Cataract Surgery Aftercare: What to Expect and Tips for Recovery

In this article
Cataract surgery is an outpatient procedure that removes a cloudy, dysfunctional eye lens and replaces it with an artificial clear intraocular lens (IOL). 1 The operation lasts under an hour, and the new lenses are maintenance-free.

There are about 28 million cataract surgeries worldwide each year. Approximately 4 million take place in the United States. 2
Cataract surgery aims to enhance your vision. Ophthalmologists combine this operation with other procedures like glaucoma surgery. 3

7 Cataract Surgery Recovery Tips
To promote healing and avoid eye complications, you’ll need to follow the post-operation care guidelines your doctor provides. 8

Below are seven essential recovery tips for cataract surgery:
1. Avoid Driving
Most people can resume driving a day after cataract surgery. However, others experience blurry vision that can last for several days. Operating a vehicle is dangerous in these cases.
To be safe, consider doing the following:
- Find a friend or family member to drive you to and from the surgery
- Plan for reliable transportation for your follow-up appointments
- Consult your doctor first, even when you think you’re fit to start driving again
- Wear a pair of driving glasses or sunglasses to prevent excess light from harming your eyes when you begin driving
2. Avoid Strenuous Activity
Intense activities and certain postures can increase eye pressure and interfere with healing. Therefore, avoid these as much as you can:
- Heavy lifting
- Contact sports
- Specific postures, such as bending that puts your head below your waist
- Sneezing or vomiting
Before returning to regular activities, talk to your doctor about your eyes’ stability and potential risks.
3. Avoid Water Contact
Water contains bacteria and other germs. Exposure to shower, river, or ocean water after surgery can cause an infection.
To be safe, wait at least 24 hours after surgery before showering. Remember to prevent the water from getting in your eyes when you shower. Moreover, speak to your eye doctor before resuming activities like swimming and bathing in the hot tub.
4. Avoid Rubbing Your Eyes
Rubbing your eyes after cataract removal may interfere with the incision site. Your hands can also introduce bacteria to the site and cause infection.
To avoid rubbing your eyes, use the prescribed eye drops to soothe discomfort. Wearing an eye shield at night can also prevent you from accidentally rubbing your eyes while you sleep.
5. Protect Your Eyes
After surgery, your eyes are prone to irritants, dust, and other trauma. Your eye doctor may give you protective sunglasses to shield your eyes during healing.
They may also give you an eye shield to protect them from accidental injury while you sleep. You can also use sunglasses to protect your sensitive eyes from excess light that can lead to discomfort.
6. Avoid Makeup
Avoid applying anything to your face and eyes for at least two weeks. Don’t wear eye makeup, such as mascara, eyeliners, and artificial eyebrows. They can promote bacteria growth and lead to infection.
7. Follow Your Doctor’s Advice
During the first few weeks of recovery, take all correct medication dosages promptly. Contact your doctor immediately if you notice any concerning side effects like vision loss or eye pain.
Listen In Q&A Format
Recovery after cataract surgery, vision center podcast.

What to Expect After Cataract Surgery
After cataract surgery , you can anticipate a period of recovery where certain precautions and steps are necessary to ensure proper healing. Here’s what to expect:
- Discomfort or itching: It’s common to feel discomfort or have an itchy sensation in the operated eye. It’s crucial to avoid rubbing or squeezing the eye to prevent disrupting the healing process.
- Medication: Your eye doctor may prescribe medicated eye drops and antibiotics to prevent infections. They also help manage inflammation and eye pressure. 5
- Eye protection: Use an eye patch or a protective shield over the eye for a few days post-surgery, especially during sleep, to avoid accidental self-injury.
- Follow-up visits: Schedule a follow-up appointment with your doctor within 24 to 48 hours after the surgery. Moreover, continue these visits to ensure a safe recovery.
Potential Side Effects
You may experience the following side effects the first day or two after surgery:
- Blurry vision due to pupil dilation
- Sensitivity to bright light (photophobia)
- Glares and halos around lights
- Gritty and scratchy eyes
- Drooping, swollen eyelids
- Mild pain for a few days
Your pupil will return to its normal size after a couple of days. This change will result in clearer vision.
When Should You Seek Medical Attention After Cataract Surgery?
Seek immediate medical attention if you experience any of the following:
- Decreased or lost vision
- Severe eye pain
- Severe reddening of the eyes
- Sticky eye discharge
- Clouding of the cornea
- Bleeding eyes
- Inflammation
Recovery Time
After cataract surgery, you can expect to see improvements in your vision. Here’s an overview of the recovery timeline:
- Experience clear within a few days post-surgery, though individual healing rates vary
- It may take one to two weeks for some to see images sharply
- Expect complete recovery and healing within eight weeks
- The procedure has a high success rate of about 99%, so complications are rare 6
A possible complication includes cloudiness or posterior capsule opacification, which can develop months to years later. If this occurs, a YAG laser capsulotomy , a straightforward and painless laser treatment, can correct this issue. 7
Preparing for Cataract Surgery
Cataract surgery is safe. However, preparation is essential to ensure optimum results and to avoid complications.
Proper preparation for cataract surgery also ensures that aftercare is easier. Each step of the preparation process can minimize potential complications and optimize the condition of your eyes and general health for surgery.
Before surgery, your eye doctor will conduct an ultrasound test to determine your IOL type. IOL choice depends on eye length and the curvature of the cornea.
To prepare for surgery, you should:
- Stop taking aspirin or anti-clotting drugs, as these may interfere with normal bleeding
- Stop taking prostate medication such as Flomax since these alpha-blockers interfere with iris muscles during cataract surgery
- Avoid wearing makeup such as mascara, eyeliners, and false eyelashes
- Wash your face with soap and water on the day of surgery
- Abstain from drinking alcohol at least 24 hours before the procedure
- Avoid wearing contact lenses at least 3 days before the operation
- Ask a friend or family member to drive you home after surgery because you may experience blurry vision
- Have a friend or family member arrange to drive you home post-operation, as you may have blurry vision
- Use antibiotic eye drops a day or two before the surgery to prevent infection and inflammation 4
- Cataract surgery is the mechanical removal of a cloudy lens and replacement with an artificial one (Intraocular lens or IOL).
- The success rate of cataract surgery is about 99%.
- While cataract surgery is considered safe, preparation is important to ensure optimum results and to avoid complications.
- Successful recovery is possible if you avoid rubbing your eyes, wearing makeup, indulging in strenuous activity, and neglecting your eyes.
- Following the post-op care tips, seeking medical advice, and frequent checkups will promote a successful healing process.
Related Articles

Is Cataract Surgery Painful?
Medically Reviewed by Dr. Melody Huang, O.D.

Lens Replacement Surgery

What to Expect with Cataract Surgery

Cataracts: Symptoms, Causes, Diagnosis & Treatment

Glaucoma vs Cataracts

How Long After Cataract Surgery Can I Drive?
- “ Cataract surgery .” Mayo Clinic, 2023.
- Lindstrom, R. “ Future of cataract surgery seems promising .” Healio, 2021.
- Iwach, A. “ Cataract Surgery and Glaucoma ,” Glaucoma Research Foundation, 2022.
- Kent, C.“ Antibiotics & Cataract Surgery: New Frontiers .” Review of Ophthalmology, 2015.
- “ Recovery-Cataract surgery ,” National Health Service, 2021.
- “ Cataract surgery: What you should know .” University of California, Irvine, 2018.
- Karahan et al. “ An Overview of Nd: YAG Laser Capsulotomy .” National Center for Biotechnology Information, 2014.
- Eghrari, A. “ Cataract Surgery Recovery: 5 Tips From an Expert .” The Johns Hopkins University.

- Find a Lasik Surgeon Near You
- Find Optometrist Near You
- Contact Lenses
Other Links
- Advertise With Us
- Privacy Policy
- Listen to the Podcast
Social Links
Cataract Surgery
A cataract is a cloudy area in the lens of your eye (the clear part of the eye that helps to focus light) . This can make your vision cloudy. Surgery is the only way to get rid of cataracts .
Who needs cataract surgery?
Your eye doctor will probably suggest cataract surgery if you have vision loss that gets in the way of everyday activities like reading, driving, or watching TV.
Your doctor might also recommend surgery even if your cataracts aren’t the main cause of your vision problems. For example, you may need to have cataracts removed so your doctor can see into the back of your eye. This can help them track and treat other eye conditions, like diabetic retinopathy or age-related macular degeneration (AMD) .
You don’t need to rush to have surgery to get rid of cataracts. Ask your eye doctor about the risks and benefits of cataract surgery to decide if it’s right for you.
Keep in mind that if you have cataracts in both eyes, you’ll need to have surgery on each eye at a separate time, usually about a month apart.
How do I prepare for cataract surgery?
You’ll probably need to take a few steps to get ready for your cataract surgery. Your eye doctor will tell you exactly what you need to do.
Before your surgery
- Visit your eye doctor. About a week before your surgery, your eye doctor will do some tests to measure the size and shape of your eye. These tests help your eye doctor choose the right kind of artificial lens (called an intraocular lens, or IOL).
- Use special eye drops. Your eye doctor may prescribe these eye drops to help protect your eye from getting an infection.
- Stop taking some medications. Tell your eye doctor about any medications you take. If you take a medication that could cause bleeding during your surgery, your eye doctor may ask you to stop taking it for a little while.
- Don’t eat or drink the night before. Your eye doctor may tell you to stop eating and drinking several hours before your surgery.
- Clean your eyelids and eye lashes. Your eye doctor may have you clean your eyelids and eyelashes with baby shampoo the night before and the morning of your surgery to get rid of any germs that could cause an infection.
The day of your surgery
Be sure to bring a friend or family member with you the day of your surgery. You won’t be able to drive afterward — so you’ll need someone to make sure you get home safely.
What happens during cataract surgery?
During surgery, your eye doctor will remove the cloudy lens from your eye and replace it with an artificial lens (called an intraocular lens, or IOL). The surgery lasts about 1 hour and is almost painless.
Usually, you’ll be awake during cataract surgery. You might notice lights or motion, but you won’t be able to see what your doctor is doing. Your eye doctor can give you medicine to help you stay relaxed and calm during the surgery .
When you get this surgery, your eye doctor will:
- Put numbing drops into your eye to keep you from feeling anything
- Use tiny tools to cut into your eye, break up the lens, and take it out
- Place the new artificial lens in your eye
After your eye doctor places your new lens, you’ll need to rest in a recovery area outside the operating room for a little while. Before you go home, the medical team will check to make sure you don’t have any problems with your eye.
What happens after cataract surgery?
Your eye doctor will explain how to protect your eye after cataract surgery. They’ll give you eye drops to help your eye heal, and you may need to wear a special eye shield or glasses. You may also need to avoid some activities for a few weeks — like touching your eye, bending over, or lifting heavy things.
Your eye may feel a bit itchy or uncomfortable and sensitive to light and touch. After 1 or 2 days, your eye should feel better.
Call your eye doctor right away if you notice any of these problems after surgery:
- Vision loss
- Bad pain that won’t go away even if you take medicine for it
- Very red eyes
- Floaters — flashes of light or a lot of small dark spots or squiggly lines that float across your vision
Most people are completely healed 8 weeks after their surgery. Your eye doctor will schedule checkups to make sure your eye is healing correctly.
Will my vision be normal after cataract surgery?
About 9 out of 10 people who get cataract surgery see better afterward , but your vision might be blurry at first while your eye recovers.
Some people notice that colors seem brighter after cataract surgery. This is because the artificial lens doesn’t have the noticeable yellow or brown tint your natural lens had from the cataract.
Once your eye is completely healed, you might need a new prescription for glasses or contact lenses to see clearly.
What are the risks of cataract surgery?
Cataract surgery is one of the most common, safe, and effective types of surgery done in the United States. But like with any surgery, there are risks. For example:
- Swelling, bleeding, or infections
- Vision loss or double vision
- Unusual changes in eye pressure
- Retinal detachment
- Secondary cataracts (posterior capsule opacity)
Your eye doctor can treat these problems, but it’s best to start treatment as soon as possible. Be sure to go to all your checkups, and call your eye doctor if you notice anything wrong with your eyes or vision.
Secondary cataracts
After cataract surgery, some people may develop a condition known as a secondary cataract, or posterior capsule opacification. Secondary cataracts can appear weeks, months, or even years after cataract surgery. The good news is your eye doctor can fix them with laser treatment.
Learn more about secondary cataracts
Last updated: January 4, 2023

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Eye Health A-Z
- Glasses & Contacts
- Tips & Prevention
- Ask an Ophthalmologist
- Patient Stories
- No-Cost Eye Exams
- For Public & Patients /
What Are Cataracts?
Cataract Surgery: Risks, Recovery, Costs
BPH Medicine and Cataract Surgery
- IOL Implants: Lens Replacement After Cataracts
- Presbyopia-Correcting IOLs
- Pediatric Cataracts
- How to Choose a Cataract Surgeon
- What Do Cataracts Look Like?

Cataract surgery is an operation to remove your eye’s lens when it is cloudy.
What to Expect with Cataract Surgery
- Cataract Surgery Recovery
What Are the Risks of Cataract Surgery?
Posterior capsular opacification, cataract surgery costs.
The purpose of your lens is to bend (refract) light rays that come into the eye to help you see. Your own lens should be clear, but with a cataract it is cloudy. Having a cataract can be like looking through a foggy or dusty car windshield. Things may look blurry, hazy or less colorful.
The only way to remove a cataract is with surgery. Your ophthalmologist will recommend removing a cataract when it keeps you from doing things you want or need to do.
During cataract surgery, your cloudy natural lens is removed and replaced with a clear artificial lens. That lens is called an intraocular lens (IOL) . Your ophthalmologist will talk with you about IOLs and how they work .
Before surgery:
Your surgeon will measure your eye to determine the proper focusing power for your IOL. Also, you will be asked about any medicines you take. You might be asked not to take some of these medicines before surgery.
You may be prescribed eye drop medicines to start before surgery. These medicines help prevent infection and reduce swelling during and after surgery.
The day of surgery:
Your ophthalmologist may ask you not to eat any solid food at least 6 hours before your surgery.
Cataract removal surgery may be done in an outpatient surgery center or in a hospital. Here is what will happen:
- Your eye will be numbed with eye drops or with an injection around the eye. You may also be given a medicine to help you relax.
- You will be awake during surgery. You may see light and movement during the procedure, but you will not see what the doctor is doing to your eye.
- Your surgeon looks through a special microscope. She creates tiny incisions (cuts, created by blade or a laser ) near the edge of your cornea . The surgeon uses these incisions to reach the lens in your eye. Using very small instruments, they will break up the lens with the cataract and remove it. Then they put your new lens into place.
- Usually your surgeon will not need to stitch the incisions closed. These “self sealing” incisions will close by themselves over time. A shield will be placed over your eye to protect it while you heal from surgery.
- You will rest in a recovery area for about 15 to 30 minutes. Then you will be ready to go home.
How Long Does It Take To Recover From Cataract Surgery?
Days or weeks after surgery:.
- You may have to use eye drops after surgery. Be sure to follow your doctor’s directions for using these drops.
- Avoid getting soap or water directly in the eye.
- Do not rub or press on your eye. Your ophthalmologist may ask you to wear eyeglasses or a shield to protect your eye.
- You will need to wear a protective eye shield when you sleep.
- Your ophthalmologist will talk with you about how active you can be soon after surgery . They will tell you when you can safely exercise, drive or do other activities again.
Like any surgery, cataract surgery carries risks of problems or complications. Here are some of those risks:
- Eye infection.
- Bleeding in the eye.
- Ongoing swelling of the front of the eye or inside of the eye.
- Swelling of the retina (the nerve layer at the back of your eye).
- Detached retina (when the retina lifts up from the back of the eye).
- Damage to other parts of your eye.
- Pain that does not get better with over-the-counter medicine.
- Blurred vision.
- Seeing halos, glare, and dark shadows.
- Vision loss.
- The IOL implant may become dislocated, moving out of position.
Cataract surgery will not restore vision lost from other eye conditions, such as macular degeneration , glaucoma , or diabetic retinopathy .
Your ophthalmologist will talk with you about the risks and benefits of cataract surgery.
Your vision could become cloudy or blurry weeks, months or years after cataract surgery. This is not unusual. Your doctor might call this a “posterior capsular opacification (or PCO).” It's also called " secondary cataract " or "scar tissue." It's not like a scar you get on your skin. But because it happens after the eye has healed from cataract surgery, some people think of it as a scar. It happens when a membrane called the posterior capsule becomes cloudy. It might help to think of the posterior capsule as a transparent pocket. It holds your IOL in place. It also once held your eye’s natural lens (what became the cataract) in place. If you notice cloudy vision again, you might need to have a laser procedure. The laser creates an opening in the cloudy capsule and is called a posterior capsulotomy (or a YAG laser capsulotomy) . This procedure helps restore clear vision.
Cataract surgery costs are generally covered by Medicare if you are Medicare eligible. Private insurance usually covers cataract surgery as well.
Medicare will cover your costs if your vision tests at a certain level of acuity or clarity. Private insurance plans may have similar vision requirements. If your surgery is covered you may still have some costs. Special types of IOLs will cost more . Choosing to have cataract surgery before your vision has deteriorated enough will cost more.
In certain cases, it might be possible to get coverage before you meet the age or vision requirements. Talk with your ophthalmologist if you are considering having early cataract surgery.
What do you do if you don't have Medicare or private insurance coverage? You may still be able to reduce and manage the cost of cataract surgery. Ask about payment plans through your doctor's office. See if your employer offers flexible spending accounts that can help. Your ophthalmologist can help you learn more about costs of cataract surgery. Discuss your options for affording the procedure.
More Cataract Articles
- What Is a Posterior Capsulotomy?
- What Is Monovision (or Blended Vision)?
- Adjustable IOL Could Help Some Ditch Their Glasses After Cataract Surgery
- Can I Fly With This Eye?
Popular Cataract Answers
- Can cataract surgery affect depth perception? (Video Answer)
- How long will I have blurry vision and glare after cataract surgery?
- Is routine pre-operative medical clearance needed before cataract surgery?
- Why have I regained my balance after cataract surgery?
- How is the lens power determined before cataract surgery?
- What are some of the risks associated with not having a cataract removed?
- Can I prevent or slow the development of my mild cataract?
- How long do I have to use the antibiotic eye drops after cataract surgery?
- Is it safe to have an MRI after cataract surgery?
- Does marijuana help cataracts?
- Find an Ophthalmologist Search Advanced Search
Free EyeSmart Newsletter
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
- Ophthalmology Job Center
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients
- Intraocular Lens
- Cataract Surgeons
- 10 Cataract Surgery Side Effects, and How to Cope
Centers Near You
Selected Address
NVISION Procedures
Every NVISION patient is different. We look forward to working with you to determine the best eye surgery or nonsurgical treatment for your individual needs.
- LASIK Eye Surgery
- Contoura® Vision LASIK
- EVO ICL™ (Implantable Lens)
- SMILE™ Vision Correction
- Cataract Surgery
- Comprehensive Ophthalmology
- Lifestyle Lenses
- Vivity Extended Vision IOL
- Cross-Linking
- INTACS® Corneal Implants
- Oculoplastic
- Cosmetic Treatments
- Blepharoplasty
- Dry Eye Treatments
- Glaucoma Surgery
- PDT Eye Treatment
- Monovision LASIK
- Refractive Lens Exchange
- Pterygium Surgery
- Implantable Miniature Telescope Surgery
See Your Best This Winter!
Get $1000 off LASIK + Enjoy Easy and Fast LASIK Financing.**
Nvision conditions.
- Astigmatism
- Nearsightedness
- Farsightedness
- Keratoconus
- Macular Degeneration
- Coronavirus
NVISION Education
- ‣ LASIK Candidate Quiz ‣
- All About LASIK
- LASIK Safety & Success Rates
- LASIK Eye Surgery Cost
- LASIK for Astigmatism
- How Long Does LASIK Take?
- Glasses After Cataract Surgery
- Best Lens for Cataract Surgery
- When to Get Cataract Surgery
- What to Expect: Anesthesia
- Types of Cataracts
- Types of Lenses For Cataract Surgery
- PRK Surgery
- Guide to Laser Eye Surgery
- Types of Eye Surgery
- Corneal Cross-Linking
- Improving Eyesight
- Intraocular Lens
- Survey: America’s Bad Eye Care Habits
- Diet & Vision?
NVISION Locations
Start your journey to clearer vision now and book your appointment with us one of our many locations from our extensive network.
- Inland Empire
- Los Angeles
- Orange County
- Ventura County
- Fort Lauderdale
- Port St. Lucie
- West Palm Beach
- Indianapolis
- Kansas City
- Washington DC
- Minneapolis
- Lincoln City
- Philadelphia
- Corpus Christi
- South Texas
- Salt Lake City
- Virginia Beach
Find a nearby center
Last Updated Jul 13, 2023
Further Reading
- Cataracts & Your Golf Game
- Guide to Medicare Coverage
- Which Lens is Best?
- PanOptix Trifocal Lenses (IOL)
- Transportation Options for Cataract Surgery
- How is Glaucoma Different?
- Dizzy Spells
- Can Cataracts Come Back?
- Identifying Cataracts
- Do Natural Cures Work?
- What Happens When Left Untreated?
- Congenital Cataracts
- Stages: When to Get Treatment
- Insurance Coverage for Cataracts
- Can They Cause Blindness?
- Fast-Developing Cataracts
- What Is YAG Laser Capsulotomy?
Post-Cataract Surgery – Timeline and Tips for Recovery
Home / Cataracts / Post-Cataract Surgery Recovery
Table of Contents
- Recovery Timeline
- Recommendations
- Recovered Vision
Frequently Asked Questions
Recovery from cataract surgery generally takes two to four weeks. You’ll want to be very careful with your eye following cataract surgery.
Your ophthalmologist will provide you with clear, detailed instructions for the hours, days, and weeks after your cataract surgery.
General tips for post-cataract surgery care include:
- Avoid heavy lifting or strenuous exercise for a few weeks.
- Do not bend over for a couple days.
- Avoid swimming for the weeks following surgery.
- Protect your eye from irritants.
- Don’t rub your eye.
Post-Cataract Surgery Care: Timeline & Stages
Cataract surgery is most often an outpatient procedure , so you will be able to go home the same day your cataract is removed. This means that most of the recovery process will be at home, with some follow-up visits to your ophthalmologist to make sure your eye is healing properly. It is important to closely follow your ophthalmologist’s guidelines for recovery, so you are at less risk of developing complications from the procedure, like inflammation, infection, swelling in the retina, pain, detached retina or lens, and vision loss.
Your ophthalmologist will give you a more detailed schedule of the recovery timeline and expectations, but here are some general recommendations to follow after cataract surgery.
Immediately After Surgery
Once cataract surgery has been completed, and your time in the recovery area has allowed initial recovery from sedation, you can return home. Because some of the medication effects will linger for 24 hours and your vision will be impacted immediately after surgery, it is not safe to drive yourself home. It is important that you have someone you trust take you back home after the procedure. While this is typically an outpatient operation, it is still an operation, and you may experience grogginess, discomfort, or pain after the surgery. Normal side effects in the first day after surgery include:
- Watery eyes.
- Feeling like you have grit in your eyes.
- Blurry or double vision.
- A red or bloodshot eye.
You may receive medicated eye drops to treat discomfort and reduce the risk of swelling and infection. You should also receive a pair of sunglasses to protect your eyes from the glare of the sun or lights, and it is important to wear these for the length of time recommended by your ophthalmologist. To ensure the safety of your eyes overnight, you may also receive an eye patch, shield or a protective visor to wear to bed so your eye is not hit or poked in your sleep.
A Few Days Later
You may still experience some physical discomfort in the eye that underwent cataract surgery, but these symptoms should begin to clear up within 24 to 48 hours after the procedure. You may be using medicated eye drops for several days to weeks after the procedure, which may require cleaning around the outside of your eye. Follow your eye doctor’s instructions for this very closely to avoid getting anything, aside from the prescribed eye drops, in your eye.
After you return home, you should be careful not to get soap and water directly into your eye for the period of time recommended by your ophthalmologist. Although you should be able to perform normal activities like showering within a day after this outpatient surgery, you may need to protect your eye while you bathe. You should also avoid many hair products, perfumes, face washes, lotions, and makeup for a few days while your eye heals. You may wear special eyeglasses for a few days after surgery to prevent you from poking, rubbing, or scratching your eye. Mild itching and discomfort are common for a few days after the procedure, but it is important to avoid touching your eye during this time.
After two to three days, this itching and discomfort will clear up. If it does not go away, or it gets worse, speak with your doctor. You may need to wear glasses to correct your vision. Although your vision should become clearer within a day or so after surgery, you may need help seeing objects up close if you have the basic monofocal lens implanted because this lens will not correct for different ranges of sight. Toric lens implants will correct astigmatism and usually aid in distance vision without glasses, while premium lenses will usually reduce the need for any prescription for distance and near vision tasks
While you can perform many basic activities the day after surgery, like watching television and moving around your house, more strenuous activities should be avoided. Your ophthalmologist will work with you to determine which aspects of your lifestyle are safe to perform, such as reading, up-close hobbies like sewing, driving, or physically strenuous activities like exercise. It is important to follow your ophthalmologist’s advice closely because you are at risk of dislocating the new lens.
Typically, you will see your ophthalmologist a day or two after your surgery. You may still need help getting to and from your eye doctor’s office. You will have another follow-up exam a week or two later.
If you have cataracts in both eyes that require surgery, your ophthalmologist will typically operate on one eye first, wait for the eye to recover, and then schedule the second surgery. While this lengthens your overall vision recovery time, this allows for for an adjustment period, so you can see out of one eye and know whether there may be complications during the healing process. A one to two week wait before the second eye is typical, though in some cases it may be longer and same day sequential surgery for both eyes, while relatively uncommon, is sometimes recommended.
Weeks Later
While you can expect considerable vision improvement in one to three days after surgery, it can take between three and ten weeks for your vision to improve as much as possible. In particular, if you elect the premium lens implant option to give better focus without glasses at distance and near, your vision while good initially may continue to improve for 6 months or even longer.
Your final post surgical follow-up exam with your ophthalmologist should be about one month after your surgery. This is the standard expected recovery time, though each eye can vary. With the exams before the one-month mark, your eye doctor should be able to catch any problems that come up after cataract surgery and treat these as needed.
Colors may seem brighter quickly and your vision should be clearer overall within days though as above best vision will take weeks or sometimes longer. While with the basic single vision lens implant you are not likely to recover perfect, or 20/20 vision, you are likely to have 20/30 or 20/40 vision without any corrective wear like glasses unless there is a moderate to large amount of preoperative astigmatism that is not corrected with a toric lens implant. This level of vision usually qualifies for driving without glasses though corrective lenses are needed for any near work. Once your eyes have healed fully after cataract surgery, your doctor will give you your final eyeglass prescription. This is not likely to change much over time because the artificial lens in your eye will not change shape or clarity like a biological lens would.
Recommendations for After Cataract Care
In the days and weeks after your surgery, it is recommended that you:

- Use prescription eye drops as detailed by your ophthalmologist.
- Follow all the recommendations of your ophthalmologist and/or eye surgeon.
- Rest and relax for two to three days.
- Use your eye shield every night for at least one week.
- Wear the eye shield while showering, especially if washing your hair.
- Perform normal, low-impact activities like using a computer, reading, or watching TV as normal.
- Avoid swimming during recovery for four to eight weeks.
It is important to avoid for four to eight weeks:
- Rubbing your eye.
- Getting foreign objects in your eye, like shampoo.
- Performing strenuous activities like running, swimming or yoga.
- Driving before getting the all-clear from your eye doctor.
- Flying without your doctor’s knowledge and approval.
You can return to work a few days or weeks after the procedure, depending on what type of job you have.
Recovered Vision Is Likely After Cataract Surgery
It is important to follow your eye doctor’s instructions for at-home, postoperative care. Attend all follow-up exams so your doctor can ensure your eye is healing properly. If you experience problems with your vision, ongoing or worsening discomfort or pain, swelling, or redness, or loss of vision, report these to your doctor immediately.
Because cataract surgery has been performed for decades and the technology used has progressively improved, it has a high success rate and a low rate of complications . When you do undergo cataract surgery, the bulk of your recovery time will be at home, so it is important to understand exactly how to take care of yourself, which your ophthalmologist will make clear.
Is cataract surgery painful?
Patients usually don’t experience any pain during cataract surgery. Numbing drops are used beforehand, so you won’t feel pain.
Do I need to have my cataract removed immediately?
Not necessarily. Doctors often monitor mild cataracts rather than removing them. Sometimes, a cataract will never develop to the point where it needs to be removed. Once it starts impacting vision, it is generally time to remove it.
Does insurance cover cataract surgery?
Most health insurance plans , including Medicare , will cover cataract surgery.
How long do I need to take off work?
Most people return to work within a day or two if your job does not require significant physical activity. You can return as soon as you feel comfortable to do so.
Can I drive myself home after cataract surgery?
No. You will be unable to drive, so you must have someone drive you home.
- Cataract Surgery . (March 22, 2018). Mayo Clinic.
- Cataract Surgery Recovery . (October 2016). All About Vision.
- Cataract Surgery . (November 9, 2018). American Academy of Ophthalmology (AAO).
- Recovery: Cataract Surgery . (December 14, 2017). National Health Services (NHS).
- Cataract Surgery: What to Expect at Home . (December 3, 2017). MyHealth.Alberta.ca.
The information provided on this page should not be used in place of information provided by a doctor or specialist. To learn more, read our Privacy Policy and Editorial Policy pages.

- Are Premium Cataract Lenses Worth the Extra Cost?
- Cataract Surgery – What Are the Three Types of Cataract Lenses?
- What is the Success Rate of Toric IOL Implantation?
- Cataract Surgery – What Are the Different Lenses in Each Eye?
- What is the Most Advanced Cataract Lens?
- Cataract Surgery
- LASIK Surgery
- PRK Surgery
How Many Doctor Visits After Cataract Surgery Are There?
Cataract surgery is an outpatient process that typically lasts less than an hour, during which your physician will remove and replace your natural lens with an artificial plastic one.
Although cataracts are uncommon, if you do have them it’s essential to stay in touch with your physician regularly for check-ups in order to avoid serious complications like retinal detachment.
Your first few days after surgery may include discomfort, sensitivity or blurred vision – these symptoms are normal and will ease over time. Your doctor will prescribe eye drops and oral medications to prevent infection and reduce inflammation; be sure to take these as instructed. Also wear shields or eye glasses for added protection from dust or debris entering your eyes.
Cataract surgery entails replacing your eye’s cloudy lens with an artificial plastic lens implant. Two techniques may be used: phacoemulsification or extracapsular cataract extraction.
Experienced ophthalmologists can perform cataract surgery with remarkable skill, while new cataract surgeons must first build up enough surgeries during training before becoming proficient at performing it safely and predictably. On average, new cataract surgeons typically conduct approximately 200-300 cataract operations during their training period in order to ensure safe and predictable outcomes; it is important that patients recognize and understand this difference between new and experienced cataract practitioners.
Cataract surgery is one of the most frequently performed surgeries in the US. This process replaces your natural cloudy lens with an artificial one to restore clear vision. After surgery, colors may seem brighter.
Your doctor will numb your eye for this approximate 15-minute procedure known as phacoemulsification, which should leave it feeling comfortable after. Aftercare instructions include refraining from strenuous activity and using makeup; additionally, eye drops must be used as directed.
Your eye may experience mild pain and itching for one or two days following cataract surgery; these symptoms should resolve as your cataract heals. Acetaminophen or ibuprofen can help alleviate these discomforts.
Studies have revealed that an initial postoperative visit after cataract surgery may not be necessary due to low rates of complications among those undergoing uncomplicated surgeries and with no ocular or systemic comorbidity; however, doctors can use this opportunity to identify patients more readily who require management changes with greater sensitivity.
After one week post-surgery, it is essential that you visit your physician to check on how well the eye has recovered. Any swelling should have subsided by now and vision should be clearer than it was shortly following your procedure.
At this visit, your doctor will perform a comprehensive exam on both of your eyes, test visual acuity and measure eye pressure before discussing how best to utilize prescription eye drops as well as when it might be time for new glasses.
At night, you should wear an eye shield to sleep, in order to protect it from debris or objects that could irritate the surgical wound. Your doctor may suggest wearing sunglasses or a hat with a brim to shield from sunlight as well as continue with prescribed eye drops at this time.
After surgery, you may experience discomfort and blurriness of vision for several days afterward. These effects should lessen over time; usually within a week or two they should fade.
Your doctor may prescribe eye drops or medications to protect against infection, inflammation, and high pressure in your eye. They may also advise wearing an eye shield at night to ensure the operated eye remains safe from damage.
Researchers conducted one study and discovered that suboptimal vision at four weeks was comparable between patients who came independently for follow-up visit after cataract surgery, and those reviewed directly afterward. This was significant as it indicated that delaying initial ophthalmic review after cataract surgery may be safe; however if any symptoms arise that cannot go undetected by patients themselves (i.e. persistent pain, increased redness or decreased vision), care must still be sought immediately at a hospital – these include persistent discomfort, increased redness or diminished vision that require immediate hospital attention (ie persistant pain, increased redness or diminution).
At this stage, your eye doctor will want to assess how well your eye is healing and improving; your vision should still be blurry but more clear than it was immediately following surgery. Furthermore, they will give instructions for using any prescribed antibiotic or anti-inflammatory eye drops multiple times daily.
Your surgeon will inform you when it is time to receive a new glasses prescription; generally it takes between one and three months post-cataract surgery for eyes to heal completely and gain enough focusing power for you to achieve the visual result you are after.
Cataract surgery is one of the most frequently performed surgeries in the US and it has very few complications, with most experienced surgeons boasting a complication rate below 5% and major complication rates being less than 1/2000. Therefore, cataract surgery should be seen as a safe procedure; just make sure that you follow all postoperative care instructions provided by your surgeon!
At this point, your vision should begin to stabilize. Although you may still experience blurriness or distortion at first, these symptoms should gradually decrease as your eye heals. At this appointment, your doctor will ensure the intraocular lens implant is centered correctly and that both eyes are healing properly; additionally they’ll give detailed instructions for using eye drops that reduce infection and inflammation.
Your doctor may prescribe medication to address any eye-related symptoms you are experiencing, so be sure to follow any prescriptions given and contact him or her immediately if there are new issues or any concerns with regards to recovery.
If your eyes are still dilated and sensitive, arrange to have someone drive you home after this appointment. In order to give them time to recover fully, avoid strenuous activity like contact sports as well as strenuous physical exertion such as weight lifting. Furthermore, wearing sunglasses when going outside would be ideal.
Your doctor will conduct tests a week or two prior to surgery in order to assess the size and shape of your eye, in order to select an artificial lens suitable for you. They’ll also provide eye drops so you can use prior to any scheduled procedures.
Cataract surgery entails extracting your cloudy natural lens and replacing it with an artificial one that will enhance your vision. This procedure should significantly increase visual clarity.
Most patients can resume their daily activities within a few days following surgery, though if driving is required for any reason you should make arrangements for a friend or family member to drive you home from the procedure.
Adherence to your physician’s post-op care schedule is crucial for successful and timely healing from eye surgery. Most people should attend appointments the day after, one week later, and one month post procedure; however if complications or special circumstances arise additional visits may be required.
After one to two weeks have passed since cataract surgery, doctors typically arrange another appointment to monitor for complications like leakage of surgical wound or cloudiness of new lens implant. They dilate eyes and measure eye pressure at these appointments in order to make sure iris has healed correctly, that there have been no complications and that implant is centered in eye.
Doctors also evaluate the results of each procedure and test visual acuity during these visits, giving patients an opportunity to voice any queries or raise any concerns that they might have.
Cataract surgery should only be carried out by surgeons with sufficient experience of performing this process. An average cataract surgeon performs around 350 cataract surgeries annually, giving them ample opportunities to refine their surgical skills and speed up the procedure. Patients looking for one with extra expertise should seek referral from either their primary care physician or optometrist.
Cataract surgery is one of the safest surgeries performed in America. Even experienced surgeons may experience complications that range from minor to major. Therefore, follow-up appointments after cataract surgery are so vital.
At this point, your eyes should feel better and an ophthalmologist will evaluate the site of incision. They may also offer additional bathing instructions, physical activity restrictions and eye drop usage tips.
Recent survey of cataract surgery clinics in Sweden demonstrated it is possible to reduce visits without jeopardizing patient safety. If all cataract surgeons adopted this routine, resources would become available for other patients more effectively. For patients without ocular or systemic comorbidities following successful cataract surgery (phacoemulsification or MSICS), follow-up appointments could safely be deferred for four weeks after an uneventful procedure – saving both money and time for these patients.
You Might Also Like
Recent posts, recent comments.
Sign in to your account
Username or Email Address
Remember Me
- Blurry Vision
- Conjunctivitis - Pink Eye
- Corneal Abrasions
- Eye Discharge
- Dilated Pupils
- Eye Infections
- Eye Twitching
- Ocular Migraines
- Swollen Eyelids
- How to Get Rid of a Stye
- Blepharitis
- Eye Floaters
- Myopia in Children
- Myopia (nearsightedness)
- Astigmatism
- Contrast sensitivity testing
- Refractive errors and refraction
- Visual Acuity: 20/20 Vision
- Hyperopia (farsightedness)
- Digital Eye Strain
- Computer Glasses
- Kids & Screen Time
- Blue Light and Vision
- Blue Light Glasses
- How to Choose Eyeglass Lenses
- Anti-reflective Lenses
- Progressive Lenses
- Eyeglass Lens Coatings
- Photochromic Lenses
- Multi-focal Lenses
- Eyeglass Frame Materials
- How to Clean Your Glasses
- What do the numbers on your eyeglass frames mean?
- Eyeglass temples: How do you know if they're the right length?
- Can you be allergic to eyeglasses?
- The Best Glasses for Your Face Shape
- Pupillary Distance
- Glasses for Round Faces
- Glasses for Small Faces
- Glasses for Long Faces
- Sunglasses for Oval Faces
- How Much Do Glasses Cost?
- Cheap Glasses
- Choosing Eyeglasses
- Best Places to Buy Glasses
- How to Solve Problems with New Glasses
- Styles: Trends in Men's Glasses
- Polarized Lenses
- Prescription Sunglasses Guide
- Ray-Ban Wayfarer Guide
- Performance Sunglasses
- Are Designer Shades Worth It?
- How to Spot Fake Wayfarer Sunglasses
- Guide to High-Quality Sunglasses
- Tint Guide for Sports Sunglasses
- UV Radiation and Your Eyes
- Contact Lens Basics
- Reading a Contact Lens Prescription
- Soft Contact Lens Care
- Daily Disposable Contacts
- Buying Contacts Without a Prescription?
- Bifocal Contacts
- Toric Contact Lenses
- Colored Contacts
- Multifocal Contacts
- Gas Permeable Contact Lenses
- Scleral GP Contact Lenses
- What is vision insurance?
- How to Use Vision Insurance Benefits
- Check Your Vision Insurance Benefits
- EyeMed Vision Insurance
- VSP Vision Insurance
- Vision Insurance or Vision Benefits Plan
- Vision Insurance Provider List
- Provider Networks and Vision Insurance
- What is Covered by Vision Insurance?
- Medicare & Medicaid Vision Benefits
- Medicare Advantage Plans (Part C Plans)
- Medicaid: Eligibility and Vision Benefits
- How to Get Free Eye Exams and Glasses
- LASIK Eye Surgery Guide
- Cost of LASIK
- LASIK Risks
- How Long Does LASIK Last?
- Does LASIK Hurt?
- Do I Have To Be Awake During LASIK?
- PRK Surgery
- SMILE Laser Surgery
- Epi-LASIK Surgery
- Lens Replacement Surgery
- LASEK Eye Surgery
- PresbyLASIK
- Cataract Surgery
- Laser Cataract Surgery
- Cataract Surgery Video
- Cataract Surgery Recovery
- Cataract Surgery Complications
- Cataract Surgery Cost
- What to Expect During Eye Exams
- Free Eye Exams
- What is an Eye Test?
- How to Read Your Eyeglass Prescription
- How to Choose an Eye Doctor
- Infant vision development
- Are contact lenses a good choice for kids?
- Reading glasses: Tips before you buy
- How older drivers can improve their driving at night
- Lutein & Zeaxanthin
- Eye Vitamins and Supplements
- Omega-3 Fatty Acids
- Safety Glasses
- Sports Glasses & Goggles
- Eye Safety Basics
- Contact Lenses for Sports
- Shooting Glasses and Hunting Eyewear
- Ski Goggles
- Eye Diagram
- Baby's Eye Colors
- Dominant Eye Test
- Color Blindness
- Color Blind Tests
Cataract surgery recovery: 8 tips to minimize recovery time
By Marilyn Haddrill ; contributions and review by Charles Slonim, MD
Your cataract surgery recovery should be short and uneventful, as long as you follow the post-op instructions you receive from your surgeon and attend all recommended follow-up visits with your eye doctor .
Uncomplicated cataract surgery usually takes no longer than about 10 minutes to perform. Immediately after the surgery, you will rest in a recovery area until you are less groggy from sedation or anesthesia. Typically this takes about 30 minutes to an hour.
You must have someone available to drive you home after the procedure. You'll be given a pair of sunglasses to wear on the trip home to protect your eye from bright light and glare.
If you are sleepy or tired when you get home, you might want to rest in bed for a few hours. Depending on the advice you receive from your cataract surgeon , you may be able to remove the protective shield placed over your eye within several hours after the procedure.
Just remember that you will need to tape the shield back over your eye at night or during naps, for protection while you recover from cataract surgery, at least for several days.
What is a typical cataract surgery recovery time?
Don't be alarmed if your vision seems cloudy, blurry or distorted when you first remove the eye shield. It can take some time for your visual system to adjust to the removal of the cataract and adapt to the intraocular lens used to replace your eye's natural lens.
During this adaptation period, some patients even report seeing "wavy" vision or distortions. This phenomenon, if present, should last only an hour or so.
You may also develop red and bloodshot eyes because of temporary damage to blood vessels on the "white" of your eye ( sclera ) during cataract surgery. As your eye heals, the redness should dissipate within several days.
If you received an injection of anesthesia through the skin into the lower portion of your eye, you may notice some bruising similar to a black eye . This, too, should fade within a few days.
Many patients report clear vision within several hours after cataract surgery. But each person heals differently, and you may need as long as a week or two before you see images in their sharpest focus.
Typically, you will have a follow-up appointment with your cataract surgeon the day after the procedure to make sure there are no complications. If you don't notice any improvement in blurry vision or you feel eye pain or significant discomfort in the days following this visit, you should report this to your surgeon.
Sometimes people report some dry eye or "scratchiness" after cataract surgery. These sensations should subside as your eye heals, unless you already had problems with dry eyes prior to having the procedure.
Your full cataract surgery recovery should occur within about a month, when your eye is completely healed.
How to get the best cataract surgery recovery?
You might be surprised at how good you feel and how easy it is to resume normal activities even the day after cataract surgery.
However, you should observe a few precautions during the first week or so, to make sure you avoid any complications during your cataract surgery recovery.
Your eye doctor typically will prescribe antibiotic eye drops to prevent infection and anti-inflammatory eye drops to help reduce any internal inflammation. You'll need to apply the eye drops several times daily for about the first week following surgery.
Depending on the amount of postoperative inflammation you have, you may need the drops for a few weeks to a month. Make sure you use these eye drops exactly as prescribed.
Oral pain relievers such as acetaminophen may be prescribed, if needed. Typically, however, you should feel only slight discomfort after cataract surgery.
For a safe and speedy cataract surgery recovery, follow these tips:
Don't drive on the first day following surgery .
Don't do any heavy lifting or strenuous activity for a few weeks.
Immediately after the procedure, avoid bending over to prevent putting extra pressure on your eye.
If at all possible, don't sneeze or vomit right after surgery.
Be careful walking around after surgery, and don't bump into doors or other objects.
To reduce risk of infection, avoid swimming or using a hot tub during the first week of your cataract surgery recovery.
Don't expose your eye to irritants such as dust, dirt, wind and pollen during the first few weeks after surgery.
Don't rub your eye after surgery.
Generally speaking, you should be able to perform these activities within a few hours of your surgery:
Computer work
Light TV watching
Showering or bathing
For the best cataract surgery recovery possible, follow your doctor's detailed instructions about how to protect your eye following your procedure. Usually these instructions will be given to you as a handout that you can take home with you on surgery day.
If you need cataract surgery in both eyes, your surgeon usually will wait at least a few days to two weeks for your first eye to recover before performing a procedure on the second eye.
Cataract surgery recovery and typical outcomes
Cataract surgery is one of the safest and most commonly performed surgical procedures in the United States. More than 3 million cataract surgeries are performed in the U.S. each year, and most people have excellent outcomes with no cataract surgery complications .
Past studies show:
Almost 96% of eyes that had no other problems such as other eye diseases prior to a cataract procedure achieved at least 20/40 uncorrected distance visual acuity, which legally is good enough to drive without eyeglasses or contact lenses .
In all eyes, including those with pre-existing eye conditions other than cataracts, almost 90% of all patients had good outcomes.
Fewer than 2% of eyes that undergo cataract surgery have sight-threatening complications after the procedure.
In rare cases, sight-threatening cataract surgery complications such as endophthalmitis — an inflammation of the inside of the eye, usually caused by an eye infection — can occur.
People who experience serious complications often have other health conditions such as diabetes or high blood pressure.
A relatively common complication of cataract surgery that usually can be treated easily is posterior capsular opacification (PCO), which can cause your vision to become cloudy months or years after cataract removal. A simple laser procedure called a posterior capsulotomy usually can clear up the cloudiness and restore sharp vision.
READ NEXT: Refractive cataract surgery
Page published on Wednesday, February 27, 2019

Schedule an exam
Women’s vision: Understanding risks and ways to protect it

Alice in Wonderland syndrome (AIWS)

Horizontal gaze nystagmus (HGN)
How to limit your child’s screen time with digital apps, ray-ban stories: features, pros and cons, how dirty are your facial tools.

An OD’s Guide to Postoperative Cataract Care
Practical advice for both routine and complex cases..
By Oliver Kuhn-Wilken, OD
Providing care for your patients during their recovery from cataract surgery can be exciting and gratifying. Few experiences will cement patients to your practice like regaining their vision; it will also help your clinic operate at the peak of its capacity. Most patients have a straightforward recovery, and only a few require more attention. If any serious problems present, your surgeon is standing by, ready to assist. 1
Each month, our clinic and the community optometrists we serve see hundreds of cataract patients through their healing process. This article describes the sequence and elements of an uncomplicated recovery from cataract surgery and then discusses how to handle some of the more common complications.
The Uncomplicated Course
The vast majority of cataract cases undergo an uncomplicated and predictable path; in the United States today, more than 97% of all cataract cases unfold successfully. 2 Timeline, medications and care have all been standardized for decades.
Medications. All cataract patients will require medications postoperatively to protect them from infection, inflammation and pain, but a wide variation exists in the specific medications and dosages used by individual surgeons. All formulas include an antibiotic to protect against endophthalmitis and a steroid to control inflammation. A steroid used for less than a month can be stopped abruptly when the bottle is empty, although many clinics will ask for the more traditional taper.
Some clinics use a nonsteroidal anti-inflammatory drug (NSAID) to complement the steroid in controlling inflammation and pain, while others do well without them. Regardless, NSAIDs are frequently prescribed for patients whose eyes have a high risk of developing cystoid macular edema (CME) or inflammation: this includes cases of diabetic retinopathy, epiretinal membranes, a history of retinal vein occlusion or macular degeneration.
A growing movement urges doctors to skip some, or all, post-op drops in favor of an injection usually containing a steroid and an antibiotic. In these cases you must be familiar with your surgeon’s mixture and its expected performance. This approach can produce some harmless but unusual visual effects immediately after surgery and has a rare but significant risk of a dangerous reaction to the medication. 3
The one-day exam. Use the first postoperative exam to ensure that the surgery was carried out well, to verify that the patient understands their responsibilities and to answer their immediate post-op questions and concerns. The one-day exam must include a history, measurement of visual acuity (VA), an auto-refractor reading or pinhole acuity, an intraocular pressure (IOP) check and a slit-lamp exam.
For most patients, normal symptoms at the one-day exam include blur, foreign body sensation, ache and redness. Normal findings include reduced VA (typically around 20/25 to 20/60), a small ptosis (from the spring clamps used during surgery), residual dilation, mildly elevated IOP, injection and cells and flare in the anterior chamber.
There will be a primary incision, either in the temporal cornea or in the superior conjunctiva, along with one or two small corneal port incisions. Subconjunctival hemorrhages are common, especially following femtosecond-laser assisted surgery and among patients taking anticoagulants. Often, you will see some mild keratitis; grade 2+ or less should only need the diligent application of artificial tears to restore comfort. There will usually be some disruption of the endothelium (“snail tracks”) and small fragments of capsular debris in the anterior chamber; these are inconsequential and self-resolving. The intraocular lenses (IOL) should be well-positioned. Often, patients will feel sore, have a mild headache or will have slept badly; it is appropriate for them to resort to their over-the-counter oral NSAID of choice for this. The retina need not be examined at the one-day exam unless you or the surgeon have specific concerns.
Any comanaging optometrist must be comfortable grading anterior chamber inflammation, as this is used to judge progress throughout the post-op period ( Table 1 ).
It is important at this time to confirm that the patient understands their drop regimen. Exhorting frequent artificial tear usage and the vigorous shaking of any steroid suspensions can avoid many subsequent panicked late-night phone calls. It’s also a good time to remind patients of their post-op restrictions, which usually include avoiding eye-rubbing, make-up or tap water near their eyes.
The one-week exam. Every patient should be seen between seven and 14 days after each eye’s surgery; this exam is used to verify that the incisions have healed enough to discontinue the patient’s antibiotics, monitor their refractive state and, often, to check for a satisfactory outcome so as to green-light their fellow eye for surgery. If so prescribed, you will ask the patient to begin tapering their steroid. The early signs of endophthalmitis can occur at this point, as well as CME, so be wary of unexplained inflammation, pain or poor vision. 4
Although mild anterior chamber inflammation and mildly reduced vision are standard, all findings should be stable or improved compared with the one-day exam. The one-week exam must include a history, a measurement of aided and unaided VAs, an IOP check and a slit-lamp exam of the anterior segment. A dilated fundus exam is called for only if there are concerns.
The one-month exam. Typically, the patient will have one final exam three to six weeks after surgery. This one must include a dilated fundus exam to confirm the patient is well-healed and stable, and also a final postoperative refraction and prescription. The patient should be relatively asymptomatic, with the exception of refractive error complaints.
If all has gone well, this exam transitions the patient back to their regular eye care schedule. Be sure to review their ocular health, be explicit about the recommended frequency for eye exams and discuss the importance of adequate ultraviolet light protection now that their cataracts are gone. You may ask them to stop their drops at this point.
Expectations. If a patient enters into surgery expecting an improvement in vision after a measured recovery, a significant amount of work instilling eye drops, absolute presbyopia and some amount of residual refractive error, that patient will likely be pleased at every step. If you have the misfortune of caring for a patient who is expecting a perfect outcome, you will have to spend some time working through their unrealistic expectations. Any experienced surgery center will work hard to ensure that all patients have an accurate understanding of what the cataract surgery process will and will not deliver.
Premium IOLs. These introduce a different set of expectations for the postoperative period. These patients have invested in an IOL expecting higher visual performance and will require more care.
Toric IOLs can greatly reduce the patient’s astigmatism; use each postoperative exam to verify the patient’s refraction and satisfaction. The toric IOLs now available in the United States can correct corneal astigmatism between 1.03D and 4.11D—they don’t eliminate irregular astigmatism or astigmatism higher than 4.11D.
Multifocal IOLs are expensive and high performing, but require a significant amount of education and careful screening of candidates. Patients tend to have high expectations and some anxiety about their vision, and you will need to be well-versed in the details of the multifocal IOLs preferred by your surgeon to adequately counsel your patients. Appropriate expectations are crucial, and you must carefully counsel patients preoperatively to expect glasses wear for some specific tasks after surgery. Visual performance can increase for up to six months after implantation of multifocal IOLs as the patient’s neural pathways grow increasingly facile at working with an altogether new way of seeing, and your encouragement can help tremendously along the way.
The ability to accurately grade anterior cells is crucial to evaluating postoperative inflammation. In a darkened room, create a high-intensity, high-magnification field with a 1mm by 1mm slit beam at a 30º to 60º angle. Carefully differentiate between pigment granules (dark brown clumps, common after complex surgeries or small pupils), red blood cells (tiny red spots, unusual) and actual inflammatory cells: small white motes, primarily lymphocytes with some neutrophils. Count the number of inflammatory cells in your beam at a single moment. Any layer of hypopyon is unusual and should precipitate a search for endophthalmitis. Flare will cause the aqueous humor to appear smoky.
Complications
While most cataract patients recover without a hitch, a few may encounter one of these complications:
IOP rise. We often see pressure spikes, whether from retained viscoelastic, or from the impact of inflammation on the trabecular meshwork, after surgery. Fortunately, this spike is transient and usually resolves within the first few days. 5
If the optic nerve is healthy, our clinic will only treat the IOP if it is greater than 30mm Hg by Goldmann tonometry. If the pressure is 30mm Hg to 35mm Hg, often a single drop of brimonidine suffices; if it is higher than 35mm Hg, we will instill brimonidine and sometimes timolol and re-measure the IOP every 30 minutes until the pressure sinks below 30mm Hg. Prostaglandins are next to useless in this case due to their slow action. If the pressure is slow to recover we prescribe a bottle of brimonidine BID for a week. In general, we avoid “burping the wound” due to the risk of infection from backflow.
If the patient has glaucoma, IOP will require more aggressive treatment, based on the glaucoma severity and the stubbornness of the pressure. 6 We keep a bottle of acetazolamide 250mg tablets in the clinic for use in dangerous situations; we give them at a QID dosage until IOP returns to its habitual level, and never for more than a month. Do not be afraid to continue the steroid at full strength in glaucoma patients, as the calming of their trabeculitis may actually help lower pressure. The first recourse should always be to add hypotensive drops and pills to control pressure, reserving an aggressive steroid taper for cases in which this doesn’t work.
Corneal edema. This complication is common and often self-resolving in the first few days or weeks after cataract surgery, but will dramatically affect vision until it clears—usually causing the patient much anxiety. As blur may arise from several factors, it is crucial to rule out a retinal detachment even in cases of evident corneal edema. Immediate post-op corneal edema will come from one of three sources, each treated slightly differently. Examine all layers of the cornea carefully; edema can manifest as microcysts or even bullae at the epithelium, as thickening of the stroma or as folds in the endothelium.
If corneal edema was caused by surgical trauma, it will usually present as stromal thickening and endothelial folds; you may consider adding hypertonic sodium chloride 5% ointment at night if this is severe, but generally this will resolve with time. If the edema is caused by a transient loss of endothelial cell function due to inflammation, you will see 3+ to 4+ cells in the anterior chamber; consider doubling the steroid. If IOPs are greater than 30mm Hg, the hydraulic pressure is likely creating the edema by driving aqueous into the cornea; add timolol or brimonidine to lower IOPs. You may have to employ several tactics simultaneously. 7
Any persistent bullae should trigger a phone call to the surgeon. If no improvement is seen after three months, this unfortunate patient will soon be talking to a surgeon about a corneal surgery.
Inflammation. Complex surgeries (e.g., dense cataracts, poor dilations and torn posterior capsules) tend to ignite a vigorous inflammatory response. 8 Known cases of uveitis, diabetes or other pre-existing inflammatory diseases are expected to struggle with inflammation. Some patients will even have a post-op uveitis without a difficult surgery.
Your first action should be to search for indicators of endophthalmitis or retained lens material. A hypopyon is a dangerous sign. Having ruled these out, you may simply proceed to dampen the inflammation using stronger or more frequent steroids. If there is a risk of CME, add an NSAID back into the mix. Consider a subconjunctival steroid injection and a surgeon consult if the reaction proves stubborn.
Cataract fragments. Occasionally, lens fragments are inadvertently left in the eye by even the most experienced surgeons. They are most commonly found in the inferior anterior chamber angle or hidden in the capsule equator behind the iris. 9 Any unusual level of cells in the anterior chamber should prompt a gonioscopic search of the angle, but a fragment behind the iris will be hard to find.
Lens cortex fragments hydrate and appear fluffy, like cotton; often the eye will melt these away within a few weeks’ time, but, in the meantime, you must control the inflammation carefully. Retained nucleus will look more solid and waxy. This will arouse a greater inflammatory reaction and necessitate a return to surgery for extraction.
You should notify your surgeon of every fragment you notice, even if it is self-resolving.
Refractive surprise. Despite decades of improvements in accuracy, around 26% of patients end up missing their desired refractive target by greater than +/-0.50D. 10 If they have undergone LASIK in the past, this number doubles to more than 50%. 11 This occurrence, especially if compounded by natural astigmatism, can lead to great disappointment; once again, any seeds of unrealistic expectations will bloom inexorably into post-op discontent. If the preoperative counseling was not performed diligently and you are faced with an unhappy patient, it is best to listen carefully, take a precise refraction and adopt a compassionate attitude. Elective surgical solutions are available but unpalatable: IOL exchange or LASIK.
Toric rotation. Like any lens, toric IOLs depend on precise alignment to work, and not only is this difficult to achieve in the operating room, but the lenses have a 3% chance of rotating during the first month. 12 Your best indicators that a rotation may have happened are significant blur and an increase in oddly oriented astigmatism. If your surgeon communicates the desired axis of the implant, you can check this by dilating and looking for the marks indicating the steep axis, but you often do not have this information. A small deviation from alignment that does not greatly affect vision is not a concern.
Any suspicion of a significant rotation should precipitate a return to the surgery center, and quickly; the best time to rotate a toric IOL back into place is within the first few weeks, before the capsule has a chance to fibrose down around the lens.
Wound leak. If the IOP is less than 8mm Hg or the anterior chamber is shallow, check for a wound leak. Often the patient will complain of significant eye ache. With fluorescein, low IOPs often manifest as waffling of the corneal surface. Instill anesthetic, then gently press a wetted strip of fluorescein around every incision. A leak will show up under cobalt blue light as a stream emerging from the incision: the positive Seidel sign.
If you discover a mild leak, place a tight bandage contact lens, stop or decrease the steroid, notify the surgeon immediately and schedule a follow up the next day. You can even prescribe a topical hypotensive such as brimonidine BID to reduce the hydraulic flow. Wound leak patients must be seen daily until resolution. Mild leaks usually seal spontaneously within a day or two, at which point you can resume the steroid.
If the leak is vigorous, the anterior chamber is so flat as to allow the iris and cornea to touch or the IOP is less than 4mm Hg, call the surgeon and send the patient back immediately; this may need a suture or anterior chamber fill.
Vitreous to the wound. If the posterior capsular tears during surgery, a strand of vitreous can stick to the surgeon’s instruments and during withdrawal be pulled out into an incision. Though invisible when fresh, eventually stray pigment granules stick to the strand, making it easier to spot. The easiest tell-tale sign, however, is a peaked pupil pointing to an incision. This incites a vigorous inflammatory response and requires a quick return to the surgeon, who will likely sever the strand with a Nd:YAG laser.
Cystoid macular edema. This presents overwhelmingly in those with a history of retinal vein occlusion, pre-existing diabetic retinopathy, macular traction from the hyaloid or from an epiretinal membrane, or a posterior capsular tear during surgery. The onset can be from weeks to months after surgery; the patient will typically report initially good vision but later blur. 13 Their macula will show a petaloid or honeycomb appearance, sometimes with appreciable elevation. Look for decreased pinhole vision, or the characteristic OCT scan.
CME tends to respond quite well to a combination of a topical steroid and NSAID at their usual dosage. These cases should be seen every two to four weeks; any case that does not improve at each visit merits consideration of a subconjunctival steroid injection or a visit to the retina specialist. If allowed to stagnate, CME can affect vision permanently.
Endophthalmitis. The most feared complication is invasion and infection of the eye by microbes. This can occur during surgery, or later if the wound is slow to heal. Any patient with some combination of significant pain, declining vision, lid edema, severe anterior chamber reaction, hypopyon and inflammatory cells in the vitreous within 72 hours after surgery should be assumed to have infectious endophthalmitis until proven otherwise. Endophthalmitis is rare—from four to 12 per 10,000 eyes in the United States. 14,15
Unfortunately, this catastrophic infection does not follow a predictable course and can present in a mild form or even much later with certain microbes. Occasionally, a smoldering uveitis or vitritis is not correctly diagnosed until months later.
You must call the surgery center immediately with any suspicious findings. The next step is often a vitreous tap and culture. The prognosis for confirmed endophthalmitis is poor, with permanently reduced vision often from 20/40 to 20/400 or worse.
Retinal detachments. Eyes without unusual risk factors seem to have no increased risk of retinal tear or detachment after cataract surgery. 16 Myopic and lattice degeneration patients, on the other hand, do have an increased risk for up to 10 years after cataract surgery. 17 You should caution at-risk patients about the usual symptoms. 17
After cataract surgery, patients often regain visual clarity that they have not enjoyed in many years. Watch out for the aforementioned signs, but, in the vast majority of cases, you will get to celebrate a safe and remarkable recovery and enjoy your patients’ satisfaction.
Dr. Kuhn-Wilken is a staff optometrist at Pacific Cataract & Laser Institute, in Tacoma, Wash.
Related Content
- Combined Surgery May Increase Endophthalmitis Risk
- One Size Won’t Fit All: Treating Ocular Infection
- Head First Into the Exam Room
- Reoperation Rates after RD Vary with Age
- A Good Catch, Myopia and Traumatic Cataracts
Current Issue
Table of Contents
Read digital edition, read pdf edition, subscriptions, related topics.
- Therapeutics

Copyright © 2024 Jobson Medical Information LLC unless otherwise noted.
All rights reserved. Reproduction in whole or in part without permission is prohibited.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
- Patient Care & Health Information
- Diseases & Conditions
To determine whether you have a cataract, your eye doctor will review your medical history and symptoms. They also will perform an eye exam. Your doctor may do several tests, including:
- Vision test. A vision test, also called a visual acuity test, uses an eye chart to measure how well you can read a series of letters. One eye is tested at a time, while the other eye is covered. A chart or a viewing device with letters that get smaller is used. With this, your eye doctor determines if you have 20/20 vision or if you have trouble seeing.
- Eye structure exam. An eye structure exam, also called a slit lamp, allows your eye doctor to see the structures at the front of your eye up close. It's called a slit lamp because it uses an intense line of light, a slit, to light up the structures in your eye. The slit allows your doctor to view these structures in small sections. This makes it easier to find anything that may be wrong.
- Retinal exam. A retinal exam looks at the back of your eyes, called the retina. To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide, called dilation. This makes it easier to see the retina. Using a slit lamp or a special device called an ophthalmoscope, your eye doctor can examine your lens for signs of a cataract.
- Fluid pressure test. This test, also called applanation tonometry, measures fluid pressure in your eye. There are multiple different devices available to do this.
When your prescription glasses can't clear your vision, the only effective treatment for cataracts is surgery.
When to consider cataract surgery
Talk with your eye doctor about whether surgery is right for you. Most eye doctors suggest considering cataract surgery when your cataracts begin to affect your quality of life. This may include your ability to perform daily activities, such as reading or driving at night.
For most people, there is no rush to remove cataracts because they usually don't harm the eyes. But cataracts can worsen faster in people with certain conditions. These include diabetes, high blood pressure or obesity.
Waiting to do cataract surgery typically won't affect how well your vision recovers. Take time to consider the benefits and risks of cataract surgery with your doctor.
If you choose not to have cataract surgery now, your eye doctor may recommend periodic follow-up exams to see if your cataracts are getting worse. How often you'll see your eye doctor depends on your situation.
What happens during cataract surgery
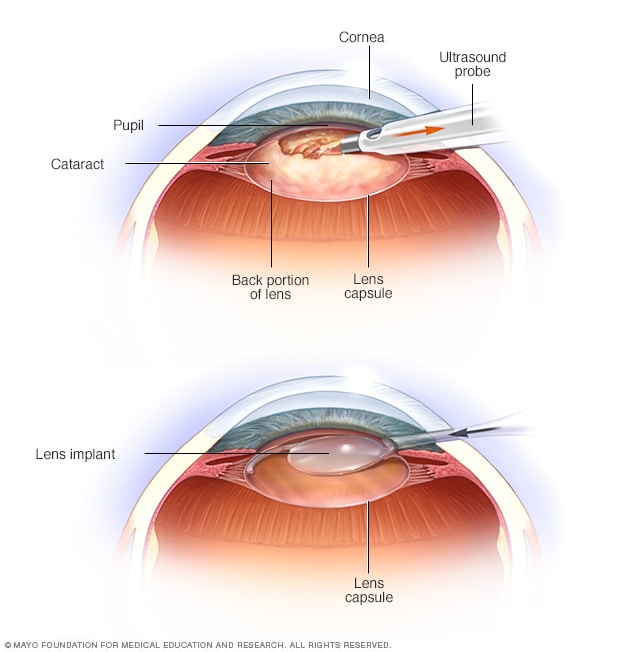
- Cataract surgery
The most common type of cataract surgery is called phacoemulsification. During this process, the rapidly vibrating tip of an ultrasound probe breaks up the cataract. Your surgeon then suctions out the lens, as seen in the top image. An outer housing of the cataract, called the lens capsule, is generally left in place. After removing the lens, your surgeon places the lens implant into the empty space within the capsule where the natural lens used to be, as seen in the bottom image.
Cataract surgery involves removing the clouded lens and replacing it with a clear artificial lens. The artificial lens, called an intraocular lens, is put in the same place as your natural lens. It remains a permanent part of your eye.
For some people, artificial lenses can't be used. In these situations, once the cataract is removed, vision may be corrected with eyeglasses or contact lenses.
Cataract surgery is typically done on an outpatient basis. This means you won't need to stay in a hospital after the surgery. During surgery, your eye doctor uses a medicine to numb the area around your eye. You usually stay awake during the procedure.
Cataract surgery is generally safe. However, it carries a risk of infection and bleeding. Cataract surgery also increases the risk of the retina being pulled out of place. This is called retinal detachment.
After the procedure, you may be sore for a few days. Healing usually happens within a few weeks.
If you need cataract surgery in both eyes, your doctor will schedule surgery to remove the cataract in the second eye after you've healed from the first surgery.
Intraocular lenses
Vivien Williams: There are some things about aging you just can't control. Take your eyesight, for example. You can fight it, but after age 40, the fine print on restaurant menus gets hard to read. And as you continue to mature, cataracts can form. But now, doctors are implanting lenses that can correct these things and even more. Here is the latest from Mayo Clinic.
Edyth Taylor is having cataract surgery. Her vision is such that it's hard for her to read the numbers on a clock.
Edyth Taylor, cataract surgery patient: I could guess. It's about five after 1:00.
Dharmendra Patel, M.D.—Mayo Clinic ophthalmology: But it's hazy?
Edyth Taylor: But it's hazy.
Dharmendra Patel, M.D.: And this is sharper?
Edyth Taylor: Oh yeah. That's as clear as can be.
Dharmendra Patel, M.D.: OK. Well, we're going to try to match it up so that your vision is equal in both eyes.
Vivien Williams: Edyth's already had one eye done. Now it's time for the other. Dr. Dharmendra Patel says the new lenses he's implanting will take care of the cloudiness caused by the cataract, plus they'll fix a whole lot more.
Dharmendra Patel, M.D.: The newer implants that are available, they do give you the multifocality. So, you will get correction for distance vision, which is similar to LASIK, but you also get the correction for near vision or reading vision, and that's something that's very unique to these implants.
Vivien Williams: Another patient, Joyce Wisby, got the new intraocular implants a few months ago.
Joyce Wisby: My coworker kept saying to me, 'You need to have this done, you can't see.'
Vivien Williams: Joyce says, after a lifetime of poor vision made worse by cataracts, she can finally see the fine print without glasses or contacts.
Joyce Wisby: If the numbers are real small, I'd have to go and ask for help or use a magnifying glass even with my glasses. Now I can read everything and everybody's coming to me and asking me to help them with the numbers.
Vivien Williams: During the procedure, Dr. Patel numbs the eye with drops. Then, through tiny incisions in the cornea, he removes the lens with the cataract. Next, he inserts the implant, which unfolds into position.
Edyth just got out of surgery.
Edyth Taylor: I can see the clock.
Vivien Williams: A 15-mininute operation for a lifetime of better vision. Dr. Patel says these lenses are most commonly used for people with cataracts, but younger people who want correction from nearsightedness could benefit too. For Medical Edge, I'm Vivien Williams.
Yes, Babies and Children Get Cataracts, Too
Hello. My name is Eric Bothun. I'm a pediatric eye surgeon at the Mayo Clinic in Rochester, Minnesota, caring for kids of all ages and eye diseases. Many times, kids simply need glasses to straighten their eyes, but others have crippling eye conditions. Some of my greatest professional joys and accomplishments have come in diagnosing, researching and treating pediatric cataracts.
Yes, babies and kids get cataracts, too — whether from complex genetic disease, a firecracker injury in an older child, or a birth defect in a newborn. Cataracts may severely cloud the vision of children. And since vision development in the brain takes years to refine, having a cataract even for a short time will have a lifelong implication.
Here at the Mayo Clinic, I seek to diagnose pediatric cataracts early — hopefully even in that newborn baby — and determine an appropriate workup and treatment plan. Caring for these kids typically involves complex cataract surgery, even for the smallest, and a team approach in rehabilitation with families for years as they grow. It all starts by first understanding and addressing a given child's unique systemic or ocular anomalies and related conditions like glaucoma. Many times, I enlist a team of specialists to aid in the various aspects of that care.
This is an example of a complex pediatric cataract surgery. The ocular features in this unilateral condition include the eye being abnormally small, having an irregular iris appearance and an often membranous-like cataract with a vessel stalk that connects that cataract to the back of the eye. One can see that stalk in this surgical video. Eyes like this often have a less favorable outcome because they hold a greater risk of glaucoma and retinal detachment. Standard intraocular lenses are typically not an option, and thus, contact lenses are often used to correct the vision postoperatively. But first and foremost is giving the child a clear view to the world.
I often compare the hazy lens to a chocolate M & M candy. And my cataract surgery involves opening that candy shell, carefully removing the chocolate and inserting a special new lens into the remaining candy shell. There, that artificial lens is meant to provide clarity for the eye and the child, lifelong.
There are unique challenges in some eyes and in some kids. I enjoy tailoring the known surgical and clinical treatment options for each kid, visit by visit, as they grow. And through research and teaching, I continue to find better ways to help these kids with cataracts.
This is an example of a fairly up-to-date approach for pediatric cataract surgery in a child between nine months and two years of age. Here, the cataract capsule is opened with a special vitrector instrument. There are a variety of techniques, depending on the anatomy and age of the child, to do this. The lens contents, which can vary in density and opacity, is completely removed. And this leaves that natural capsular bag in place behind the iris for the insertion of the artificial lens and long-term stabilization.
Some eyes simply cannot hold a standard lens in the typical location. I have been involved in studying a newer lens design that simply clips the artificial lens to the front side of the iris. This approach is only suitable for certain eyes but has become a valuable tool for visually rehabilitating special patients.
Through my service and the coordinated care at the Mayo Clinic, we deliver quality outcomes for pediatric cataracts. The before and after photos are dramatic. But the real positive emotion and the real blessing is in watching the eyes recover and the vision improve as kids grow up into fuller lives. If you know someone who has a pediatric cataract — or condition even that puts them at risk of one — please come to our team at the Mayo Clinic.
More Information
Clinical trials.
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
To deal with symptoms of cataracts until you decide to have surgery, try to:
- Make sure your prescription for your eyeglasses or contact lenses is up to date.
- Use a magnifying glass to read if you need more help reading.
- Improve the lighting in your home with more or brighter lamps.
- Wear sunglasses or a broad-brimmed hat to reduce glare during the day.
- Limit driving at night.
Self-care measures may help for a while, but your vision may get worse as the cataract grows. When vision loss starts to affect your everyday activities, consider cataract surgery.
Preparing for your appointment
Make an appointment with your usual eye care professional if you notice changes in your vision. If they determine that you have cataracts, then you may be referred to an eye specialist who can perform cataract surgery.
There's often a lot to talk about. It's a good idea to be well prepared for your appointment so that you can make the most of your time. Here's some information to help you get ready.
What you can do
- List any symptoms you're experiencing, including any that may not seem related to the reason you scheduled the appointment.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Take a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- List questions to ask your health care team.
For cataracts, some basic questions to ask include:
- Are cataracts causing my vision problems?
- What kinds of tests do I need?
- Will cataract surgery correct my vision problems?
- What are the potential risks of cataract surgery? Are there risks in waiting to do surgery?
- What will cataract surgery cost, and will my insurance cover it?
- How much time will I need to recover from cataract surgery?
- Will any usual activities be restricted after cataract surgery? For how long?
- After cataract surgery, how long should I wait before getting new glasses?
- If I use Medicare, will it cover the cost of cataract surgery? Does Medicare cover the cost of new glasses after surgery?
- If I don't want surgery right now, what else can I do to help with my vision changes?
- How will I know if my cataracts are getting worse?
- I have these other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask questions at any time if you don't understand something.
What to expect from your doctor
Your health care team is likely to ask you a number of questions. Being ready to answer them may allow more time later to cover other points you want to address. You may be asked:
- When did you begin having symptoms?
- Do you have your symptoms all the time or do they come and go?
- Do you have vision problems in bright light?
- Have your symptoms gotten worse?
- Do your vision problems make it difficult for you to drive?
- Do your vision problems make it difficult to read?
- Do your vision problems make it difficult to do your job?
- Have you ever had an eye injury or eye surgery?
- Have you ever been diagnosed with an eye problem, such as inflammation of your iris?
- Have you ever received radiation therapy to your head or neck?
- Cataract. Merck Manual Professional Version. https://www.merckmanuals.com/professional/eye-disorders/cataract/cataract?query=cataract#. Accessed April 17, 2023.
- AskMayoExpert. Cataracts. Mayo Clinic; 2022.
- Cataract. American Optometric Association. https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/cataract?sso=y. Accessed April 17, 2023.
- Jacobs DS. Cataract in adults. https://www.uptodate.com/contents/search. Accessed April 19, 2023.
- Cataracts. National Eye Institute. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts. Accessed April 19, 2023.
- Cataract in the adult eye PPP. American Academy of Ophthalmology. https://www.aao.org/education/preferred-practice-pattern/cataract-in-adult-eye-ppp-2021-in-press. Accessed April 19, 2023.
- Causes of cataracts. National Eye Institute. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts/causes-cataracts. Accessed April 19, 2023.
- How a cataract affects your vision
- What a cataract looks like
Associated Procedures
Products & services.
- A Book: Mayo Clinic Guide to Better Vision
- A Book: Mayo Clinic on Healthy Aging
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
By Catlin Nalley, Contributing Editor
Maximizing Vision After Cataract Surgery
Most surgeries are successful, but there are some patients who aren’t happy with their vision for no obvious reason, and surgeons have to delve deeper..
W ith more than three million Americans undergoing cataract surgery each year, it is one of the most common—and safest—procedures performed in the United States. And ongoing advancements in surgical techniques and intraocular lens technology support the efforts of ophthalmologists who continuously strive to ensure their patients have the best possible visual outcomes.
Maximizing outcomes depends on a number of factors and doesn’t end with the removal of the cataract and the implantation of an IOL. “The key aspects of patient satisfaction after cataract surgery today include a meticulous preoperative evaluation, judicious patient selection and a comprehensive patient education to set the appropriate postoperative expectations,” says Garden City, New York’s Eric Donnenfeld, MD, while noting that postoperative management also plays a crucial role in successful cataract surgery outcomes, and part of that is addressing patient concerns and complaints.
However, what do you do if you have run the appropriate tests and everything (i.e., the macula, IOL, cornea) looks normal yet the patient is still having an issue with their vision? In this article, we’ll explore various strategies to maximize vision after cataract surgery and IOL implantation as well as how to help their patients navigate the process.
Clinical Pearls for Surgeons
When the standard exams all come back normal, taking a step back and carefully considering how best to proceed can help ophthalmologists uncover the underlying issue and appropriate intervention. Below ophthalmologists offer advice on how they approach these cases.
If a patient isn’t satisfied with their visual outcome post-surgery, Daniel Chang, MD, of Empire & Laser in Bakersfield, California, begins by making sure he has a clear understanding of the issue. Is it quality of vision? Range of vision? Dysphotopsia?
To determine next steps, it’s important to get as much detail from the patients as possible. Dr. Chang will often ask questions like, “What specific thing are you doing and when does it specifically bother you?” This allows you to get a detailed picture of the problem and from there you can figure out the cause and best treatment approach.
Don’t overlook dry eye, advises Dr. Donnenfeld. “Even if the patient’s cornea looks normal, very commonly you will find irregularities that explain the vision, and I look for a history of visual fluctuation. Any time the vision fluctuates, I consider ocular surface disease,” he explains. “In addition to a visual inspection of the ocular surface, I add lissamine green to highlight any staining irregularities in the conjunctiva and provide a more in-depth evaluation of the ocular surface.”
Additionally, Dr. Donnenfeld will use topography to find slight irregularities that may be compromising a patient’s vision. “When I see these problems, I will often take a more aggressive approach to manage the ocular surface.” This includes perfluorohexyloctane (Meibo), which he has found stabilizes the surface and is a good refractive solution. Punctal plugs can also have a role as well as some low-dose steroids, he notes. “Even the mildest tear film abnormalities, which can be very easily missed, can cause significant patient dissatisfaction.”
Wills Eye’s Beeran Meghpara, MD, reiterated the value of a corneal topography for these cases. “It’s very easy to miss subtle changes, especially if you’re a doctor who doesn’t specialize in the cornea. Therefore, I always perform a corneal topography on these patients, which can help pick up issues such as subtle epithelial basement membrane dystrophy that you may not be able to see or subtle areas of irregular astigmatism,” he says, noting the importance of looking at the Placido ring image when using this tool.
Dr. Meghpara will also get an OCT of the macula when trying to determine the reason behind a patient’s vision complaints. “Even if the retina appears normal, there are some changes, such as a subtle epiretinal membrane, that you can’t see when using a slit lamp,” he explains.
A very commonly overlooked problem, according to Dr. Donnenfeld, is one that wasn’t always on his checklist either. “In the past I didn’t always include the vitreous in my standard workup, but what we’re seeing now is that a lot of patients, particularly those with multifocal lenses, who have even mild vitreous opacification can have significant loss of quality of vision,” he says, while emphasizing the need for a dilated eye exam.
“Vitreous floaters are an often underdiagnosed reason for patient dissatisfaction after multifocal IOL surgery,” adds Dr. Meghpara. “In our practice, we’ll refer patients to a retinal surgeon for vitrectomy. Afterwards, patients are very grateful and happy with the results. Some ophthalmologists may opt to address floaters with an office-based approach, such as a YAG laser.”
When addressing visual concerns post-surgery, Dr. Meghpara suggests tools like iTrace can be helpful. “This diagnostic tool performs both corneal topography and wavefront aberrometry,” he says. “If you conduct this test on a patient after cataract surgery, the image quality should be excellent (9 or 10 on a scale of 10). However, if that image quality is low, say a 5 or 6, but everything looks crystal clear then you are missing something. Oftentimes, that is the vitreous.”
Another easily missed abnormality, notes Dr. Donnenfeld, is related to the angle kappa—the angle between the pupillary axis and the visual axis. “When the pupils aren’t coincident with the central lens that will induce coma, glare and some halo as well.”
In those cases, when other options have been exhausted, Dr. Donnenfeld will perform an argon-laser iridoplasty. “I can actually put laser spots onto the iris and pull the pupil over the center of the lens to make the lens more productive. Using a 500-milliwatt, 500 microsecond and 500 millijoule procedure, I place four or five spots in the area of the iris where I want to move the pupil. So, if the pupil is decentered temporally, I place the spots nasally and you can move the pupil very effectively into the area.”
Refraction is another key component, notes Richard Davidson, MD, of Aurora, Colorado. “Our team will always conduct a thorough eye exam. This includes visual acuity and refraction. We will refract every one of these patients and really try to nail down a good refraction because even if someone is ‘20/20,’ they still may have a little residual astigmatism, for instance, and that may be enough to bother them.”
Another consideration for surgeons is when additional procedures, such as a YAG laser capsulotomy or PRK enhancement, are warranted. For example, Dr. Davidson recently saw a patient who was one-week postop in her right eye and three-weeks postop in her left eye. She has multifocal lenses and was happy with the vision in her right eye but was complaining of blurriness in her left.
“Based on our discussion, this was not a lens adaptation issue,” he says. “We refracted the left eye and even with refraction the vision quality wasn’t as good as she wants it to be.
“I know she doesn’t have any macular edema,” he continues. “So, I looked at her capsule and she’s got a little wrinkling. It’s not a lot but enough that it can drop her vision enough, especially compared to the other eye. Therefore, I recommended a YAG laser capsulotomy. We know that with patients who have multifocal lenses there’s going to be a lower threshold to do a YAG compared to someone with a monofocal lens.”
Dr. Davidson notes that it can be challenging to determine if, and when, these types of interventions are necessary. This is particularly true when they have only had surgery in the first eye. Are they unhappy with the lens? Are they unhappy because they have a cataract in the other eye? Are they unhappy because they have posterior capsule opacification and need a YAG?
“This is always one of the surgeon’s most frustrating and challenging dilemmas,” says Dr. Davidson, while adding that there is no one-size-fits-all approach. “It really comes down to a variety of factors, including how the patient did immediately postop, how bad the cataract is in the other eye, do they have a lot of anisometropia, etc. If the patient is happy with the type of lens and I’ve done everything else, I’d consider a YAG capsulotomy.”
When it comes to PRK enhancement, Dr. Davidson waits a minimum of six weeks before considering it. “I want to see how they’re functioning as well as make sure that the lens has settled in and that they have consistent refractive error,” he explains. “If we’re going to move forward to a PRK enhancement, I want to have a complete picture to ensure we’re providing our patients with the approach that best fits their individual needs.”
Determining if a lens exchange is the best option is also on the table, surgeon say. “There can be a temptation to just do a treatment, such as a YAG laser capsulotomy when the capsule is actually quite clear, because a lens exchange is a much more involved procedure. However, there are times when it may be necessary,” says Dr. Chang.
If you’ve done everything you can—and ruled out other issues—and the patient just isn’t happy, for whatever reason, with the lens, Dr. Meghpara suggests discussing a lens exchange. “Sometimes you just have to bite the bullet and acknowledge that this lens is not perfect,” he says. “While, for instance, multifocals work well for the majority of patients, in some patients they’re just not well-tolerated.”
This holds true for monofocal lenses as well, he notes. “Perhaps your patient is experiencing dysphotopsia such as shadows, streaks and starbursts and you’ve done everything you can to address the problem. This is another situation that could be attributed to the lens and, while uncommon, this can happen with an IOL placement.”
In these cases, Dr. Meghpara would offer a lens exchange as long as their symptoms and dissatisfaction can clearly be attributed to the lens. “On the other hand, if you can’t explain their symptoms and their unhappiness by the lens, we won’t simply do a lens change and hope that it’ll improve a patient’s vision because there are risks associated with that procedure.”
Expectations & Education
Beyond taking the appropriate clinical action, success also depends on how you approach your patient and respond to their concerns. “Don’t dismiss their complaints,” urges Dr. Davidson. “Try not to get defensive or frustrated. I always do my best to reassure patients and validate their concerns, letting them know that I am there to help and will do everything I can to address the problem.”
Fostering understanding and cooperation with your patients depends—in large part—on education and expectation management. Ophthalmologists must communicate openly with their patients during the entire cataract surgery process from the first preoperative appointment throughout the postoperative stage.
“Setting expectations in advance is critical,” says Dr. Meghpara, who encourages his patients to have someone with them during the evaluation and also sends them home with a written record of the key discussion points. “Help your patients understand what’s realistic and what isn’t. I also avoid absolutes such as ‘you’ll never have to wear glasses again.’ ”
“It’s important to remember that, in addition to the technical and clinical aspects of cataract surgery, there’s a personality and expectation component that must be managed as well,” Dr. Chang concludes. “We have to be prepared to problem solve and manage any challenges that arise to achieve the best possible visual outcomes for our patients.”
Dr. Chang consults for Johnson & Johnson Vision and Carl Zeiss. Dr. Davidson consults for Zeiss, Johnson & Johnson Vision, Alcon and Centricity Vision. Dr. Donnenfeld consults for Allergan, Alcon, Bausch & Lomb and Johnson & Johnson Vision. Dr. Meghpara reports no relevant disclosures.
Related Articles

How to Manage Postop Inflammation
More than one way to crack a nucleus.
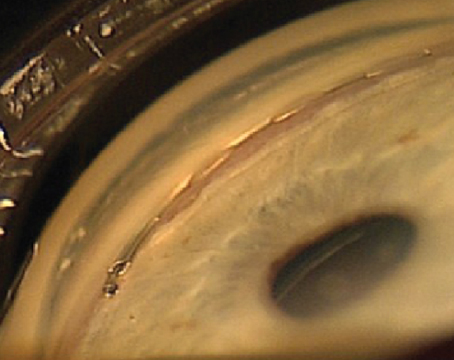
IOLs & Cataract Surgery in Glaucoma Patients
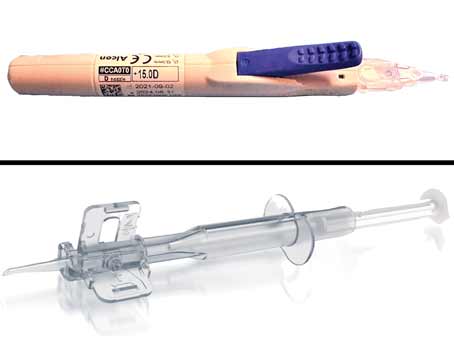
A Look at the Latest Pre-loaded IOL Injectors
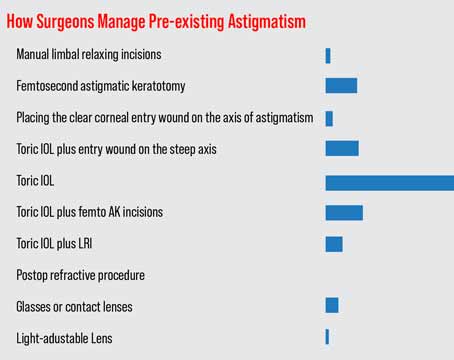
Survey: Cataract Surgery Snapshot
Current issue.

Table of Contents
Read digital edition, read pdf edition, subscriptions.

Copyright © 2024 Jobson Medical Information LLC unless otherwise noted.
All rights reserved. Reproduction in whole or in part without permission is prohibited.

A weekend getaway in Northern PA

Annual All Star Labor Classic is 4/14

Take a road trip to Harford County, MD

Natural ways to lower blood pressure

- Health News
- Children's Health
Entertainment
- Food & Drink
- Restaurants
- Family-Friendly
- Performances
- Fantasy Football
- Staff / Contributors
- Legal / Privacy
© 2024 WWB Holdings, LLC. All rights reserved
- Google Plus
More Health:
- Healthy Eating
- Mental Health
April 05, 2024
Are you one of the millions about to have cataract surgery? Here’s what you need to know
The procedure is among the most common in the world. serious complications are rare, and patients typically go home right away..
Cataract surgery is one of the most commonly performed procedures in the world. Above, Dr. Douglas Kohl of Eye Associates of Boca Raton in Florida looks through an opthalmic microscope before performing cataract surgery on a sedated patient in one of the clinic's operating rooms on Monday, Dec. 19, 2022
Cataract surgery is one of the most popular and commonly performed procedures in the world. The vast majority of patients have excellent outcomes with few complications.
• By age 80, over half of all Americans have cataracts . • Close to 4 million cataract surgeries are performed in the U.S. every year . • Over 90% of patients have 20/20 vision with glasses after surgery , although those with other eye conditions may not do as well, including those with glaucoma , a progressive disease typically associated with elevated pressure within the eye; diabetic retinopathy , which ultimately can cause leakage in the retinal tissues; and macular degeneration , a disease that is typically related to age. • The rate of post-surgery infection from endophthalmitis is less than 0.1%.
As ophthalmologists who have performed thousands of these procedures , we know that many patients have misconceptions about both cataracts and the surgery. For example, some think a cataract is a growth on the eye’s surface.
We like to compare a cataract with the frosted glass of a bathroom window, where light can be transmitted but details cannot. Or when turbulence from a storm causes normally clear water in the ocean to become murky. In much the same way, the eye’s once transparent lens becomes cloudy.
About the surgery
Cataract surgery removes the clouded lens of the eye and replaces it with a new, clear lens to restore your vision. Most patients report the procedure is painless.
It’s typically an elective surgery that is performed on an outpatient basis. The patient is often awake, under local anesthesia, with sedation similar to that used for dental procedures. We like to say patients receive the equivalent of three margaritas in their IV.
Numbing drops are then applied to the eye’s surface, along with an anesthetic inside the eye. Patients with claustrophobia, or movement disorders such as Parkinson’s disease, may not be suitable candidates for awake surgeries and require general anesthesia.
Before surgery, patients receive dilating drops to make the pupil as large as possible. The surgeon makes a tiny incision, usually with a small pointed scalpel, between the clear and white part of the eye to gain access to the lens capsule , a thin membrane similar in thickness to a plastic produce bag at the grocery store.
This capsule is suspended by small fibers called zonules , which are arranged like the springs that suspend a trampoline from a frame. The surgeon then creates a small opening in the capsule, called a capsulotomy, to gain access to the cataract. The cataract is then broken into smaller parts so they are removable through the small incision.
This is similar to a tiny jackhammer, breaking the large lens into smaller pieces for removal. That sounds scary, but it’s painless. Ultrasound emulsifies the lens and vacuum power then aspirates it from the eye.
Laser-assisted cataract surgery has been found to have similar outcomes to traditional cataract surgery.
Complications are rare
Serious complications, such as postoperative infection, bleeding in the eye or a postoperative retinal detachment are rare; they occur in approximately 1 in 1,000 cases. But even in many of these situations, appropriate management can salvage useful vision .
Capsular complications deserve additional discussion. According to some studies, they occur in up to 2% of cases . If a hole or tear of the posterior capsule is encountered during cataract surgery, the clear gel in the vitreous – the back chamber of the eye – may be displaced into the front chamber of the eye.
If that happens, the gel must be removed at the time of the cataract surgery. This will reduce the likelihood of additional postoperative complications, but those who have the procedure, known as a vitrectomy , have an increased risk for additional complications, including postoperative infections and postoperative swelling.
After the surgery
Patients usually go home right after the procedure. Most surgery centers require that the patient have someone drive them home, more for the anesthesia rather than the surgery. Patients begin applying postoperative drops that same day and must wear an eye shield at bedtime for a few weeks after surgery.
Patients should keep the eye clean and avoid exposure to dust, debris and water. They should try not to bend over and should avoid heavy lifting or straining in the first week or so after surgery. Lifting or straining can cause a surge of blood pressure to the face and eye. Known as a choroidal hemorrhage , it can lead to bleeding into the wall of the eye and be devastating to vision.
Things that cause only moderate increases in heart rate such as walking are OK. Routine postoperative examinations are usually completed the day after surgery, about a week after surgery and about a month after surgery.
A choice of lens
The plastic lens used to replace the cataract, or intraocular lens , requires careful sizing for optimal results and a nuanced discussion between patient and surgeon.
Early intraocular lens technologies were monofocal , and most patients with these lenses chose distance correction and used reading glasses for near tasks. This is still the preferred approach for approximately 90% of patients having cataract surgery today.
Recent advances have led to intraocular lenses that offer multifocality – the opportunity to have near as well as distance vision, without glasses. Some multifocal lenses are even in the trifocal category, which includes distance, near, and intermediate vision, the latter of which in recent years has become very important for computer and phone use.
Most patients with these advanced technology multifocal lenses are happy with them . However, a small percentage of patients with multifocal lenses can be so bothered by visual disturbances – notably night glare and halos around light sources in the dark – that they request removal of the multifocal lens to exchange it for a standard intraocular lens. These exchanges are a reasonable option for such situations and offer relief for most affected patients.
Determining who’s an ideal candidate for a multifocal intraocular lens is an area of active research. Most clinicians would recommend against such a lens for a patient with a detail-oriented personality. Such patients tend to fixate on the shortcomings of these lenses despite their potential advantages.
As with many technologies, current generation advanced technology intraocular lenses are much better than their predecessors. Future offerings are likely to offer improved vision and fewer side effects than those available today.
But these newer lenses are often not reimbursed by insurance companies and often entail substantial out-of-pocket costs for patients.
Allan Steigleman , Associate Professor of Ophthalmology, University of Florida and Elizabeth M. Hofmeister , Associate Professor of Surgery, Uniformed Services University of the Health Sciences
This article is republished from The Conversation under a Creative Commons license. Read the original article .
Allan Steigleman, University of Florida and Elizabeth M. Hofmeister, Uniformed Services University of the Health Sciences
Health Videos

A parent’s guide to poison prevention at home

From fidgeting to focus: Sensory toys help kids and adults
Just in.
- 4.8-magnitude earthquake rattles Philly and surrounding region
- Northbound section of I-95 in Port Richmond to remain closed into weekend
- WATCH: The Rock arrives to Philly, trash talks Eagles ahead of WrestleMania 40
- Philly bans license plate flippers, which allow drivers to evade tolls, parking tickets and police
- Theater, street cleanups and WrestleMania: Your weekend guide to things to do
- Jersey Shore beach sweeps cleared 176,000 pieces of trash last year — including weird stuff
Running won't help when you're mad, but it offers many psychological benefits
- Temple eye doctor explains the dangers of looking at the sun during an eclipse
- How often should you replace your kitchen sponge? Probably more often than you do
- Lack of sleep could increase risk of high blood pressure, study says
- Later bedtimes, irregular sleep habits linked to lower grades for high school students, study finds
- Vaping increases risk of heart failure by nearly 20%, study suggests
Must Read
Aramark stadium workers gain city council support as strike looms.

Men's Health

A theater company known for D&D improv finds a permanent home

Phillies to unveil City Connect uniforms this week

Kensington Derby and Arts Festival moving race to Frankford Avenue

- About PhillyVoice.com
- About aHealthierPhilly
The contents of this website, such as text, graphics, images, and other material contained on this website, are for informational purposes only and do not constitute medical advice.
a healthier philly is sponsored by Independence Blue Cross, the leading health insurance organization in Southeastern Pennsylvania, serving nearly 2.5 million people in the region, providing health news and related information that leads to a more informed, healthier life.
a healthier philly and its health-related information resources are not a substitute for the medical advice, diagnosis, and treatment that patients receive from their physicians or health care providers and are not meant to be the practice of medicine, the practice of nursing, or to carry out any professional health care advice or service in the state where you live. Nothing in this website is meant to be used for medical or nursing diagnosis or professional treatment.
Always seek the advice of your physician or other licensed health care provider. Always consult your health care provider before beginning any new treatment, or if you have any questions regarding your health condition. You should not disregard medical advice, or delay seeking medical advice, because of something you read on this site. In the event of a medical emergency, call a doctor or 911 immediately.
This website does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on this website. Descriptions of, references to, or links to other products, publications, or services does not imply endorsement of any kind. Reliance on any information provided by this website is solely at your own risk.
Although we try to keep the information on the site as accurate as possible, a healthier philly disclaims any warranty concerning its accuracy, timeliness and completeness of content, and any other warranty, express or implied, including warranties of merchantability or fitness for a particular purpose. a healthier philly also reserves the right to temporarily or permanently discontinue this website, any page or any functionality at any time and without any notice.
The website and its content are provided on an “as is” basis.
- The Magazine
- Stay Curious
- The Sciences
- Environment
- Planet Earth
What You Need To Know Before Cataract Surgery
Cataract surgery removes the clouded lens of the eye and replaces it with a new, clear lens.

Cataract surgery is one of the most popular and commonly performed procedures in the world. The vast majority of patients have excellent outcomes with few complications.
Here are the numbers:
By age 80, over half of all Americans have cataracts .
Close to 4 million cataract surgeries are performed in the U.S. every year .
Over 90% of patients have 20/20 vision with glasses after surgery , although those with other eye conditions may not do as well, including those with glaucoma , a progressive disease typically associated with elevated pressure within the eye; diabetic retinopathy , which ultimately can cause leakage in the retinal tissues; and macular degeneration , a disease that is typically related to age.
The rate of post-surgery infection from endophthalmitis is less than 0.1%.
As ophthalmologists who have performed thousands of these procedures , we know that many patients have misconceptions about both cataracts and the surgery. For example, some think a cataract is a growth on the eye’s surface.
We like to compare a cataract with the frosted glass of a bathroom window, where light can be transmitted but details cannot. Or when turbulence from a storm causes normally clear water in the ocean to become murky. In much the same way, the eye’s once transparent lens becomes cloudy.
After surgery, there’s no bending, inversions, lifting or straining, high-impact activities or eye makeup for one to two weeks or until the doctor says it’s OK.
About the Surgery
Cataract surgery removes the clouded lens of the eye and replaces it with a new, clear lens to restore your vision. Most patients report the procedure is painless.
It’s typically an elective surgery that is performed on an outpatient basis. The patient is often awake, under local anesthesia, with sedation similar to that used for dental procedures. We like to say patients receive the equivalent of three margaritas in their IV.
Numbing drops are then applied to the eye’s surface, along with an anesthetic inside the eye. Patients with claustrophobia, or movement disorders such as Parkinson’s disease, may not be suitable candidates for awake surgeries and require general anesthesia.
Before surgery, patients receive dilating drops to make the pupil as large as possible. The surgeon makes a tiny incision, usually with a small pointed scalpel, between the clear and white part of the eye to gain access to the lens capsule , a thin membrane similar in thickness to a plastic produce bag at the grocery store.
This capsule is suspended by small fibers called zonules , which are arranged like the springs that suspend a trampoline from a frame. The surgeon then creates a small opening in the capsule, called a capsulotomy, to gain access to the cataract. The cataract is then broken into smaller parts so they are removable through the small incision.
This is similar to a tiny jackhammer, breaking the large lens into smaller pieces for removal. That sounds scary, but it’s painless. Ultrasound emulsifies the lens and vacuum power then aspirates it from the eye.
Laser-assisted cataract surgery has been found to have similar outcomes to traditional cataract surgery.
Complications are Rare
Serious complications, such as postoperative infection, bleeding in the eye or a postoperative retinal detachment are rare; they occur in approximately 1 in 1,000 cases. But even in many of these situations, appropriate management can salvage useful vision .
Capsular complications deserve additional discussion. According to some studies, they occur in up to 2% of cases . If a hole or tear of the posterior capsule is encountered during cataract surgery, the clear gel in the vitreous – the back chamber of the eye – may be displaced into the front chamber of the eye.
If that happens, the gel must be removed at the time of the cataract surgery. This will reduce the likelihood of additional postoperative complications, but those who have the procedure, known as a vitrectomy , have an increased risk for additional complications, including postoperative infections and postoperative swelling.
After the Surgery
Patients usually go home right after the procedure. Most surgery centers require that the patient have someone drive them home, more for the anesthesia rather than the surgery. Patients begin applying postoperative drops that same day and must wear an eye shield at bedtime for a few weeks after surgery.
Patients should keep the eye clean and avoid exposure to dust, debris and water. They should try not to bend over and should avoid heavy lifting or straining in the first week or so after surgery. Lifting or straining can cause a surge of blood pressure to the face and eye. Known as a choroidal hemorrhage , it can lead to bleeding into the wall of the eye and be devastating to vision.
Things that cause only moderate increases in heart rate such as walking are OK. Routine postoperative examinations are usually completed the day after surgery, about a week after surgery and about a month after surgery.
Light and UV exposure, coupled with time, causes the lens of the eye to become increasingly cloudy.
A Choice of Lens
The plastic lens used to replace the cataract, or intraocular lens , requires careful sizing for optimal results and a nuanced discussion between patient and surgeon.
Early intraocular lens technologies were monofocal , and most patients with these lenses chose distance correction and used reading glasses for near tasks. This is still the preferred approach for approximately 90% of patients having cataract surgery today.
Recent advances have led to intraocular lenses that offer multifocality – the opportunity to have near as well as distance vision, without glasses. Some multifocal lenses are even in the trifocal category, which includes distance, near, and intermediate vision, the latter of which in recent years has become very important for computer and phone use.
Most patients with these advanced technology multifocal lenses are happy with them . However, a small percentage of patients with multifocal lenses can be so bothered by visual disturbances – notably night glare and halos around light sources in the dark – that they request removal of the multifocal lens to exchange it for a standard intraocular lens. These exchanges are a reasonable option for such situations and offer relief for most affected patients.
Determining who’s an ideal candidate for a multifocal intraocular lens is an area of active research. Most clinicians would recommend against such a lens for a patient with a detail-oriented personality. Such patients tend to fixate on the shortcomings of these lenses despite their potential advantages.
As with many technologies, current generation advanced technology intraocular lenses are much better than their predecessors. Future offerings are likely to offer improved vision and fewer side effects than those available today.
But these newer lenses are often not reimbursed by insurance companies and often entail substantial out-of-pocket costs for patients.
Deciding on what type of lens is best for you can be complicated. Fortunately, except in unusual circumstances, such as when a cataract develops after trauma to the eye, there is seldom a hurry for adult cataract surgery.
Allan Steigleman is an Associate Professor of Ophthalmology at the University of Florida. Elizabeth M. Hofmeister is an Associate Professor of Surgery at the Uniformed Services University of the Health Sciences. This article is republished from The Conversation under a Creative Commons license . Read the original article .
Already a subscriber?
Register or Log In

Keep reading for as low as $1.99!
Sign up for our weekly science updates.
Save up to 40% off the cover price when you subscribe to Discover magazine.
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
The State of Bilateral Cataracts
By: Joe Paone | Senior Editor
Published: 4/1/2024
Poor reimbursement and hesitancy among surgeons continue to hamper broad adoption of same-day surgeries on both eyes, but this practice lauds the efficiency, outcomes and financial sustainability.
M ost cataract patients suffer the condition in both eyes. So why not perform cataract surgery on both eyes on the same day? Well, for many surgeons and facilities… it’s complicated.
Unpacking obstacles
The first obstacle: Medicare and private insurers continue to decline paying (or paying enough) for the second eye. That means the financials don’t add up for most eye facilities. The second rests with the majority of eye surgeons who either fear patients contracting infections in (and potentially losing sight in) both eyes, or who simply prefer to continue the tried-and-true cadence of operating on one eye on a given day, then operating on the other a few days or weeks later. If you’re running a safe, profitable, high-volume cataract line with positive patient outcomes, the thinking goes, why mess with success?
After well over a decade in practice, bilateral same-day cataract surgery still faces a steep uphill climb to widespread adoption. For the select few that have restructured their practices to fully embrace the bilateral concept, however, the benefits in terms of both the patient experience and the bottom line have made their outlier status rewarding. We recently spoke with a South Florida facility that does almost nothing but bilateral same-day cataract surgeries. Its story illustrates the conditions needed to succeed with this enticing but rare subspecialty.
‘It’s all we do’
The winning formula for providing bilateral same-day cataract surgeries at SightTrust Eye Institute in Sunrise, Fla., incorporates a specialized workflow, implantations of premium intraocular lenses (IOLs), patients who don’t rely on private insurance or Medicare for payment, and a dedicated surgeon and facility that maintains an unblemished infection prevention strategy.
SightTrust’s setup developed quickly and has purred like a kitten for about a decade, says Victoria Wiltshire, MBA, RN, vice president and chief operating officer, who estimates at least 95% of the cataract surgeries performed at SightTrust are bilateral same-day procedures. “There’s rarely a time we’ll do a single eye unless the patient had an eye done somewhere else, or has a Grade III or denser cataract,” she says.
A decade ago, SightTrust performed cataract surgeries like most every other facility. “It was, ‘You’ll be back for the second eye in one week, two weeks,’” says Ms. Wiltshire, who noticed many patients got confused by the different drop schedules for each eye.
SightTrust Medical Director and CEO Andrew Shatz, MD, spent two years researching the safety and efficacy of bilateral same-day cataract surgeries. Ultimately comfortable with what he learned, he began performing them at SightTrust, and the surgeries soon dominated the practice. “I went off the beaten path,” says Dr. Shatz. “There aren’t too many people, even my fellow residents, who would even consider doing this kind of thing.”
“Suddenly 25% of our caseload was bilateral, then 50%, then 75%,” says Ms. Wiltshire. “We got to 100% quickly. We didn’t get a lot of pushback from patients when we’d say, ‘Hey, you can have both eyes done on the same day.’ They were like, ‘Great, how quickly can I sign up?’”
Go with the flow
The procedural quirk — and infection prevention requirement — of bilateral same-day cataract surgery is that each eye must be treated as a completely separate surgery. SightTrust’s two-OR facility and workflow is designed specifically to make the “dual surgery” system as routine and efficient as possible.
Suddenly 25% of our caseload was bilateral, then 50%, then 75%. We got to 100% quickly. Victoria Wiltshire, MBA, RN
When a patient arrives, they’re immediately taken to prep. They sit in a stretcher chair and dilate for about 30 minutes. They meet the anesthesiologist, who provides very mild IV sedation with midazolam, which makes the patient calm and comfortable but also responsive and coherent throughout the procedure, while ensuring they can quickly talk and walk postoperatively. At this stage, Dr. Shatz says hello to the patient.
Once dilated and sedated, the patient is wheeled to the first OR, which houses a femtosecond laser. Dr. Shatz makes the necessary incisions, corrects any astigmatism and creates a checkerboard laser pattern that breaks up the cataracts and allows them to be extracted as small cubes. Ms. Wiltshire says this process takes five to seven minutes per eye. The laser OR is a “clean technique” room, not a sterile OR, she notes.
The patient is then wheeled to the sterile second OR, where phacoemulsification and IOL implantation is performed on the first eye. That takes 10 to 15 minutes. Then the room is completely sterilized around the patient. “Dr. Shatz ungowns and leaves the room, and we turn the room over,” says Ms. Wiltshire. “The OR is fully wiped down, new instrument trays are brought in, and we set everything up again. The patient is re-sterilized and re-draped, and the entire process is started over again.” The turnover takes about seven minutes. Dr. Shatz then returns, freshly gowned and scrubbed, and operates on the second eye.
The patient is then wheeled to recovery, which takes about 15 minutes. “Patients are here for an hour-and-a-half to two hours total,” says Ms. Wiltshire, who notes this process is repeated over and over each day of surgery.
Once patients are home, Dr. Shatz says there’s really no difference from traditional cataract surgery in terms of recovery, except the postoperative drop regimen is easier. “They’re putting the same number of drops at the same frequency in both eyes at the same time,” he says. “It’s really confusing for a patient if they wait weeks between eye one and eye two. As they’re tapering the medication, one eye needs less drops than the other. With bilateral same-day cataract surgery, they don’t need to think about that.”
Dr. Shatz doesn’t call the procedure “bilateral same-day cataract surgery” when explaining it to patients. “We tell them we’re going to take care of both eyes on the same day,” says Dr. Shatz. “But I always stress that it’s two eye surgeries done on the same day, that we’re not operating on both eyes together.”
Overcoming obstacles

Fear of patients developing devastating infections like endophthalmitis or toxic anterior shock syndrome in both eyes is minimal at SightTrust, because among the thousands of bilateral same-day cataract surgeries performed there over the last decade, there has never been a bilateral infection. “Not a single one,” says Ms. Wiltshire. “We run a tight ship. It’s as if the patient physically left here between eyes and came back on a different day. The sterile technique is the same. Every standard of care is upheld in that moment.”
“I’m always concerned about risk of infection, but the fact of the matter is, studies have shown the safety of bilateral same-day surgery,” says Dr. Shatz. “I think that’s because most of us doctors who perform bilateral same-day surgery are that much more cautious that everything is done perfectly. We’re a lot more fastidious about making sure everything is sterilized properly, cleaned properly, that we’re not using the same equipment each time. We don’t cut any corners.”
In terms of qualifying patients, Dr. Shatz calls on his experience. “I think there are more people who it’s better to do it on than not,” he says. “For instance, you’d think an elderly person shouldn’t do this, but if you want to save them from a second anesthesia session, it’s a good idea. Where I may hold off doing two eyes on the same day is with people who have very dense cataracts that take longer to heal. They may be better off having one eye helping them while the other heals.”
Clinically, then, bilateral same-day surgeries appear to be safe, and deliver positive outcomes. The true obstacles to widespread adoption are financial and operational.
Making it work
SightTrust dropped out of Medicare last year because CMS doesn’t pay enough for the second eye, and has largely eschewed reluctant private payors as well in favor of a cash-pay model. Asked whether CMS and other payors are coming around to bilateral same-day cataracts, Ms. Wiltshire has moved on. “We don’t try to lobby or stay up to date with reimbursement,” she says. “We gave it a good shot to try to make it work. Ultimately, the technology has advanced, our business model has advanced, and insurance hasn’t really kept up with the times. To delay a procedure just for reimbursement didn’t make sense to us.”
Bolstering this model is a heavy focus on patients paying out of pocket for not only their surgeries but also high-margin premium IOLs, which Ms. Wiltshire says well over 95% of patients receive. “It comes with a different level of handholding and expectation-setting with the patient initially, but it’s amazing technology that should definitely be offered if a patient is a candidate,” she says, adding it’s not a tough sell. “Dr. Shatz does it every day,” she says. “He’s got a speech prepared.”
Dr. Shatz says pairing premium IOLs with bilateral same-day procedures makes clinical as well as financial sense. “If you’re having premium lens surgery, the sooner you get both eyes operated on relative to each other, the quicker the brain adapts,” he says. “It readjusts much faster to their quality of vision. If you wait days, weeks or months between eyes, some patients have a very hard time adapting.”
Many eye surgeons reject bilateral same-day surgery because they prefer to do one eye days or weeks before the second, which affords them the refractive insight to confirm quality of vision in the first eye and adjust their plan for the second if needed. “A lot of doctors want to see the result of the first eye, so they’re scared to do both the same day,” Dr. Shatz acknowledges. “We’ve seen no real difference in frequency of patients having one eye’s prescription significantly off.”

Dr. Shatz says most eye surgeons, fairly conservative and risk-averse in their practices, lack strong incentive to embrace bilateral same-day surgery due to the lack of insurance reimbursement combined with the fear of the unknown that comes with such a big change in practice. In South Florida, SightTrust has no competitors in this subspecialty. The rest of the market is doing fine offering traditional cataract surgeries under the Medicare/insurance model, and doesn’t feel competitive pressure to change.
Even if the reimbursement piece was in place, Dr. Shatz doesn’t believe it would spur wide adoption. “A doctor has to see in their mind that it really provides a major benefit,” he says. “If the majority of their patients are in their mid-to-late 70s with significantly dense cataracts and health issues, they may want to wait until the first eye heals.” He adds that while younger ophthalmologists get the concept, those who might perform it are stymied because most join larger surgeon groups that forbid the practice.
Dr. Shatz says high patient volumes are vital to make bilateral same-day surgery work. “If you’re doing less than 500 surgeries a year, there’s no incentive to clear up your space and do half the amount of patients in a day,” he says. ASCs, he says, will likely not be interested in the practice due to the poor reimbursement picture unless their surgeon-owners collectively make a strong push for adoption.
Efficiencies abound
Ultimately, bilateral same-day cataract surgery is a patient pleaser for SightTrust due to time savings: halved surgical and postoperative visits, less confusing post-op drop regimens, and a quicker pathway to improved binocular vision.
“We live in a time where convenience is king, and to pay a little extra to not be out of work or contend with childcare and different things that really inconvenience a person’s day-to-day, it’s self-care to some degree,” says Ms. Wiltshire, who notes SightTrust consistently receives five-star Google reviews. “The market has shown us this is here to stay. Patients will pay out-of-pocket for premium IOLs, for laser, for same-day surgery. We just believe in it, and we never went back.
“If we were to tell our patients after surgery, ‘Oh, by the way, you could have had the eyes done individually,’ they’d probably look at us like we were crazy,” she says. “There really haven’t been any negatives or downsides to it that I can think of.” OSM
Related Articles
Behind closed doors: to knee or not to knee.
The date was set for Knee Replacement No. 1, aka “Laverne....”
Photo Essay: That’s a Wrap
In March, the Outpatient Surgery Magazine editors headed down to Nashville to attend AORN Global Surgical Conference & Expo, the 71st edition of the popular event....
Business Advisor: Meeting the Demand for a Larger Workforce
The aging population has increased the need for healthcare services as older individuals require more medical services and care....
Partner With Us!
Connect with 100,000+ outpatient OR leaders through print and digital advertising, custom programs, e-newsletters, event sponsorship, and more!
AORN Enterprise
Quick links.
Carl Zeiss Meditec AG Completes Acquisition of Dutch Ophthalmic Research Center (D.O.R.C.); Companies Unite to Shape Ophthalmology Market
Zeiss secures regulatory approvals to acquire d.o.r.c.; companies now shift focus to integration implementation, fueling world-class innovation, and driving market expansion strategy for ophthalmic medical devices and surgery..
Jena, Germany | April 4, 2024 | Carl Zeiss Meditec AG
Carl Zeiss Meditec AG announced today that, after securing all required regulatory approvals, it has completed the acquisition of 100% of D.O.R.C. (Dutch Ophthalmic Research Center) from the investment firm Eurazeo SE, Paris, France. The acquisition enhances and complements ZEISS Medical Technology’s broad ophthalmic portfolio and range of digitally connected workflow solutions for addressing a wide variety of eye conditions, spanning retina and cornea disorders, cataract, glaucoma, and refractive errors.
“Together we are better. Today holds significant importance for us as we bring our teams together and turn our collective attention toward delivering breakthrough innovations and solutions for our customers. We are very excited to welcome D.O.R.C.’s team members to our ZEISS family and to begin integrating our products and practices as we work toward a brighter future together,” says Dr. Markus Weber, President and CEO of Carl Zeiss Meditec AG.
“Together we can offer an unmatched portfolio of advanced technologies and digital workflows. With D.O.R.C., we have an incredible opportunity to serve ophthalmologists around the world with more complete workflows and solutions than ever before,” says Euan S. Thomson, Ph.D., President of Ophthalmology and Head of the Digital Business Unit for ZEISS Medical Technology. “We’ve set our sights high to become the top player in the world for ophthalmology by leveraging our workflow solutions, enhancing our portfolio offerings and market position in the anterior surgery segment, and by significantly expanding our presence in the posterior surgery segment.”
“Together we are stronger. With four decades behind our amazing business and surgeon-inspired innovation, we look forward to writing the next chapter of our success story together with ZEISS Medical Technology,” says Pierre Billardon, CEO of D.O.R.C. “By joining forces, we can extend our reach, scale our efforts, and accelerate ophthalmic surgery advancements for more surgeons faster than before. I am filled with a great sense of pride and gratitude for every D.O.R.C. team member. Together, we have achieved so much to arrive at this pivotal moment in our journey. And together with ZEISS, we have so much more to accomplish in our bright future ahead to help patients see again.”
Combination of portfolios will create unmatched end-to-end solution within the digitally-connected ZEISS Retina Surgery Workflow
As a leading player in the retina surgical devices and consumables market, D.O.R.C.’s contributions will be critical to ZEISS Medical Technology’s long-term strategy and success going forward. With D.O.R.C., ZEISS is in a unique position to offer an unmatched portfolio of market-leading technologies to ophthalmologists, including an expanded, digitally-connected Retina Surgery Workflow from ZEISS. The companies’ portfolios are highly complementary and the powerful combination of the EVA NEXUS® platform from D.O.R.C. with ZEISS’s extensive range of visualization, diagnostic and therapeutic devices, and surgical instruments and consumables, all connected to a digital ecosystem, will enable the creation of efficient clinical workflows that will reshape the ophthalmology market for the benefit of surgeons and their patients alike.
D.O.R.C. brings to the acquisition one of the market’s most advanced dual-function systems - the EVA NEXUS platform. EVA NEXUS is the core of a strong portfolio, comprising a full range of accessories, instruments and liquids, offering one of the best-in-class solutions across vitreo-retinal (VR) and combined cataract procedures. The expansion that D.O.R.C.’s overall portfolio brings to ZEISS ensures that surgeons will have more options to choose the solutions that best meet their specific surgical requirements and preferences.
With the completion of this acquisition, health care professionals can expect to benefit from an extensive and unique combination of digitally connected devices and workflow solutions, from clinical pre-operative needs to the surgical operating room. This supports efficient clinical workflows and helps surgeons to improve outcomes for their patients. The two companies’ immediate priorities span maintaining business continuity and customer satisfaction, cultivating areas of deep expertise, and enhancing the value of their solutions and services for current and future customers.
Not all products, services or offers are approved or offered in every market and approved labeling and instructions may vary from one country to another. For country-specific product information, see the appropriate country website. Product specifications are subject to change in design and scope of delivery as a result of ongoing technical development.
Head of Group Finance and Investor Relations Carl Zeiss Meditec AG
- +49 3641 220-116
- Download vCard
Head of Global Communications Ophthalmology Carl Zeiss Meditec AG
- +1 925 487 3036
About Carl Zeiss Meditec AG
Carl Zeiss Meditec AG (ISIN: DE0005313704), which is listed on the MDAX and TecDAX of the German stock exchange, is one of the world's leading medical technology companies. The Company supplies innovative technologies and application-oriented solutions designed to help doctors improve the quality of life of their patients. The Company offers complete solutions, including implants and consumables, to diagnose and treat eye diseases. The Company creates innovative visualization solutions in the field of microsurgery. With approximately 4,823 employees worldwide, the Group generated revenue of €2,089.3m in fiscal year 2022/23 (to 30 September).
The Group’s head office is located in Jena, Germany, and it has subsidiaries in Germany and abroad; more than 50 percent of its employees are based in the USA, Japan, Spain and France. The Center for Application and Research (CARIn) in Bangalore, India and the Carl Zeiss Innovations Center for Research and Development in Shanghai, China, strengthen the Company's presence in these rapidly developing economies. Around 41 percent of Carl Zeiss Meditec AG’s shares are in free float. The remaining approx. 59 percent are held by Carl Zeiss AG, one of the world’s leading groups in the optical and optoelectronic industries.
For more information visit our website at www.zeiss.com/med
About D.O.R.C. Dutch Ophthalmic Research Center (International) B.V.
D.O.R.C. is one of the world’s leading suppliers of equipment, instruments, and liquids for ophthalmic surgery. For 40 years, D.O.R.C. has grown into a successful international business, shaping its product portfolio through close collaboration with leading top surgeons. The company improves eye surgery globally and maximizes surgeon control by providing innovative quality approaches for eye disorders. Its products are exported to more than 80 countries worldwide. The company is headquartered in Zuidland, the Netherlands, and has more than 800 employees.
Further articles

Publication of a Related Party Transaction pursuant to Article 111c of the AktG with the aim of European distribution
Press portal.
Get all press releases of the Carl Zeiss Meditec AG here:

IMAGES
VIDEO
COMMENTS
Cataract surgery is a procedure to remove the lens of the eye and, in most cases, replace it with an artificial lens. A cataract causes the lens to become cloudy when it is typically clear. Cataracts can eventually affect vision. Cataract surgery is performed by an eye doctor, also called an ophthalmologist.
Cataract surgery is a quick, painless surgery to remove a cloudy lens that's causing vision issues. You receive a new intraocular lens that also corrects nearsightedness and farsightedness. You only need surgery if cataracts keep you from doing your usual tasks. Surgery improves vision for 97% of people.
The National Eye Institute (NEI) provides the following guidelines for preparing for cataract surgery:. Visiting the eye doctor: About a week before surgery, an ophthalmologist will measure the ...
Most people can resume driving a day after cataract surgery. However, others experience blurry vision that can last for several days. ... Follow-up visits: Schedule a follow-up appointment with your doctor within 24 to 48 hours after the surgery. Moreover, continue these visits to ensure a safe recovery. Potential Side Effects .
Some studies have questioned the need for a one-day post-op visit after uncomplicated cataract surgery, given the expected low risk of complications. 1 However, it is still part of many surgeons' postoperative protocols. There are several important things that need to be assessed at this early visit. First, evaluate the eye for a wound leak.
In the Future. Most people can see much better after cataract surgery. The procedure helps fix problems like blurry vision, glare, and sensitivity to light. However, these effects won't be immediate. Your cataract surgery recovery includes time for your eye to heal and adjust. Here is what you can expect in the first few days, weeks and ...
The week after your surgery, your vision may remain a bit blurred. You can speed recovery by avoiding grit, water, and contamination. After a month, you may have crisp vision, but your eye is still healing and you will still need to follow your doctor's orders. After eight weeks, your healing is complete.
Recovery at home after cataract surgery. You will see your ophthalmologist for several postoperative visits—typically one day, one week, one month, two months, and six months after surgery. At each appointment, the doctor will examine your eye, test your visual acuity, and measure your eye pressure.
During surgery, your eye doctor will remove the cloudy lens from your eye and replace it with an artificial lens (called an intraocular lens, or IOL). The surgery lasts about 1 hour and is almost painless. Usually, you'll be awake during cataract surgery. You might notice lights or motion, but you won't be able to see what your doctor is doing.
Cataract surgery will not restore vision lost from other eye conditions, such as macular degeneration, glaucoma, or diabetic retinopathy. Your ophthalmologist will talk with you about the risks and benefits of cataract surgery. Posterior Capsular Opacification. Your vision could become cloudy or blurry weeks, months or years after cataract surgery.
Your ophthalmologist will provide you with clear, detailed instructions for the hours, days, and weeks after your cataract surgery. General tips for post-cataract surgery care include: Avoid heavy lifting or strenuous exercise for a few weeks. Do not bend over for a couple days. Avoid swimming for the weeks following surgery.
Request an Appointment. 410-955-5080 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. Recovery from cataract surgery can be seamless as you ease back into your daily life. These 5 tips from a Johns Hopkins expert help you get through the healing process and have your vision restored on time.
soreness. watery eyes. double vision. eye redness. a gritty feeling in the eye. sensitivity to light. These often resolve after a few days, but it can take up to 8 weeks for a full recovery. Learn ...
After cataract surgery, people will need to avoid: rubbing or touching the eye. getting soap or shampoo in the eye. swimming for 4-6 weeks. strenuous activity or exercise. wearing makeup for 4 ...
Week One. After one week post-surgery, it is essential that you visit your physician to check on how well the eye has recovered. Any swelling should have subsided by now and vision should be clearer than it was shortly following your procedure. At this visit, your doctor will perform a comprehensive exam on both of your eyes, test visual acuity ...
Your cataract surgery recovery should be short and uneventful, as long as you follow the post-op instructions you receive from your surgeon and attend all recommended follow-up visits with your eye doctor.. Uncomplicated cataract surgery usually takes no longer than about 10 minutes to perform. Immediately after the surgery, you will rest in a recovery area until you are less groggy from ...
Eyes without unusual risk factors seem to have no increased risk of retinal tear or detachment after cataract surgery. 16 Myopic and lattice degeneration patients, on the other hand, do have an increased risk for up to 10 years after cataract surgery. 17 You should caution at-risk patients about the usual symptoms. 17
After cataract surgery, it's important to follow a few simple steps to make sure the eye heals properly. Learn more about cataract surgery and what you can expect before, during, and after surgery. ... Be prepared for at least two to three visits. When to call the doctor. While cataract surgery is quite safe, there are still things you'll ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. Cataract surgery is a commonly performed surgical procedure that involves swapping out the cloudy natural lens of the eye with a new artificial lens.
After surgery, your eye may feel scratchy, sticky, or uncomfortable. It may also water more than usual. Most people see better 1 to 3 days after surgery. But it could take 3 to 10 weeks to get the full benefits of surgery and to see as clearly as possible. Your doctor may send you home with a bandage, patch, or clear shield on your eye.
During surgery, your eye doctor uses a medicine to numb the area around your eye. You usually stay awake during the procedure. Cataract surgery is generally safe. However, it carries a risk of infection and bleeding. Cataract surgery also increases the risk of the retina being pulled out of place.
When addressing visual concerns post-surgery, Dr. Meghpara suggests tools like iTrace can be helpful. "This diagnostic tool performs both corneal topography and wavefront aberrometry," he says. "If you conduct this test on a patient after cataract surgery, the image quality should be excellent (9 or 10 on a scale of 10).
• By age 80, over half of all Americans have cataracts. • Close to 4 million cataract surgeries are performed in the U.S. every year. • Over 90% of patients have 20/20 vision with glasses ...
After surgery, there's no bending, inversions, lifting or straining, high-impact activities or eye makeup for one to two weeks or until the doctor says it's OK. About the Surgery Cataract surgery removes the clouded lens of the eye and replaces it with a new, clear lens to restore your vision.
SightTrust's two-OR facility and workflow is designed specifically to make the "dual surgery" system as routine and efficient as possible. Suddenly 25% of our caseload was bilateral, then 50%, then 75%. We got to 100% quickly. When a patient arrives, they're immediately taken to prep.
Carl Zeiss Meditec AG announced today that, after securing all required regulatory approvals, it has completed the acquisition of 100% of D.O.R.C. (Dutch Ophthalmic Research Center) from the investment firm Eurazeo SE, Paris, France. The acquisition enhances and complements ZEISS Medical Technology's broad ophthalmic portfolio and range of ...