss their health care wishes and medical treatment preferences if they become unable to communicate or make decisions about their care. At the patient’s discretion, you can provide the ACP during the AWV.
Use these CPT codes to file ACP claims as an optional AWV element:
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure)
Report a diagnosis code when submitting an ACP claim as an optional AWV element. We don’t require you to use a specific ACP diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
We waive both the Part B ACP coinsurance and deductible when it’s:
- Provided on the same day as the covered AWV
- Provided by the same provider as the covered AWV
- Billed with modifier 33 (Preventive Service)
- Billed on the same claim as the AWV
We waive the ACP deductible and coinsurance once per year when billed with the AWV. If we deny the AWV billed with ACP for exceeding the once-per-year limit, we’ll apply the ACP deductible and coinsurance .
We apply the deductible and coinsurance when you deliver the ACP outside the covered AWV. There are no limits on the number of times you can report ACP for a certain patient in a certain period. When billing this service multiple times, document changes in the patient’s health status or wishes about their end-of-life care.
SDOH is important in assessing patient histories; in assessing patient risk; and in guiding medical decision making, prevention, diagnosis, care, and treatment. In the CY 2024 Medicare Physician Fee Schedule final rule , we added a new SDOH Risk Assessment as an optional, additional element of the AWV. At both yours and the patient’s discretion, you may conduct the SDOH Risk Assessment during the AWV.
Use this HCPCS code to file SDOH Risk Assessment claims as an optional AWV element:
Administration of a standardized, evidence-based social determinants of health risk assessment tool, 5-15 minutes
Report a diagnosis code when submitting an SDOH Risk Assessment claim as an optional AWV element. We don’t require you to use a specific SDOH Risk Assessment diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
The implementation date for SDOH Risk Assessment claims is July 1, 2024. We waive both the Part B SDOH Risk Assessment coinsurance and deductible when it’s:
We waive the SDOH Risk Assessment deductible and coinsurance once per year when billed with the AWV.
If we deny the AWV billed with SDOH Risk Assessment for exceeding the once-per-year limit, we’ll apply the deductible and coinsurance. We also apply the deductible and coinsurance when you deliver the SDOH Risk Assessment outside the covered AWV.
AWV Resources
- 42 CFR 410.15
- Section 140 of the Medicare Claims Processing Manual, Chapter 18
No. The AWV isn’t a routine physical some patients may get periodically from their physician or other qualified NPP. We don’t cover routine physical exams.
No. We waive the coinsurance, copayment, and Part B deductible for the AWV.
We cover an AWV for all patients who’ve had Medicare coverage for longer than 12 months after their first Part B eligibility date and who didn’t have an IPPE or AWV within those past 12 months. We cover only 1 IPPE per patient per lifetime and 1 additional AWV every 12 months after the date of the patient’s last AWV (or IPPE). Check eligibility to find when a patient is eligible for their next preventive service.
Generally, you may provide other medically necessary services on the same date as an AWV. The deductible and coinsurance or copayment applies for these other medically necessary and reasonable services.
You have different options for accessing AWV eligibility information depending on where you practice. Check eligibility to find when a patient is eligible for their next preventive service. Find your MAC’s website if you have specific patient eligibility questions.
Know the Differences
An IPPE is a review of a patient’s medical and social health history and includes education about other preventive services .
- We cover 1 IPPE per lifetime for patients within the first 12 months after their Part B benefits eligibility date
- We pay IPPE costs if the provider accepts assignment
An AWV is a review of a patient’s personalized prevention plan of services and includes a health risk assessment.
- We cover an annual AWV for patients who aren’t within the first 12 months after their Part B benefits eligibility date
- We cover an annual AWV 12 months after the last AWV’s (or IPPE’s) date of service
- We pay AWV costs if the provider accepts assignment
A routine physical is an exam performed without relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury.
- We don’t cover routine physical exams, but the IPPE, AWV, or other Medicare benefits cover some routine physical elements
- Patients pay 100% out of pocket
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure .
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Health & Human Services (HHS).
CPT codes, descriptions and other data only are copyright 2022 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.

- CCM (Chronic Care Managmenet)
- Care Coordination
- Preventitive and Wellness Programs
- Product Updates
- RHCs / FQHCs
« View All Posts
Annual Wellness Visit | CPT codes
2023 Annual Wellness Visit CPT Codes: G0402, G0438, G0439
- Share This Article
January 25th, 2023 | 8 min. read

ThoroughCare
Content Team
Print/Save as PDF
Understanding the billing codes for Medicare Annual Wellness Visits (AWVs) can provide a better idea of what is expected, both by the patient and by the payer. Understanding billing codes may also help you project revenues and optimize your staff’s capacity .
At ThoroughCare , we’ve worked with clinics and physician practices nationwide to help them streamline and capture Medicare reimbursements. Our software solution assists with the rules and regulations for AWVs while also tracking all activities related to providing the program and easing the difficulties of billing.
What are Annual Wellness Visits?
Annual Wellness Visits are free for anyone covered by Medicare Part B and include a yearly assessment of a patient’s health and overall well-being. They are designed not as a yearly physical examination, but as a critical care marker that bridges gaps in the yearly physical exam while developing and updating a patient’s personalized plan of care.
That personalized care plan is designed to help prevent disease and disability and is based on the patient’s current health and determined risk factors. The overall goal is to establish a record of the patient’s physical and mental well-being for the purpose of preventive health planning .
AWVs Include:
- A health risk assessment (HRA)
- A review and update of medical and family history
- A review of current providers, prescriptions/medications, and durable medical equipment suppliers
- Height, weight, blood pressure, BMI, and other routine measurements
- Personalized health advice, health education, and preventative counseling
- A list of identified risk factors, current medical and mental health conditions, and recommended treatment options
- A cognitive impairment screening
- A five to 10-year screening schedule for appropriate preventive services
- A review of the patient’s functional ability and level of safety, including screening for hearing impairments, risk of falling, activities of daily living, and level of home safety
- Identification of patients at risk for alcohol, tobacco, and opioid abuse
- Advance care planning
There are three types of wellness visits : Initial Preventive Physical Examination (IPPE), an Initial Annual Wellness Visit, and the Subsequent Annual Wellness Visit. Each entails a different billing code as well as specific qualifiers for each program.
- Initial Preventive Physical Examination: Patients may only receive this benefit within the first 12 months of their Medicare enrollment . Commonly referred to as the “welcome to Medicare visit,” it is considered a once in a lifetime assessment and after the initial eligibility period, the patient cannot receive an IPPE. It is also dependent on the HRA .
- Initial Annual Wellness Visits : Similar to an IPPE, except it is available to a patient after 11 months of Medicare enrollment . This is for patients that miss their window for an IPPE. However, if the patient does complete an IPPE, they must still complete the Initial Annual Wellness Visit. This screening also includes an optional cognitive exam and end-of-life planning.
- Subsequent Annual Wellness Visit: Is the yearly follow-up to an Initial Annual Wellness Visit . Eleven full months after the Initial Annual Wellness Visit, a patient can attend these visits to modify and maintain their preventive care plan, based on how their health is at any given time.
As the patient’s health evolves over time, a doctor may use the Subsequent Annual Wellness Visit to guide them toward other Medicare preventive programs, such as Chronic Care Management (CCM) , Behavioral Health Integration (BHI) , or Remote Patient Monitoring (RPM) .

Billing Medicare Annual Wellness Visits
Five items are required when submitting a claim through Centers for Medicare & Medicaid Services (CMS) :
- A CPT Code for the specific type of AWV provided
- An ICD-10 code for a general adult medical examination (Z00.00)
- Date of service
- Place of service (most office in-office or telehealth)
- Submit National Provider Identifier (NPI) number
It is helpful to know the care manager assigned to a patient in case of an audit.
Three Steps to Bill for AWVs :
- Verify CMS requirements were met
- Submit claims to CMS annually
- Determine there are no conflicting billing codes
CPT Codes for Annual Wellness Visits
See 2024 reimbursement rates here .
The types of AWVs are reflected in the CPT codes. The crucial qualifying determinant is when a certain AWV can be provided and billed.
.png?width=953&height=419&name=awv_2023_cpt_codes_downloadable_cta%20(3).png)
AWVs for Federally Qualified Health Centers (FQHC) and Advance Care Planning (ACP)
As shown in the chart above, FQHC are able to bill for AWVs, although they utilize additional codes.
In addition to the standard CPT codes associated with AWVs, FQHC may use a special add-on code (G0468) that will allow them to receive additional reimbursement. For example, if an FQHC were to provide an IPPE, the clinic would bill for G0402 + G0468 for a total average reimbursement of $322. This coding indicates to CMS that the service is being provided through an FQHC. The good news is that these organizations receive much higher average reimbursement rates
Advance care planning (ACP) is not a type of AWV , but it can play a meaningful part in the program.
ACP is a formal process to understand the patient’s preferences for potential and future medical care, such as end-of-life planning, a living will, and power of attorney. It is an opportunity to craft a patient-centered care plan and an AWV drives just that opportunity. Providers often complete an ACP during an AWV.
ACP is fully covered for patients under Medicare Part B if it is conducted during the AWV. It is a free service that is an optional element of AWVs. Favorably, it is reimbursable for your practice and can be billed in concurrence with an AWV using CPT code 99497 for the first 30 minutes and 99498 for subsequent 30-minute billing.
Streamline Medicare Annual Wellness Visits
ThoroughCare offers end-to-end workflow for Annual Wellness Visits.
We simplify the process and help providers engage patients to get their most relevant health information. Guided interviews help ask the right questions and ensure all service requirements are met. ThoroughCare includes digital solutions, such as:
- An interactive health risk assessment
- Screening tools, such as ADL, CAGE, DAST-10, GAD-7, MDQ, PAC, PHQ-2, and a mini cognitive exam
- A care gaps summary with recommended interventions
- A full report of Personalized Prevention Plan Services
- Comprehensive care planning tools
- Automated CPT code assignment for accurate billing

Reimbursement rates are based on a national average and may vary depending on your location. Check the Physician Fee Schedule for the latest information.
Get the newsletter
Insights for those starting, managing, and growing independent healthcare practices
Get expert tips, guides, and valuable insights for your medical practice

April 8, 2024
Getting Paid
Medical Billing & Coding
2024 getting paid strategies for independent practices and billing companies
The key to preventing billing errors and claim denials is preparation.

Most Popular
At a glance.
- New regulations and payer challenges, such as tighter Medicaid controls and scrutiny of E&M codes, have emerged post-COVID-19 pandemic, complicating medical billing.
- Reducing claim denials relies on clear initial paperwork, precise coding, and proactive patient insurance verification.
- For 2024, success hinges on assembling skilled teams, offering targeted training, and employing digital tools to enhance billing efficiency and revenue.
Getting paid enables practices and billing companies to grow faster — but capturing payments hasn’t been easy since the start of the COVID-19 pandemic. However, there are several ways to improve the billing process and drive revenue.
In our recent webinar , Aimee Heckman, a healthcare business consultant with over 35 years of experience in medical practice management, offers insights into the medical billing industry and strategies to optimize payments in 2024.
We’ve summarized the highlights below.
State of the healthcare industry
Learn about crucial 2024 updates to the industry, and regulatory and payer challenges to be aware of.
New regulatory challenges
The public health emergency technically ended in May 2023 but continues to affect the healthcare industry, particularly when dealing with billing. Key regulatory challenges and changes include:
- Tighter Medicaid controls . The COVID-19 pandemic led many organizations to relax requirements and normal controls, leading to this overpayment. However, we are already seeing a return to tighter controls to reduce overpayments.
- More Health Insurance Portability and Accountability Act ( HIPAA) data breaches . In 2022 and 2023, millions of patients suffered from data breaches. Unfortunately, social media and news outlets were often involved in these breaches.
- Medicare’s 2024 final fee schedule . This expanded options for medicare patients to access mental health professionals. Primary care providers can also leverage a new add-on code, G2211 , for compensation related to patients with complex and multiple comorbidities.
- Restriction of medical debt information . The Consumer Financial Protection Bureau (CFPB) is an independent government agency that protects the American consumer from unfair business practices. In 2022, it proposed excluding medical debt to calculate vantage scores, making it difficult to collect from patients.

Payer challenges
Payers also face significant hurdles when it comes to making payments:
- Evaluation and management (E&M) code denials. Patients attending procedures without a separately identified NM service for a condition not related to a procedure face almost automatic denials.
- Stringent ICD-10 coding requirements . Including diagnosing codes irrelevant to a patient visit leads to additional claim denials.
- Increasing smart edits . Smart edits is a claim optimization tool meant to reduce rejections. However, it can confuse practice management systems and cause errors.
The “end” of the public health emergency
The end of the COVID-19 public health emergency has driven many of the regulatory changes over the past 2 years. Verified telehealth benefits have reduced the use of patient cost-sharing. Despite its flexibility for providers and patients, there have been adjustments to cross-state treatments that may affect billing.
Overcoming payer roadblocks
Medical billers and practices now face additional challenges in ensuring claim acceptances. These rejections stem from several sources. But there are ways to reduce the likelihood of rejection and streamline your claims process.
Reducing rejections and denials starts at the front desk
Many rejections stem from unclear or confusing paperwork.
For example, filing claims covered by more than one health plan, known as coordinating benefits, can result in rejected claims and delayed payment due to overlapping policies and confusion over which plan pays first. Asking patients to contact their insurance to discuss a denial during their next appointment can reduce confusion and speed up the process.
“ Simple data entry errors are the major cause of rejections. ”
Furthermore, ensuring patients regularly update their payer forms at their PCP can streamline the billing process while decreasing paperwork hiccups.
“Simple data entry errors are the major cause of rejections,” says Aimee. “It’s important that your staff are the first point of contact. You can also use digital forms offerings to allow patients to enter their own information.”
65% of rejected claims will never be resubmitted , and it's harder and more costly to resubmit than it is to get it right the first time. So, follow the steps to ensure that claims are good from the start.
Payer proofing your coding
Many E&M codes and code modifiers have come under increased scrutiny for potential misuse, including modifier 25, which represents a significant and separate E&M service by the same physician on the same day of a procedure or appointment. Ensuring that the use of modifier 25 matches guidelines and maintaining code documentation can increase the likelihood of claim acceptance. Only include codes on the claim that relates to the patient’s visit.
“If it wasn't addressed during the visit, and it's not documented, don't include the code on your claim,” says Aimee.
Documenting visits to beat automatic denials
Avoid notes that look like copy-and-paste descriptions from earlier notes, also called carry forward notes, to reduce automatic claim denials. Furthermore, ensure the documentation includes specific information from the most recent visit and that the codes match the conditions addressed.
“If you do use carry forward, clear out anything that wasn’t addressed during the visit,” says Aimee. “More importantly, ensure you add information on what was addressed.”
Further Reading
Preparing for a strong 2024: lessons from successful practices and billing companies.
In 2024, there are many strategies that billing companies and medical practices can use to improve their billing process and get paid on time.
Build a successful team
Finding the right people is only step one in developing a successful team. Proper onboarding, perks, and policy documentation improve staff retention and empower your staff .
Providing resources, training, and strategic recommendations
Often, medical billers have to spend valuable time correcting avoidable errors when practices aren’t doing their part. In a recent Tebra survey :
- 57% of medical billing companies said practices fail to verify insurance is up to date and eligible
- 37% of medical billing companies said practices submit inaccurate patient information
- 37% of medical billing companies said practices don't get prior authorizations
In addition, 52% of billing companies are prioritizing training their own staff over training their practices, despite the fact that the most common frustrations and roadblocks are coming from mistakes on the practice side. Frustrations like the ones above can drain time and internal resources, so practices and billing companies need to invest in proper training for both internal and client staff.
Capture every dollar you can
Accurate coding and charge capture not only keep pace with regulations but also reduce the likelihood of rejections, improve cash flow, and boost revenue.
Don’t let dollars walk out the door
There are many easy-to-implement ways practices can provide value while capturing more revenue.
Streamlining check-in with digital patient tools, such as an online booking calendar or portal, removes pressure from the front desk and patients while reducing no-shows. Digital intake forms reduce data entry errors and help you collect better co-pays. Additional payment or statement options make it even easier to collect.
Year-end housekeeping
The key to preventing billing errors and claim denials is preparation. Medical billers and practice management can drive growth while staying compliant by:
- Conducting HIPAA risk assessments
- Applying for MIPS/QPP exceptions
- Reviewing the cost-sharing reset and benefits verification
- Refreshing eligibility verification policies
Get all the details
Want more than the highlights? Check out our full webinar with Aimee Heckmann and learn how to optimize your billing in 2024 .

You Might Also Be Interested In
Optimize your independent practice for growth. Get actionable strategies to create a superior patient experience, retain patients, and support your staff while growing your medical practice sustainably and profitably.
Subscribe to The Intake: A weekly check-up for your independent practice
Kelsey Ray Banerjee
Kelsey Ray Banerjee is a professional content writer in the healthcare, marketing, and finance space. She has worked in the back office of a psychiatric practice, and with family members working in mental health for 2 generations, she understands the challenges healthcare professionals face when it comes to marketing and admin. She believes access to efficient healthcare is essential for society’s well-being, and loves being able to write content that can positively impact a practice and its patients.
Suggested for you

Coding rules for modifier 33 and modifier PT

Sample letter for appealing a health insurance claim denial

Understanding E&M codes and getting the latest updates

How to outsource medical billing to master revenue management
Get expert tips, guides, and valuable insights for your healthcare practice, subscribe to the intake.
A weekly check-up for your independent practice — right in your inbox

FinanceBuzz
Understanding These Health Insurance Codes Could Help You Spot Errors and Avoid Overpaying
Posted: May 30, 2023 | Last updated: July 29, 2023

Many people worry that despite health insurance coverage, they might get stuck paying an expensive bill after a visit to the doctor.
Even if you call the doctor’s office and make sure your insurance will cover the provider, it's still possible to end up paying some of the cost.
In some cases, the amount you owe is small. But billing errors can lead to a costly situation. And such errors are more common than you might think.
Understanding the most common insurance codes and how they work can help you avoid wasting money by paying hundreds more than you actually should.
6 clever ways to crush your debt
What are insurance codes?
When you visit a medical professional, they will bill your insurance provider with a specific code related to your appointment. The code describes what happened during the visit. Each visit may have multiple codes, especially if you had lab tests, imaging, or similar services.
Insurance companies use these codes to decide how much of the service they will cover before the rest of the bill is passed on to you. Unfortunately, it's not uncommon for errors to creep into this process.
The American Medical Association (AMA) says error rates at insurance companies can reach nearly 20%. Unless you notice and dispute such errors, you could end up on the hook for a larger percentage of the bill than you expected.
Next are a few key types of health insurance coding systems you need to know.
Get expert advice on making more money - sent straight to your inbox.

Current Procedural Terminology
Current Procedural Terminology (CPT) is the official name of the coding system used by health care billing departments.
There are three main levels of CPT codes: Category I, Category II, and Category III. Category I represents the most common code and is likely the one you will see.
The Category I codes fall into six basic categories:
- Evaluation & Management (99201–99499)
- Anesthesia (00100–01999; 99100-99140)
- Surgery (10021–69990)
- Radiology Procedures (70010–79999)
- Pathology and Laboratory Procedures (80047–89398)
- Medicine Services and Procedures (90281–99199; 99607)
Here are some common CPT codes:
- 99213 and 99214: Established patient office visit
- 99201-05: New patient office visit
- 80053: Organ or disease-oriented panels
- 93010: Cardiography procedures
- 71045: Diagnostic radiology (diagnostic imaging) procedures of the chest

Healthcare Common Procedure Coding System
If you have Medicare, your codes will be based on another coding system: The Healthcare Common Procedure Coding System.
There are two subtypes: Level I and Level II:
- Level I refers to codes similar to those of the CPT system.
- Level II refers to codes unique to Medicare itself and used for services, products, and supplies that don't fall under CPT codes. You can download a list at the Centers for Medicare & Medicaid Services website if you need to check one of these codes.
7 Things to Do If You’re Barely Scraping by Financially
International Classification of Diseases
The International Classification of Diseases is a coding system describing your illness or diagnosis. The appropriate CPT code is then linked to this disease code.
The World Health Organization (WHO) helped create these codes, which are used globally.
Here are some common disease codes:
- U07.1: COVID-19
- G89.11: Acute pain due to trauma
- I10: Essential (primary) hypertension
- J301: Allergic rhinitis due to pollen

How to prevent errors
Billing errors can happen if the health care provider submits the wrong code. The insurance company might refuse to pay for a treatment when this happens.
For example, let’s say you have pain and swelling in your ankle and the doctor orders an X-ray. If the medical provider’s billing department codes your illness as the flu, the insurance company might deny paying for your X-ray because it’s unrelated to flu treatment.
While it's impossible to eliminate the risk of such errors, you can greatly reduce their impact by taking some key steps.
For example, when you visit the doctor's office, write down what happens. If there's a physical exam along with bloodwork, make a note of both the exam and the bloodwork. Some doctors also have an online system that lets you see their notes, which should include what occurred during the visit.
After receiving a medical bill, go through it and see if anything is listed as not covered. You may have to ask your provider for a copy of the superbill, which is a document created specifically for insurance companies.
The superbill should have all of the billing codes used during the visit. Match the codes with your notes from the actual visit.

How to fight back against insurance error codes
Contact the billing department to explain the discrepancy if you notice an error. Then, ask them to review and refile the claim with insurance.
Set a reminder to follow up in a couple of weeks to ensure that the mistake has been fixed. It can take several weeks for the issue to be resolved.
Unfortunately, medical billing departments can be notorious for giving patients the runaround, so you may have to be persistent and call back a few times. Visiting them in person can expedite the process if no one calls you back.
You can also ask for a patient advocate or ombudsperson to act as a liaison between you and the billing department. However, only some hospitals will have one of these.
If the billing department is too far away to visit, contact the physician via email or social media.
You can also contact your insurance company and ask for a three-way call between yourself, the billing department, and the insurance company. Sometimes, this will be more effective than just calling the billing department yourself.
5 Signs You’re Doing Better Financially Than the Average American

Bottom line
Medical billing errors happen more often than many people think. These mistakes can be costly for patients.
So, to eliminate some financial stress , keep a close eye on what happens during your appointment and scan your bill closely when it arrives. Doing so might save you a lot of cash.
More from FinanceBuzz:
- 6 genius hacks Costco shoppers should know
- 9 things you must do before the next recession.
- Can you retire early? Take this quiz and find out.
- 9 simple ways to make up to an extra $200/day
We may receive compensation from the products and services mentioned in this story, but the opinions are the author's own. Compensation may impact where offers appear. We have not included all available products or offers. Learn more about how we make money and our editorial policies .
More for You
30 trans celebrities who broke barriers
Kentucky GOP lawmakers remove Democratic governor's role in filling US Senate vacancies
Kansas City Chiefs receiver Rashee Rice surrenders to police in connection with 6-car crash in Dallas
These Are 10 Smells That Cats Absolutely Hate
25 movies that will really mess with your head
Putting money in bank accounts is 'the worst thing you can do' for taxes, says former Intuit CEO
Gender identity law passes in German parliament
A major Burger King franchisee in California says he can't roll out order kiosks fast enough due to the state's new $20 fast-food minimum wage
Surveillance footage captured dozens of missile interception over Israel-Lebanon border
17 Signs That Someone Is Genuinely a Good Person
27 Side Characters That Stole The Spotlight
Worried about microplastics in your water? You can get rid of them with common kitchen items
Decades-old military object washes up on Massachusetts beach
KFC Is Changing Its Menu—Here’s What to Expect
Meet the 55 newest dog breeds to get recognized by the American Kennel Club
Israel attacks Hezbollah targets in Lebanon
I moved from California to Tennessee for my husband's job. We can finally save money, but it's been a major culture shock.
Immortal TV Characters: The 25 Most Legendary Figures
The Dumbest Things You Can Do With Your Money
Masters neighbor refuses to sell home despite millions in offers from Augusta golf club
Is This Really Medically Necessary? CodeCast | Medical Billing and Coding Insights
TPE audits from Medicare, along with private and commercial payer audits are on the rise. It is more important than ever to monitor physician records and make sure that when they submit any level of E/M. (Especially level 4’s and level 5’s.) In this episode, Terry reinforces making sure the visit not only meets the level of service billed, but also that the visit is even medically necessary to be able to be billed. Subscribe and Listen You can subscribe to our podcasts via: * Apple Podcasts – https://podcasts.apple.com/us/podcast/codecast-medical-billing-coding-insights/id1305926627 * Spotify – https://open.spotify.com/show/1lA69Q7EnjSMuVr3sXVWlX * TuneIn – https://tunein.com/radio/CodeCast–Medical-Billing-p1056702/ * YouTube – https://www.youtube.com/channel/UCoNm5vs6PFMIEDa5Undidlg * YouTube Music – https://www.youtube.com/playlist?list=PLQ8tk23yZroZslhtTVe-PEIjQsAoJZJIQ * Pandora – https://www.pandora.com/podcast/codecast-medical-billing-and-coding-insights/PC:1000156874 * Amazon Podcasts – https://music.amazon.com/podcasts/c9d8dc99-fced-45a2-82b4-0efdf144c897/CodeCast-Medical-Billing-and-Coding-Insights * iHeart Radio – https://www.iheart.com/podcast/256-codecast-medical-billing-a-31135434/ If you’d like to become a sponsor of the CodeCast podcast please contact us directly for pricing: https://www.terryfletcher.net/contact/
- Episode Website
- More Episodes
- Terry Fletcher Consulting, Inc.
Top Podcasts In Business
What exactly is a billing ZIP code, and why do credit cards need it?
Billing ZIP codes are a crucial aspect of credit card security, helping to prevent fraud and ensure authorized transactions.

Laura Gariepy
Laura started writing about personal finance in 2018 when she took a sabbatical from her career in human resources and launched a blog discussing her journey. Realizing she could earn a more lucrative and flexible living as a freelancer, she went all-in. Along with writing, she has coached other professionals on how to launch their own freelance businesses.

Hanna Horvath
Hanna Horvath is a CERTIFIED FINANCIAL PLANNER™ and Bankrate's senior editor of content partnerships.
Updated April 11, 2024, 6:39 PM EDT

Fox Money is a personal finance hub featuring content generated by Credible Operations, Inc. (Credible), which is majority-owned indirectly by Fox Corporation. The Fox Money content is created and reviewed independent of Fox News Media. Credible is solely responsible for this content and the services it provides.
Advertiser disclosure: Content provided by Bankrate.com. Fox and its content partners earn compensation from the affiliate companies below. This content doesn’t include all available offers, and compensation may impact how and where links appear in the content.
You may be asked for your billing ZIP code when making online purchases or providing credit card information over the phone. But what exactly is a billing ZIP code, and why is it important?
A billing ZIP code, also known as a postal code, is a five-digit number the United States Postal Service (USPS) assigns to every address in the country. This code helps card companies verify the cardholder's identity and prevent fraudulent transactions.
Understanding how billing ZIP codes work allows you to make credit card payments smoother.
What exactly is a billing ZIP code?
The USPS created the Zoning Improvement Plan (ZIP) code system in the 1960s. ZIP codes had five digits – one to designate a broad geographic region of the country, two to narrow the location to a regional area, and two to identify a specific post office.
Your billing ZIP code, sometimes called your credit card ZIP code, is “associated with the address where you receive your bill. Or, if you receive e-statements, with the address you've listed on your account. Generally, this is your home address,” says Louis DeNicola, a personal finance writer who specializes in credit cards and fraud.
What is the purpose of a billing ZIP code?
Credit card companies use your billing ZIP Code for multiple purposes. It’s an essential tool for preventing and detecting credit card fraud.
Fraud prevention
A merchant may ask you to enter your billing ZIP code when you use your card in person or shop online. Your card issuer may ask you for it when verifying your account.
When you provide your ZIP code during a transaction, the card issuer compares it to the address they have on file. If the ZIP codes match, it's a good sign that the person making the purchase is the legitimate cardholder, says Beverly Harzog, consumer credit expert and author of The Debt Escape Plan.
For example, let's say a thief steals your credit card and tries to make an online purchase. The transaction may be declined if they don't know your billing ZIP code. The credit card company will see a mismatch between the provided ZIP code and the one associated with your account.
This security measure helps consumers keep their card information from falling into the wrong hands. Roughly 70% of card fraud is considered card-not-present fraud , which occurs online or over the phone.
Card companies can reduce the risk of unauthorized transactions by requiring billing ZIP codes.
Address verification
Billing ZIP codes are part of a larger security measure called the Address Verification System (AVS). AVS is a tool card processors use to confirm that the person making a transaction is the cardholder. AVS also checks the billing address provided against the address on file with the card issuer.
When a merchant runs a card transaction, they submit the cardholder's billing address and ZIP code to the card processor. The processor then sends this information to the issuer, who compares it to their records. The issuer will send a response code indicating whether the address and ZIP code match.
AVS is particularly useful for online and phone transactions where the cardholder is not physically present to verify their identity. By cross-referencing the provided information with the issuer's records, AVS adds an extra layer of security to these card-not-present transactions.
It's important to note that while AVS is a valuable tool for preventing fraud, it's not foolproof. Sometimes, a transaction may still be approved even if the address or ZIP code doesn't match.
This can happen if the issuer accepts the transaction based on other factors, such as the cardholder's history with the company or the purchase amount.
When you’ll need your billing ZIP code
When you apply for a new credit card, you must share your billing ZIP Code. If you’re unsure about your ZIP code, you can look it up on the USPS website . Here are a few instances when your billing ZIP code may be required.
Online and phone transactions
Billing ZIP codes are most often required for online transactions. When you're shopping online and enter your card information, you'll usually be asked to provide your billing ZIP code.
“Your purchase might be declined if the two billing ZIP codes don't match, or you might be asked for additional information, such as the card's CVV number. Or, if your card was stored in your online account, you might be asked to reenter the entire card number again,” says DeNicola.
This requirement helps online merchants protect themselves from chargebacks and fraudulent transactions. If a thief tries to use a stolen card to make an online purchase, they may not have access to the cardholder's billing ZIP code.
Gas stations
Some gas stations have customers enter their billing ZIP code when paying with a credit card at the pump. This practice helps prevent unauthorized use of stolen or lost credit cards, as thieves are less likely to know the cardholder's ZIP code.
When you insert your credit card at the pump, the gas station's payment system will prompt you to enter your billing ZIP code. The transaction will be approved if the code you enter matches the one on file with your card issuer.
This security measure is particularly important for gas stations, as they often face higher rates of credit card fraud.
In-store purchases
While less common than online or phone transactions, some in-store purchases may require a billing ZIP code. This often happens when you make a big-ticket purchase or when the store's payment system is set up to request a ZIP code for added security.
For example, suppose you're buying a high-end electronic device or expensive jewelry. The store may ask for your billing ZIP code to verify your identity and ensure you're the authorized cardholder.
What if I don’t know my billing ZIP code?
If you're unsure of your billing ZIP code, there are a few ways to find it:
- Check your credit card statement. Your billing ZIP code should be listed alongside your billing address on your monthly statement.
- Log into your online credit card account. Your account profile should include your billing address and ZIP code.
- Contact your credit card issuer. Call your credit card issuer's customer service line for assistance if you can't find your ZIP code on your statement or online account.
Keeping your billing ZIP Code updated with your credit card issuers is critical. Todd Christensen, financial counselor and education manager at MoneyFit, shared a first-hand cautionary tale about what happens when you don’t.
“My wife and I have moved our family across the country twice in the past three years, and we quickly discovered the importance of keeping our ZIP updated with our credit card companies,” he says. “Soon after arriving in our new home, I accidentally locked my credit card by entering our new home's ZIP code before I updated our address with our credit card company.”
What happens if you use the wrong billing ZIP code?
If you enter an incorrect billing ZIP code during a transaction, the consequences vary depending on the merchant and the card issuer.
Often, the transaction will be declined. You may also need to re-enter the correct ZIP code or provide an alternative payment method. The merchant may accept the transaction despite the ZIP code mismatch, particularly if you've made successful purchases with them.
If you have repeated issues with your billing ZIP code or suspect your card information has been compromised, contact your card issuer immediately. They can help you update your information, issue a new card, and investigate any suspicious activity on your account.
“When merchants and credit card companies ask for your ZIP Code at the point of purchase, it's a way of telling the cardholder, ‘You keep your information updated with us, and we'll keep potential thieves out of your account,’” says Christensen.
How to update your billing ZIP code
If you need to update your billing ZIP Code, you can do so in a few different ways:
- Log in to your online account and edit your contact details.
- Call the customer service department and tell the representative your new address. (You can find the phone number online, on the back of your card, or your billing statement.)
- Provide the correct information on the back of the payment slip enclosed with your billing statement (if you are still paying your bills by mail).
- Go to a bank branch (if applicable) and ask the representative to process the change.
Billing ZIP code vs. shipping ZIP code
A billing ZIP code is connected to the address where your credit card statements are mailed. Your shipping ZIP code determines the destination of something you've purchased.
Your billing and shipping ZIP Codes will usually be the same. But there are situations where they may differ — like if you're sending a gift to someone else or when you've recently moved and haven't updated your billing address yet.
When making an online purchase, enter the appropriate ZIP code in the designated field. If you're asked for a billing ZIP code, provide the one associated with your credit card statement address. If you're asked for a shipping ZIP code, enter the one for the destination where you want the item to be delivered.
Bottom line
Billing ZIP codes play a crucial role in credit card security. They help prevent fraud and ensure that authorized cardholders make transactions. Remember, if you're ever unsure about your billing ZIP code, you can find it on your credit card statement, online account, or by contacting your card issuer.
Editorial disclosure: Opinions expressed are author's alone, not those of any bank, credit card issuer, or other entity. This content has not been reviewed, approved, or otherwise endorsed by any of the entities included in the post.


IMAGES
VIDEO
COMMENTS
Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to ...
The E/M visit CPT® codes 99202-99215 (new and established patients) were revised to decrease documentation and coding administrative burden and to ensure that E/M payment is resource-based. The revisions remov e the history and physical examination as key components in choosing the appropriate E/M level of a visit. Now, code level selection for
The CPT codes for office visits can be found in the CPT manual; under range CPT 99202 until 99205 for office visits of new patients. For office visits of established patients, you can use range 99211 to CPT code 99215. We also included CPT 99070 in case you need to bill extra supplies/materials for office visits and CPT code 99072 if extra ...
Download PDFs of the issue brief and other resources—the AMA's telehealth quick guide outlines policy, CPT coding and payment considerations to keep in mind during COVID-19. ... An in-person visit will not be required for a patient to be eligible for behavioral health services via telehealth through December 31, 2024.
at the visit • This includes the possible management options selected and those considered, but not selected, after shared medical decision making. • CPT examples: • A psychiatric patient with a sufficient degree of support in the outpatient setting • The decision to not hospitalize a patient with advanced dementia with an acute ...
Here's a brief explanation of how you select a billing code level for an "evaluation and management" or "Office Visit" after January 1st, 2021. These guidelines apply to common visit billing codes, such as 99212, 99213, 99214, or 99215, as well as to the selection of codes 99202 through 99205. Select a Code Based on Medical Decision ...
Do not report when billing remote monitoring, CCM, TCM, care plan oversight, and codes for supervision of patient in home, domiciliary or rest home etc. for the same communication[s]). Do not report for home and outpatient INR monitoring when reporting 93792, 93793. No modifier needed as these are technology based codes.
CPT® code 99203: New patient office or other outpatient visit, 30-44 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
Code categories. Telephone codes are required for audio-only appointments, while office codes are for audio and video visits. Time of visit. A common mistake made by health care providers is billing time a patient spent with clinical staff. Providers should only bill for the time that they spent with the patient. Store-and-forward
Best Guide to E-Visit Documentation, Coding, and Billing. The American Academy of Family Physicians (AAFP) encourages safe, secure online interactions between physicians and patients, such as electronic visits or "virtual e-visits.". In non-emergency situations, e-visits can substitute for office visits with primary care providers.
Page 1 of 6. MLN901705 February 2024. We pay for specific Medicare Part B services that a physician or practitioner provides via 2-way, interactive technology (or telehealth). Telehealth substitutes for an in-person visit, and generally involves 2-way, interactive technology that permits communication between the practitioner and patient.
Append this modifier to an appropriate CPT code (listed in Table 4 in this fact sheet or refer to the 2023 CPT manual) for an audio-only real-time interaction between a physician or other qualified healthcare ... Subsequent nursing facility care services (limit 1 telemedicine visit every 30 days) 99307- 99310 Transitional care management ...
We maintain and annually update a List of Current Procedural Terminology (CPT)/Healthcare Common Procedure Coding System (HCPCS) Codes (the Code List), which identifies all the items and services included within certain designated health services (DHS) categories or that may qualify for certain exceptions. We update the Code List to conform to the most recent publications of CPT and HCPCS ...
Although, "there are some notable differences in this area when it pertains to CPT® versus CMS," Jimenez forewarned. "One of the biggest changes, I think, in the 2023 changes was the elimination of observation codes," Jimenez said. Effective Jan. 1, 2023, hospital observation codes 99217-99220 and 99224-99226 are deleted.
Coding Guidelines. Home/domiciliary services provided for the same diagnosis, same condition or same episode of care as services provided by other practitioners, regardless of the site of service, may constitute concurrent or duplicative care. When such visits are provided, the record must clearly document the medical necessity of such services.
Federally qualified health center (fqhc) visit, ippe or awv; a fqhc visit that includes an initial preventive physical examination (ippe) or annual wellness visit (awv) and includes a typical bundle of medicare-covered services that would be furnished per diem to a patient receiving an ippe or awv ... Coding. Use these CPT codes to file ACP ...
At the same time, coding compliance has become all the more critical due to greater scrutiny by payers. In 2019, CMS and the HHS Office of Inspector General handed out fines and penalties related to coding noncompliance of $2.5 billion and $3.7 billion, respectively. Issues with billing modifiers are a top reason for noncompliance.
Reimbursement rates are based on a national average and may vary depending on your location. Check the Physician Fee Schedule for the latest information. Learn 2023 CPT billing codes for annual wellness visits (AWVs) and understand requirements to maximize the value of G0402, G0438, G0439, 99497, and G0468.
Evaluation and management (E&M) code denials. Patients attending procedures without a separately identified NM service for a condition not related to a procedure face almost automatic denials. Stringent ICD-10 coding requirements. Including diagnosing codes irrelevant to a patient visit leads to additional claim denials. Increasing smart edits ...
Current Procedural Terminology (CPT) is the official name of the coding system used by health care billing departments. There are three main levels of CPT codes: Category I, Category II, and ...
TPE audits from Medicare, along with private and commercial payer audits are on the rise. It is more important than ever to monitor physician records and make sure that when they submit any level of E/M. (Especially level 4's and level 5's.) In this episode, Terry reinforces making sure the visit n…
Question: For all lab tests performed in the office, our nurse researches the history, collects the sample, then gets the results.Can I therefore bill 99211 with urinalysis code 81002? Indiana Subscriber. Answer: No. CPT ® guidelines prohibit reporting 99211 (Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a ...
CPT, or current procedural terminology codes are 5-digit numerical codes used to track and bill medical, surgical and diagnostic services, and determine how much to pay providers. The American Medical Association (AMA) develops the codes and updates the coding system as changes occur in the healthcare delivery field. ICD-10 codes consist of up ...
A billing ZIP code, also known as a postal code, is a five-digit number the United States Postal Service (USPS) assigns to every address in the country. This code helps card companies verify the ...