You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 2 - Interactions Between Travel Vaccines & Drugs
- Section 2 - Travelers’ Diarrhea

Yellow Fever Vaccine & Malaria Prevention Information, by Country
Cdc yellow book 2024.
Author(s): Mark Gershman, Rhett Stoney (Yellow Fever) Holly Biggs, Kathrine Tan (Malaria)
The following pages present country-specific information on yellow fever (YF) vaccine requirements and recommendations, and malaria transmission information and prevention recommendations. Country-specific maps are included to aid in interpreting the information. The information in this chapter was accurate at the time of publication; however, it is subject to change at any time due to changes in disease transmission or, in the case of YF, changing entry requirements for travelers. Updated information reflecting changes since publication can be found in the online version of this book and on the Centers for Disease Control and Prevention (CDC) Travelers’ Health website. Recommendations for prevention of other travel-associated illnesses can also be found on the CDC Travelers’ Health website .
Yellow Fever Vaccine
Entry requirements.
Entry requirements for proof of YF vaccination under the International Health Regulations (IHR) differ from CDC’s YF vaccination recommendations. Under the IHR, countries are permitted to establish YF vaccine entry requirements to prevent the importation and transmission of YF virus within their boundaries. Certain countries require proof of vaccination from travelers arriving from all countries ( Table 5-25 ); some countries require proof of vaccination only for travelers above a certain age coming from countries with risk for YF virus transmission. The World Health Organization (WHO) defines areas with risk for YF virus transmission as countries or areas where YF virus activity has been reported currently or in the past, and where vectors and animal reservoirs exist.
Unless issued a medical waiver by a yellow fever vaccine provider, travelers must comply with entry requirements for proof of vaccination against YF.
WHO publishes a list of YF vaccine country entry requirements and recommendations for international travelers approximately annually. But because entry requirements are subject to change at any time, health care professionals and travelers should refer to the online version of this book and the CDC Travelers’ Health website for any updates before departure.
CDC Recommendations
CDC’s YF vaccine recommendations are guidance intended to protect travelers from acquiring YF virus infections during international travel. These recommendations are based on a classification system for destination-specific risk for YF virus transmission: endemic, transitional, low potential for exposure, and no risk ( Table 2-08 ). CDC recommends YF vaccination for travel to areas classified as having endemic or transitional risk (Maps 5-10 and 5-11 ). Because of changes in YF virus circulation, however, recommendations can change; therefore, before departure, travelers and clinicians should check CDC’s destination pages for up-to-date YF vaccine information.
Duration of Protection
In 2015, the US Advisory Committee on Immunization Practices published a recommendation that 1 dose of YF vaccine provides long-lasting protection and is adequate for most travelers. The recommendation also identifies specific groups of travelers who should receive additional doses, and others for whom additional doses should be considered (see Sec. 5, Part 2, Ch. 26, Yellow Fever ). In July 2016, WHO officially amended the IHR to stipulate that a completed International Certificate of Vaccination or Prophylaxis is valid for the lifetime of the vaccinee, and YF vaccine booster doses are not necessary. Moreover, countries cannot require proof of revaccination (booster) against YF as a condition of entry, even if the traveler’s last vaccination was >10 years ago.
Ultimately, when deciding whether to vaccinate travelers, clinicians should take into account destination-specific risks for YF virus infection, and individual risk factors (e.g., age, immune status) for serious YF vaccine–associated adverse events, in the context of the entry requirements. See Sec. 5, Part 2, Ch. 26, Yellow Fever , for a full discussion of YF disease and vaccination guidance.
Table 2-08 Yellow fever (YF) vaccine recommendation categories 1
Malaria prevention.
The following recommendations to protect travelers from malaria were developed using the best available data from multiple sources. Countries are not required to submit malaria surveillance data to CDC. On an ongoing basis, CDC actively solicits data from multiple sources, including WHO (main and regional offices); national malaria control programs; international organizations; CDC overseas offices; US military; academic, research, and aid organizations; and the published scientific literature. The reliability and accuracy of those data are also assessed.
If the information is available, trends in malaria incidence and other data are considered in the context of malaria control activities within a given country or other mitigating factors (e.g., natural disasters, wars, the coronavirus disease 2019 pandemic) that can affect the ability to control malaria or accurately count and report it. Factors such as the volume of travel to that country and the number of acquired cases reported in the US surveillance system are also examined. In developing its recommendations, CDC considers areas within countries where malaria transmission occurs, substantial occurrences of antimalarial drug resistance, the proportions of species present, and the available malaria prophylaxis options.
Clinicians should use these recommendations in conjunction with an individual risk assessment and consider not only the destination but also the detailed itinerary, including specific cities, types of accommodations, season, and style of travel, as well as special health conditions (e.g., pregnancy). Several medications are available for malaria prophylaxis. When deciding which drug to use, consider the itinerary and length of trip, travelers’ previous adverse reactions to antimalarials, drug allergies, medical history, and drug costs. For a thorough discussion of malaria and guidance for prophylaxis, see Sec. 5, Part 3, Ch. 16, Malaria .
Entry requirements : Required for travelers ≥9 months old arriving from countries with risk for YF virus transmission; this includes >12-hour airport transits or layovers in countries with risk for YF virus transmission. 1
CDC recommendations : Not recommended
- Primarily the provinces that border Burma, Cambodia (few cases in Buri Ram Province), and Malaysia (few cases in Satun Province) Also, the provinces of Phitsanulok and Ubon Ratchathani (bordering Laos), and Surat Thani (especially in the rural forest and forest-fringe areas of these provinces)
- Rare to few cases in other parts of Thailand, including the cities of Bangkok (the capital), Chiang Mai, and Chiang Rai, or on the islands of Koh Pha Ngan, Koh Samui, or Phuket
- No malaria transmission on the islands of Krabi Province (Ko Lanta, Koh Phi, Koh Yao Noi, Koh Yao Yai) or in Pattaya City
- Chloroquine and mefloquine
- P. vivax (80%)
- P. falciparum (<20%)
- P. knowlesi 6 , P. malariae , and P. ovale (rare)
- Provinces that border Burma, Cambodia (except Buri Ram Province), and Malaysia (except Satun Province); the provinces of Phitsanulok, Ubon Ratchathani, and Surat Thani: Atovaquone-proguanil, doxycycline, tafenoquine 3
- All other areas with malaria transmission (including the provinces of Buri Ram and Satun): No chemoprophylaxis recommended (insect bite precautions and mosquito avoidance only) 4
Related Maps
Map 2-16 malaria prevention in thailand, other vaccines to consider.
See Health Information for Travelers to Thailand .

View Larger
1 Current as of November 2022. This is an update of the 2010 map created by the Informal WHO Working Group on the Geographic Risk of Yellow Fever.
2 Refers to Plasmodium falciparum malaria, unless otherwise noted.
3 Tafenoquine can cause potentially life-threatening hemolysis in people with glucose-6-phosphate-dehydrogenase (G6PD) deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing tafenoquine to patients.
4 Mosquito avoidance includes applying topical mosquito repellant, sleeping under an insecticide-treated mosquito net, and wearing protective clothing (e.g., long pants and socks, long-sleeve shirt). For additional details on insect bite precautions, see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods.
5 Primaquine can cause potentially life-threatening hemolysis in people with G6PD deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing primaquine to patients.
6 P. knowlesi is a malaria species with a simian (macaque) host. Human cases have been reported from most countries in Southwest Asia and are associated with activities in forest or forest-fringe areas. P. knowlesi has no known resistance to antimalarials.
Yellow Fever Maps
2 In 2017, the Centers for Disease Control and Prevention (CDC) expanded its YF vaccination recommendations for travelers going to Brazil because of a large YF outbreak in multiple states in that country. Please refer to the CDC Travelers’ Health website for more information and updated recommendations.
3 YF vaccination is generally not recommended for travel to areas where the potential for YF virus exposure is low. Vaccination might be considered, however, for a small subset of travelers going to these areas who are at increased risk for exposure to YF virus due to prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites. Factors to consider when deciding whether to vaccinate a traveler include destination-specific and travel-associated risks for YF virus infection; individual, underlying risk factors for having a serious YF vaccine–associated adverse event; and destination entry requirements.
The following authors contributed to the previous version of this chapter: Mark D. Gershman, Emily S. Jentes, Rhett J. Stoney (Yellow Fever) Kathrine R. Tan, Paul M. Arguin (Malaria)
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Situation in Haiti April 5, 2024
U.s. citizens in haiti, update january 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Before You Go
Learn About Your Destination
While Abroad
Emergencies
Share this page:
Travel Advisory July 24, 2023
Thailand - level 1: exercise normal precautions.
Reissued with obsolete COVID-19 page links removed.
Exercise normal precautions in Thailand. Some areas have increased risk. Read the entire Travel Advisory.
Reconsider travel to:
- Yala, Pattani, Narathiwat, and Songkhla provinces due to civil unrest associated with ongoing insurgent activities.
Read the country information page for additional information on travel to Thailand.
If you decide to travel to Thailand:
- Enroll in the Smart Traveler Enrollment Program (STEP) to receive Alerts and make it easier to locate you in an emergency.
- Follow the Department of State on Facebook and Twitter .
- Review the Country Security Report for Thailand.
- Have evacuation plans that do not rely on U.S. government assistance.
- Visit the CDC page for the latest Travel Health Information related to your travel.
- Prepare a contingency plan for emergency situations. Review the Traveler’s Checklist .
Yala, Pattani, Narathiwat, and Songkhla Provinces – Level 3: Reconsider Travel
Periodic violence directed mostly at Thai government interests by a domestic insurgency continues to affect security in the southernmost provinces of Yala, Pattani, Narathiwat, and Songkhla. In Songkhla, the insurgency is most active in the districts of Chana, Thepha, Nathawat, and Saba Yoi. U.S. citizens are at risk of death or injury due to the possibility of indiscriminate attacks in public places.
The U.S. government has limited ability to provide emergency services to U.S. citizens in these provinces as U.S government employees must obtain special authorization to travel to these provinces.
Visit our website for Travel to High-Risk Areas .
Embassy Messages
View Alerts and Messages Archive
Quick Facts
6 months from date of entry required
One page is required per entry stamp; please note endorsement pages are not considered blank passport page
No, if your stay is less than 30 days
Yellow fever may be required if arriving from certain countries with yellow fever
Embassies and Consulates
U.S. Embassy Bangkok 95 Wireless Road Bangkok 10330 Thailand Telephone: + (66) (2) 205-4049, 02-205-4049 (within Thailand) Emergency After-Hours Telephone: +(66) (2) 205-4000, 02-205-4000 (within Thailand) Fax: +(66) (2) 205-4103, 02-205-4103 (within Thailand) Email: [email protected]
CONSULATE
U.S. Consulate General Chiang Mai 387 Witchayanond Road Chiang Mai 50300 Thailand Telephone: +(66) (53) 107-777, 053-107-777 (within Thailand) Emergency After-Hours Telephone: +(66) 81-881-1878, 081-881-1878 (within Thailand) Fax: +(66) (53) 252-633, 053-252-633 (within Thailand) Email: [email protected]
Destination Description
Learn about the U.S. relationship to countries around the world.
Entry, Exit and Visa Requirements
Visit the Royal Thai Embassy website for the most current visa information.
- U.S. citizen tourists entering Thailand for fewer than 30 days do not require a visa.
- We strongly recommend that your passport be valid for at least six months beyond the date of your arrival in Thailand to avoid possible denied entry.
- Thai immigration officials or airline staff may ask for your onward/return ticket.
- Business travelers, U.S. government employees travelling on official business, teachers, retirees, and those planning to stay longer than 30 days should check with the Royal Thai Embassy about visa requirements .
- If you overstay your visa, you will be fined. Depending on the length of overstay, you may also be arrested, detained, deported at your own expense, and banned from re-entering Thailand.
We strongly recommend you carry a copy of your U.S. passport identification page and current Thai visa to help avoid detention by the Thai immigration police.
Thailand’s entry/exit information is subject to change without notice. For the most current information, please see The Royal Thai Police Immigration Bureau .
You can find detailed information on vaccinations and other health precautions on the CDC website .
HIV/AIDS Restrictions: Some HIV/AIDS entry restrictions exist for visitors to and foreign residents of Thailand. However, these restrictions are generally not enforced. Please verify this information with the Royal Thai Embassy before you travel.
Find information on dual nationality , prevention of international child abduction and customs regulations on our websites.
COVID-19 Requirements: There are no COVID-related entry requirements for U.S. citizens.
Safety and Security
Terrorism: Terrorist groups and those inspired by such organizations are intent on attacking U.S. citizens abroad. Terrorists are increasingly using less sophisticated methods of attack – including knives, firearms, and vehicles – to more effectively target crowds. Frequently, their aim is unprotected or vulnerable targets, such as:
- High-profile public events (sporting contests, political rallies, demonstrations, holiday events, celebratory gatherings, etc.)
- Hotels, clubs, and restaurants frequented by tourists
- Places of worship
- Shopping malls and markets
- Public transportation systems (including subways, buses, trains, and scheduled commercial flights)
For more information, see our Terrorism page.
Periodic acts of violence in Thailand remain a concern. In August 2019, several small explosions and related arson events occurred in various locations throughout Bangkok resulting in no deaths but some injuries and minor property damage. Several small-scale bombings occurred near some tourist locations in the far Southern provinces in August 2016 and December 2018. In August 2015, an explosion near the Erawan Shrine in downtown Bangkok killed at least 20 people and injured more than 100. The U.S. Department of State assesses there is a continued risk of terrorism in Southeast Asia, including in Thailand.
If a protest or demonstration is expected to pass near the U.S. Embassy or Consulate facilities, Embassy and Consulate entrances and functions may be restricted. The U.S. Embassy in Bangkok’s website , Facebook, and Twitter sites and the U.S. Consulate General in Chiang Mai’s website , Facebook , and Twitter sites post information about local events that may affect Embassy functions. Enroll in the Smart Traveler Enrollment Program ( STEP ) to receive security and safety messages.
Far Southern Thailand: Periodic violence directed mostly at Thai government interests by a domestic insurgency continues to affect security in the southernmost provinces of Yala, Pattani, Narathiwat, and Songkhla. U.S. citizens are at risk of death or injury due to the possibility of indiscriminate attacks in public places. Martial law is in force in this region.
The U.S. government has limited ability to provide emergency services to U.S. citizens in these provinces. Travel to this region by U.S government employees must be reviewed and approved in advance. For more information on terrorist threats against U.S. citizens worldwide and steps to take as a result of these threats, please see the Worldwide Caution .
- Crimes of opportunity, such as pick-pocketing, bag-snatching, and burglary, occur in Thailand.
- Violent crimes against foreigners are relatively rare. However, murders, rapes, and assaults against foreigners do occur.
- Sexually motivated violence, committed by either Thai citizens or foreigners, is most likely to occur after time spent at bars, clubs, and parties, on beaches, or in remote/isolated areas. The Thai police response will differ from an investigation in the United States; investigating officials have publicly discredited people who have reported being the victim of crimes . In addition to making a report at the police jurisdiction in which the crime occurred, we advise contacting the Embassy and engaging a local attorney if you are a victim of an assault.
- When traveling alone, exercise caution, stay near other travelers, and ensure friends or family know how to contact you.
- Taxi and “tuk-tuk” drivers may attempt to charge excessive fares or refuse passengers. You should either request the driver use the meter or agree on the fare beforehand.
- At the airport use only public transportation from the airport’s official pick-up area, cars from the limousine counters, or a car from your hotel.
- Rental scams do occur in Thailand. Many rental motorbike, jet ski, and car companies will hold your passport until you pay for real or fictitious damages. We advise against using your passport as collateral.
- Exorbitant bar tab scams occur in Thailand. Some bars and entertainment venues will charge exorbitant prices for drinks or unadvertised cover charges and threaten violence if you don’t pay.
- Other scams involving gems, city tours, entertainment venues, and credit cards are common, especially in tourist areas.
International Financial Scams: See the Department of State and the FBI pages for information.
Internet romance and financial scams are prevalent in Thailand. Scams are often initiated through Internet postings/profiles or by unsolicited emails and letters. Scammers almost always pose as U.S. citizens who have no one else to turn to for help. Common scams include:
- Romance/Online dating
- Money transfers
- Grandparent/Relative targeting
- Free Trip/Luggage
- Work permits/job offers
Victims of Crime: U.S. citizen victims of crime are encouraged to contact the U.S. Embassy or Consulate for assistance. Report crimes to the local police by calling 191 or the Tourist Police at 1155 and contact the U.S. Embassy at +66 (0) 2-205-4049 or Consulate at +(66) (53) 107-777. Remember that only local officials have the authority to investigate and to prosecute a crime.
Domestic Violence: U.S. citizen victims of domestic violence are encouraged to contact the U.S. Embassy or Consulate for assistance. Report crimes to the local police by calling 191 or the Tourist Police at 1155 and contact the U.S. Embassy at +66 (0) 2-205-4049 or Consulate at +(66) (53) 107-777. Remember that only local officials have the authority to investigate and to prosecute a crime.
See our webpage on help for U.S. victims of crime overseas .
- Help you find appropriate medical care
- Assist you in reporting a crime to the police
- Contact relatives or friends with your written consent
- Explain the local criminal justice process in general terms
- Provide a list of local attorneys
- Provide our information on victim’s compensation programs in the U.S.
- Provide an emergency loan for repatriation to the United States and/or limited medical support in cases of destitution
- Help you find accommodation and arrange flights home
- Replace a stolen or lost passport
Tourism: The tourism industry is unevenly regulated, and safety inspections for equipment and facilities do not commonly occur. Hazardous areas/activities are not always identified with appropriate signage, and staff may not be trained or certified either by the host government or by recognized authorities in the field. In the event of an injury, appropriate medical treatment is typically available only in/near major cities. First responders are generally unable to access areas outside of major cities and to provide urgent medical treatment. U.S. citizens are encouraged to purchase medical evacuation insurance. See our webpage for more information on insurance providers for overseas coverage .
Local Laws & Special Circumstances
Criminal Penalties: You are subject to local laws. If you violate local laws, even unknowingly, you may be expelled, arrested, or imprisoned. Individuals establishing a business or practicing a profession that requires additional permits or licensing should seek information from the competent local authorities, prior to practicing or operating a business.
Furthermore, some laws are also prosecutable in the United States, regardless of local law. For examples, see our website on crimes against minors abroad and the Department of Justice website.
Arrest Notification: If you are arrested or detained, ask police or prison officials to notify the U.S. Embassy immediately. See our webpage for further information.
Conditions at the Bangkok Immigration Detention Center (IDC): Conditions in immigration detention centers (IDCs) where authorities detain foreign nationals who violate immigration laws remain poor and most are overcrowded. IDCs, administered by the Immigration Police Bureau, which reports to the Royal Thai Police (RTP), are not subject to many of the regulations that govern the regular prison system. U.S. citizen detainees often complain of stark, austere living conditions, overcrowding, and unhealthy conditions. Personal security is poor. In addition, the main IDC in Bangkok does not dependably provide adequate medical or mental health care. In 2019, two U.S. citizens died while in custody at the Bangkok IDC. Deportations are self-funded and it may take up to two weeks for Thai authorities to process a case before deportation. Detainees must have funds to purchase a phone card and do not have access to the internet. Prior approval and a security escort are required to visit a Western Union or an ATM machine.
- Please see the Immigration Act B.E. 1979 for more information about Thai Immigration violations.
- Please see the Department of State’s Report on Human Rights Practices for Thailand for further information.
Lèse majesté (Royal Insult): Thais hold the monarchy in the highest regard. Making a critical or defamatory comment about the royal family is punishable by a prison sentence of up to 15 years per offense. As an example, purposely tearing Thai bank notes, which carry an image of the King, may be considered a lèse majesté offense.
- Prostitution is illegal in Thailand. Serious consequences include criminal conviction and imprisonment, particularly in the case of child prostitution.
- Commercial surrogacy is banned.
- Personal use of even non-lethal military equipment, such as protective vests and night vision scopes, is prohibited.
- Illegal drugs carry severe penalties. Expect long jail sentences under harsh conditions, heavy fines, or even execution for possessing, using, or trafficking in illegal drugs.
- Shoplifting can result in large fines and lengthy detention followed by deportation.
- Domestic Issues: Local police are reluctant to become involved in domestic issues. You may call the Family Services Emergency hotline by dialing 1300 from any Thai phone.
- Possessing counterfeit or pirated goods is a crime in Thailand. For more information see the intellectual property section of the U.S. Department of Justice website .
Customs may enforce strict regulations on Buddha images, firearms, bullets and/or bullet casings, bullet-proof vests, night vision devices and other para-military type equipment, explosives, drugs, radios, books, and recordings, which might be cultural property and/or considered harmful to the public interest.
Faith-Based Travelers: See the following webpages for details:
- Faith-Based Travel Information
- International Religious Freedom Report – see country reports
- Human Rights Report – see country reports
- Hajj Fact Sheet for Travelers
- Best Practices for Volunteering Abroad
LGBTI Travelers: There are no known legal restrictions on same-sex sexual relations or the organization of LGBTI events in Thailand. However, LGBTI groups report that in the case of sexual crimes, police tend to downplay sexual abuse claims from LGBTI victims.
See our LGBTI Travel Information page and section 6 of our Human Rights report for further details.
Travelers Who Require Accessibility Assistance. Sidewalks and street crossings are not suitable for travelers with mobility issues. Newly constructed buildings, facilities, and transportation equipment should be accessible by law for persons with mobility issues. However, enforcement of these provisions is not uniform.
Students: See our Students Abroad page and FBI travel tips .
Women Travelers: Some victims of sexual assault or domestic violence find that Thai authorities do not handle such cases with as much sensitivity or consideration for privacy as they would expect in the United States. See our travel tips for Women Travelers .
Ambulance services are:
- not present throughout the country or are unreliable in most areas except for Bangkok and other major cities.
- Injured or seriously ill travelers may prefer to take a taxi or private vehicle to the nearest major hospital rather than wait for an ambulance.
Medical treatment is generally adequate in Thailand’s urban areas. In Bangkok, Chiang Mai, Phuket, and Pattaya, good facilities exist for routine, long-term, and emergency health care. Basic medical care is available in rural areas, but English-speaking providers are rare.
Medical tourism is an established and rapidly growing industry. You should consult with your local physician before traveling and also refer to information on medical tourism from CDC.
We do not pay medical bills. Be aware that U.S. Medicare/Medicaid does not apply overseas. Most hospitals and doctors overseas do not accept U.S. health insurance.
Medical Insurance: Make sure your health insurance plan provides coverage overseas. Most care providers overseas only accept cash payments. See our webpage for more information on insurance providers for overseas coverage. Visit the U.S. Centers for Disease Control and Prevention for more information on type of insurance you should consider before you travel overseas.
We strongly recommend supplemental insurance to cover medical evacuation.
Medicine for personal use is allowed as long as the amount does not exceed a 30-day supply and you bring the medicine with you. Do not mail medicine to Thailand without first confirming it will be allowed into the country.
If traveling with prescription medication, check with Thailand Customs and the Thailand Food and Drug Administration to ensure the medication is legal in Thailand. Always, carry your prescription medication in original packaging with your doctor’s prescription.
The following diseases are present:
- Chikungunya
- Japanese encephalitis
- Tuberculosis:
- Hepatitis A and B
- Melioidosis
Vaccinations: Be up-to-date on all vaccinations recommended by the U.S. Centers for Disease Control and Prevention.
Further health information:
- World Health Organization
- U.S. Centers for Disease Control and Prevention (CDC)
Air Quality: The air quality in Thailand varies considerably and fluctuates with the seasons, but seasonal smog is a problem. In recent years the air quality in Bangkok, Chiang Mai, Khon Kaen, Lampang, Nan, and Samut Sakhon have exceeded Thai and U.S. government daily standards for fine particulate matter (PM 2.5) for a portion of the year. In Chiang Mai and other northern provinces, annual agricultural burning, approximately February through late April, and forest fires cause days with unhealthy to hazardous air quality based on the U.S. index. In Bangkok environs, airborne dust and auto pollutants are prevalent in the cooler, dry period (December-February). Anyone who travels where pollution levels are high is at risk. People at the greatest risk from air pollution exposure include:
- Infants, children, and teens
- People over 65 years of age
- People with lung disease such as asthma and chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema;
- People with heart disease
- People who work or are active outdoors
For Bangkok and Chiang Mai, U.S. Mission Thailand is reporting the U.S. EPA’s Air Quality Index (AQI) calculated from PM2.5 data captured by monitors owned and maintained by the Royal Thai Government. The information and advice on health protection measures to take is available
Visit AirNow Department of State for information on air quality at U.S. Embassies and Consulates.
The U.S. Embassy maintains a list of doctors and hospitals . We do not endorse or recommend any specific medical provider or clinic.
Health facilities in general:
- Adequate health facilities are available in Bangkok and other major cities but health care in rural areas may be below U.S. standards.
- Hospitals and doctors require payment “up front” prior to service or admission. Credit card payment is not always available.
- Medical staff at public hospitals may speak little or no English.
- Patients bear all costs for transfer to or between hospitals.
- Psychological and psychiatric services are limited, even in the larger cities, with hospital-based care only available through government institutions.
Medical Tourism and Elective Surgery:
- Medical tourism is a rapidly growing industry. People seeking health care overseas should understand that medical systems operate differently from those in the United States and are not subject to the same rules and regulations. Anyone interested in traveling for medical purposes should consult with their local physician before traveling and visit the U.S. Centers for Disease Control and Prevention website for more information on Medical Tourism.
- We strongly recommend supplemental insurance to cover medical evacuation in the event of unforeseen medical complications.
- Your legal options in case of malpractice are very limited in Thailand.
- Although Thailand has many elective/cosmetic surgery facilities that are on par with those found in the United States, the quality of care varies widely. If you plan to undergo surgery in Thailand, make sure that emergency medical facilities are available and professionals are accredited and qualified.
Pharmaceuticals:
- Exercise caution when purchasing medication overseas. Pharmaceuticals, both over the counter and requiring prescription in the United States, are often readily available for purchase with little controls. Counterfeit medication is common and may prove to be ineffective, the wrong strength, or contain dangerous ingredients. Medication should be purchased in consultation with a medical professional and from reputable establishments.
- U.S. Customs and Border Protection and the Food and Drug Administration are responsible for rules governing the transport of medication back to the United States. Medication purchased abroad must meet their requirements to be legally brought back into the United States. Medication should be for personal use and must be approved for usage in the United States. Please visit the U.S. Customs and Border Protection and the Food and Drug Administration websites for more information.
Assisted Reproductive Technology and Surrogacy:
- If you are considering traveling to Thailand to have a child through use of assisted reproductive technology (ART) or surrogacy, please see our ART and Surrogacy Abroad page .
- Surrogacy is illegal for foreigners in Thailand, subject to complex local regulation. For additional information, visit the Government of Thailand’s website for information on foreigner surrogacy.
- If you decide to pursue parenthood in Thailand via assisted reproductive technology (ART) with a gestational mother, be prepared for long and unexpected delays in documenting your child’s citizenship. Be aware that individuals who attempt to circumvent local law risk criminal prosecution.
Water Quality:
- In many areas, tap water is not potable. Bottled water and beverages are generally safe, although you should be aware that many restaurants and hotels serve tap water unless bottled water is specifically requested. Be aware that ice for drinks may be made using tap water.
Adventure Travel:
- Visit the U.S. Centers for Disease Control and Prevention website for more information about Adventure Travel .
COVID-19 Testing: For the most current list of COVID-19 testing locations in Thailand approved by the Ministry of Public Health, please visit: http://service.dmsc.moph.go.th/labscovid19 . Testing is paid for by U.S. citizens.
The Ministry of Public Health provides a list of 44 laboratories approved to conduct COVID-19 testing found here .
Please Note : Same-day Covid-19 testing is available at most private hospitals throughout Thailand. Please reference this list of testing locations and contact the provider directly to inquire about COVID-19 testing options, scheduling, cost, and other information.
COVID-19 Vaccines: The COVID-19 vaccine is available for U.S. citizens to receive in Thailand. According to Thai authorities, both private and public hospitals are providing COVID-19 vaccines. More information on a list of hospitals in Thailand is available here .
The Bang Rak Vaccination and Health Center, the Institute of Dermatology, and the Bamrasnaradura Infectious Diseases Institute are currently providing free bivalent vaccines to non-Thai citizens on a walk-in basis.
Visit the FDA's website to learn more about FDA-approved vaccines in the United States.
Travel and Transportation
Road Conditions and Safety:
- Traffic accidents are common in Thailand. According to the World Health Organization , in 2018, Thailand had one of the world’s highest traffic-related fatality rates. Bangkok and some parts of Chiang Mai have heavy traffic.
- Reckless driving: Speeding, reckless passing, and failure to obey other traffic laws are common in all regions of Thailand. Traffic moves on the left. Some drivers move illegally against the traffic. Scooters and motorbikes commonly drive on the sidewalks during rush hour and other periods of heavy traffic. Commercial drivers commonly consume alcohol, amphetamines, and other stimulants.
- Accidents involving motorcycles can be deadly . Riders may incur serious injuries when they are not wearing helmets or proper clothing and footwear. According to the World Health Organization, in 2016, 74 percent of traffic fatalities involved riders of 2-and 3-wheeled vehicles. Use of motorcycle helmets is mandatory, but this law is sporadically enforced.
- Use a pedestrian bridge to cross the road where one is available, including in front of the U.S. Embassy on Wireless Road and on Sukhumvit Road, where many pedestrians have been killed and several U.S. citizens seriously injured. Look carefully in both directions before crossing streets, even when using a marked crosswalk.
- If you have a traffic accident, you should contact your insurance company for guidance in dealing with the other party and the police.
- Emergency vehicles: Congested roads and a scarcity of ambulances can make it difficult for accident victims to receive timely medical attention
Traffic Laws:
- Driving under influence is punishable by law . If you are found to be intoxicated, you could be jailed for a minimum of two years and subject to a fine.
- Bribes are illegal. If you are found guilty, you could be imprisoned up to five years, face severe fines, or both.
- Lack of ID.
- Not obeying traffic laws and traffic signals.
- Driving slowly in regular lanes of traffic.
- If you are involved in a traffic accident, you should contact your auto insurance company for guidance .
Public Transportation:
- Mass transit: In Bangkok, the BTS elevated "Skytrain," “Airport Rail Link” mass transit, and the underground MRT systems are reliable, inexpensive, air conditioned, and often faster than Bangkok traffic.
- Bus system: Bangkok also has an extensive bus system, but buses can be overcrowded and are often driven with little or no regard for passenger safety.
- For hire vehicles: Cities outside of Bangkok typically have only rudimentary public transportation and usually do not have metered taxis. In many cases, motorcycle taxis, tuk-tuks, bicycle-powered rickshaws, and pick-up trucks will be the only options available for travelers without their own transport.
- Smartphone-based for-hire vehicle service exist in Bangkok and other large cities. Those affiliated with registered taxis, such as Grab Taxi, Line Taxi, and All Thai Taxi are legal, but their affiliated car services are under legal review.
See our Road Safety page for more information.
Aviation Safety Oversight: The U.S. Federal Aviation Administration (FAA) has assessed the government of Thailand’s Civil Aviation Authority as not being in compliance with International Civil Aviation Organization (ICAO) aviation safety standards for oversight of Thailand’s air carrier operations. Further information may be found on the FAA’s safety assessment page .
Maritime Travel: Mariners planning travel to Thailand should also check for U.S. maritime advisories and alerts . Information may also be posted to the U.S. Coast Guard homeport website , and the NGA broadcast warnings .
For additional travel information
- Enroll in the Smart Traveler Enrollment Program (STEP) to receive security messages and make it easier to locate you in an emergency.
- Call us in Washington, D.C. at 1-888-407-4747 (toll-free in the United States and Canada) or 1-202-501-4444 (from all other countries) from 8:00 a.m. to 8:00 p.m., Eastern Standard Time, Monday through Friday (except U.S. federal holidays).
- See the State Department’s travel website for the Worldwide Caution and Travel Advisories .
- Follow us on Twitter and Facebook .
- See traveling safely abroad for useful travel tips.
Review information about International Parental Child Abduction in Thailand . For additional IPCA-related information, please see the International Child Abduction Prevention and Return Act ( ICAPRA ) report.
Travel Advisory Levels
Assistance for u.s. citizens, thailand map, learn about your destination, enroll in step.

Subscribe to get up-to-date safety and security information and help us reach you in an emergency abroad.
Recommended Web Browsers: Microsoft Edge or Google Chrome.
Make two copies of all of your travel documents in case of emergency, and leave one with a trusted friend or relative.
Afghanistan
Antigua and Barbuda
Bonaire, Sint Eustatius, and Saba
Bosnia and Herzegovina
British Virgin Islands
Burkina Faso
Burma (Myanmar)
Cayman Islands
Central African Republic
Cote d Ivoire
Curaçao
Czech Republic
Democratic Republic of the Congo
Dominican Republic
El Salvador
Equatorial Guinea
Eswatini (Swaziland)
Falkland Islands
France (includes Monaco)
French Guiana
French Polynesia
French West Indies
Guadeloupe, Martinique, Saint Martin, and Saint Barthélemy (French West Indies)
Guinea-Bissau
Isle of Man
Israel, The West Bank and Gaza
Liechtenstein
Marshall Islands
Netherlands
New Caledonia
New Zealand
North Korea (Democratic People's Republic of Korea)
Papua New Guinea
Philippines
Republic of North Macedonia
Republic of the Congo
Saint Kitts and Nevis
Saint Lucia
Saint Vincent and the Grenadines
Sao Tome and Principe
Saudi Arabia
Sierra Leone
Sint Maarten
Solomon Islands
South Africa
South Korea
South Sudan
Switzerland
The Bahamas
Timor-Leste
Trinidad and Tobago
Turkmenistan
Turks and Caicos Islands
United Arab Emirates
United Kingdom
Vatican City (Holy See)
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Trop Med Hyg
- v.110(1); 2024 Jan
- PMC10793033

Malaria Stratification Mapping in Thailand to Support Prevention of Reestablishment
Donal bisanzio.
1 Inform Asia: USAID’s Health Research Program, RTI International, Bangkok, Thailand;
Prayuth Sudathip
2 Division of Vector Borne Diseases, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand;
Suravadee Kitchakarn
Jerdsuda kanjanasuwan, deyer gopinath.
3 World Health Organization, Nonthaburi, Thailand;
Niparueradee Pinyajeerapat
4 U.S. President’s Malaria Initiative, United States Agency for International Development (USAID), Regional Development Mission for Asia, Bangkok, Thailand
David Sintasath
Jui a. shah, associated data.
Thailand aims to eliminate malaria by 2026, with 46 of the country’s 77 provinces already verified as malaria free. However, these provinces remain susceptible to the reestablishment of indigenous transmission that would threaten the national goal. Thus, the country is prioritizing national and subnational prevention of reestablishment (POR) planning while considering the spatial heterogeneity of the remaining malaria caseload. To support POR efforts, a novel nonmodeling method produced a malaria stratification map at the tambon (subdistrict) level, incorporating malaria case data, demographic data, and environmental factors. The stratification analysis categorized 7,425 tambons into the following four risk strata: Local Transmission (2.9%), At Risk for Transmission (3.1%), High Risk for Reintroduction (2.9%), and Low Risk for Reintroduction (91.1%). The stratification map will support the national program to target malaria interventions in remaining hotspots and mitigate the risk of transmission in malaria-free areas.
INTRODUCTION
Thailand aims to eliminate malaria by 2026. Over the past decade, malaria incidence in the total population has significantly decreased, declining from 3.6 cases per 1,000 people in 2012 to 0.2 cases per 1,000 people in 2021. 1 This success in reducing malaria burden is due to intense intervention activities based on timely case investigation, case classification, and foci investigation. 2 During 2016, Thailand formally shifted from a control to an elimination program by adopting the National Malaria Elimination Strategy 2017–2026 3 and the 1-3-7 surveillance approach. 4
The WHO recommends that countries tailor interventions based on malaria stratification risk. 5 This approach allows countries with low malaria incidence to promote targeted interventions in remaining hotspots of autochthonous transmission. Thailand’s Division of Vector-Borne Diseases (DVBD) has a subnational verification of elimination program, which has documented and celebrated that 46 of the country’s 77 provinces are malaria free. The program builds on the WHO’s rigorous criteria for national certification. However, even malaria-free provinces remain vulnerable to the reintroduction of malaria parasites and the reestablishment of indigenous transmission, threatening national progress toward elimination. Thus, subnational prevention of re-establishment (POR) planning is an essential component of a malaria elimination program 6 to maintain the status of malaria-free areas while addressing remaining hotpots.
Malaria incidence in Thailand exhibits substantial heterogeneity, with malaria-free areas predominantly located in the central part of the country and remaining transmission areas along the borders with Cambodia, Myanmar, and Malaysia. 6 To account for this heterogeneity, the DVBD implements malaria strategies at a focus level, 7 necessitating a stratification approach to support targeted POR interventions with increased resolution. This study presents a novel method for performing malaria stratification mapping in Thailand by using routine malaria surveillance data and environmental information to support POR planning.
MATERIALS AND METHODS
The stratification followed the WHO’s guidelines 5 and used data at the tambon (subdistrict) level from fiscal years (FYs) 2019 through 2022. A list of receptivity and vulnerability variables was compiled during discussions with the DVBD and partners. The selected variables included those recorded in Thailand’s malaria information system (MIS) and other contextual variables that could affect malaria transmission dynamics. The variables described the number of reported malaria cases, population movement, demographic characteristics of reported cases, vector ecology, parasite characteristics, interventions, and environmental factors (a full list and data sources are reported in the supplemental materials). The stratification method accounted for the following national malaria foci classifications: active focus (A1), residual nonactive focus (A2), cleared but receptive focus (B1), or cleared but not receptive focus (B2) ( Supplemental Table 1 ). One tambon would have several foci, with varying classifications.
The methodology aimed to create a stratification map based on foci classification and receptivity, demographic factors, and environmental characteristics to identify areas by risk of malaria re-establishment. The unsupervised approach was based on principal component analysis (PCA). 8 The PCA estimates weights for each variable category based on its relationship with all other variables, rather than being chosen arbitrarily. 9 , 10 Investigating these correlations allows the PCA to condense multiple variables’ information into one score. 8 This statistical method is most frequently used in economics to group people into wealth categories by using their assets. 11
The PCA also included variable selection to identify only variables with high importance in classifying the tambons for malaria caseload and risk of re-establishment; variables also needed to cover all tambons within the study period (as described in the supplemental materials). In line with malaria stratification performed elsewhere, 9 , 10 tambons were grouped into four strata. This grouping results in a manageable number of intervention packages for the DVBD yet maintains an informative level of detail ( Supplemental Figure 1 ).
The PCA’s grouping performance was assessed using the Kruskal–Wallis test for statistically significant differences of the selected variables among the strata. 12 All statistical analyses were performed using the R programming language. 13 The stratification process was provided to the DVBD as an ad hoc statistical software created using Jamovi ( www.jamovi.org ), which is open-source.
Among Thailand’s 7,425 tambons, the stratification analysis assigned 216 (2.9%), 228 (3.1%), 216 (2.9%), and 6,765 (91.1%) tambons to Stratum 1, Stratum 2, Stratum 3, and Stratum 4, respectively. The results of the PCA showed good grouping performance, with the Kruskal–Wallis test showing that the values of the variables used were significantly different across strata ( P < 0.05).
Given the characteristics of the tambons in each stratum, the following labels were assigned to represent each stratum’s probability to report autochthonous cases:
- Stratum 1: Local Transmission
- Stratum 2: At Risk for Transmission
- Stratum 3: High Risk for Reintroduction
- Stratum 4: Low Risk for Reintroduction
Stratum 1: Local Transmission included tambons with the highest malaria caseload, with a median (MD) incidence equal to 2.7 malaria cases per 1,000 people (interquartile range [IQR]: 0.23–2.4 cases per 1,000 people) ( Table 1 ). Tambons in Stratum 4: Low Risk for Reintroduction had the lowest malaria incidence from FY 2019 to FY 2022 among all the strata (MD 0; IQR: 0–0). Tambons allocated in Stratum 2: At Risk for Transmission and Stratum 3: High Risk for Reintroduction had a median malaria incidence below the elimination threshold of 1 case per 1,000 people ( Table 1 ).
Characteristics of the tambons of each stratum created using the PCA approach
IQR = interquartile range; PCA = principal component analysis. The stratum population was equal to the population of tambons of the stratum. The estimated number of households was obtained by dividing the tambon population by the mean number of people per household (2.7 people per household). Based on data recorded from 2019 through 2022.
Tambons in Stratum 1: Local Transmission showed a higher mean percentage of A1 foci (MD 12.5%) compared with the other strata, in which the mean percentage of A1 foci was less than 1% ( Table 1 ). Stratum 1: Local Transmission also showed recent reporting of A1 foci, whereas most of the tambons in the other strata have not reported autochthonous transmission in at least 3 years ( Table 1 ). The fraction of cases caused by Plasmodium falciparum was higher in the tambons belonging to Stratum 1: Local Transmission compared with those in the other strata ( Table 1 ). Thai citizens and plantation workers represented more reported cases in Stratum 1: Local Transmission compared with other strata ( Table 1 ).
The spatial pattern of the strata showed that Stratum 1: Local Transmission is mostly aggregated at the borders with Myanmar, Malaysia, and Cambodia ( Figure 1 ). The analyses also identified the tambons in low endemic provinces classified as Stratum 1: Local Transmission and Stratum 2: At Risk for Transmission ( Figure 1 ). People living in Strata 1, 2, and 3 represented 1.1%, 1.2%, and 1.6% of Thailand’s population, respectively ( Table 1 ). Accounting for the mean number of household inhabitants, 282,125 households are located in the tambons assigned to Stratum 1: Local Transmission.

Malaria stratification map for Thailand using data from 2019 through 2022.
The stratification results captured the known high heterogeneity of local transmission risk, but at the tambon level to better support POR decision-making and interventions. The method showed good grouping performance to identify areas in which the tambons are still reporting autochthonous cases. Furthermore, the results highlight additional areas at high risk of malaria transmission despite not having recently reported autochthonous cases; this novel information will support meaningful POR planning.
The stratification analysis showed that all tambons that still have A1 foci belonged to Stratum 1: Local Transmission ( Table 2 ). A high fraction of foci in these tambons are classified as residual nonactive (A2) and because of the frequent transition of A2 foci to A1 classification, 14 there is high risk for local transmission to resume within tambons in Strata 1 and 2. These strata were mostly identified along international borders, following well-known patterns in the Greater Mekong Subregion. 7 High human mobility across these borders, a suitable environment, and limited access to must-reach populations continue to drive malaria transmission in these tambons. 4 , 15 , 16 To reduce the risk of outbreaks by imported cases in areas close to the western border, the DVBD implements malaria interventions tailored for mobile and migrant populations. 17 However, the persistence of transmission in border areas indicates a need for new strategies to interrupt transmission. 18
Distribution of 2022 malaria foci per malaria stratum
The results showed that 97.7% of Thailand’s population resides in Stratum 3: High Risk for Reintroduction and Stratum 4: Low Risk for Reintroduction. In these strata, local transmission has not been reported for more than 3 years and the DVBD is launching POR plans. However, tambons in Stratum 3: High Risk for Reintroduction have a higher fraction of cleared but receptive foci (B1, 19.9%) compared with those in Stratum 4: Low Risk for Reintroduction (6.4%). The presence of receptive foci in these malaria-free areas requires tailored POR planning, based on risk and available resources, to maintain Thailand’s current successes and to accelerate toward malaria elimination.
This study also aimed to build a stratification approach that could be easily adopted and maintained by the country as part of routine surveillance and strategic planning at both national and subnational levels. Compared with stratification approaches used elsewhere, 19 , 20 this approach has two substantial benefits. First, the approach highlights Thailand’s use of routine surveillance data, which supports country leadership and reduces reliance on imputed data. Second, the DVBD can learn the approach and maintain it with annual updates, as the epidemiology warrants. The stratification analysis and results were programmed into Jamovi and accompanied by sufficient training to support sustained use through the malaria elimination goal. Provincial teams will use the Jamovi outputs in POR plans outlining surveillance and response activities specific to importation and reestablishment risks.
Supplemental files
Supplemental materials.
Note: Supplemental material appears at www.ajtmh.org .
Malaria Information and Prophylaxis, by Country [L]
The information presented in this table is consistent 1 with the information in the CDC Health Information for International Travel (the “Yellow Book”).
1. Factors that affect local malaria transmission patterns can change rapidly and from year to year, such as local weather conditions, mosquito vector density, and prevalence of infection. Information in these tables is updated regularly. 2. Refers to P. falciparum malaria unless otherwise noted. 3. Estimates of malaria species are based on best available data from multiple sources. Where proportions are not available, the primary species and less common species are identified. 4. Several medications are available for chemoprophylaxis . When deciding which drug to use, consider specific itinerary, length of trip, cost of drug, previous adverse reactions to antimalarials, drug allergies, and current medical history. All travelers should seek medical attention in the event of fever during or after return from travel to areas with malaria. 5. Primaquine and tafenoquine can cause hemolytic anemia in persons with glucose-6-phosphate dehydrogenase (G6PD) deficiency. Before prescribing primaquine or tafenoquine, patients must be screened for G6PD deficiency using a quantitative test. 6. Mosquito avoidance includes applying topical mosquito repellant, sleeping under an insecticide treated bed net, and wearing protective clothing (e.g., long pants and socks, long sleeve shirt). For additional details on mosquito avoidance, see: https://www.cdc.gov/malaria/travelers/index.html 7. P. knowlesi is a malaria species with a simian host (macaque). Human cases have been reported from most countries in Southeast Asia and are associated with activities in forest or forest-fringe areas. This species of malaria has no known resistance to antimalarials.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Passports, travel and living abroad
- Travel abroad
- Foreign travel advice
Before you travel check that:
- your destination can provide the healthcare you may need
- you have appropriate travel insurance for local treatment or unexpected medical evacuation
This is particularly important if you have a health condition or are pregnant.
Emergency medical number
Dial 1669 and ask for an ambulance.
Contact your insurance or medical assistance company promptly if you’re referred to a medical facility for treatment.
Vaccinations and health risks
At least 8 weeks before your trip check:
- the latest information on vaccinations and health risks in TravelHealthPro’s Thailand guide
- where to get vaccines and whether you have to pay on the NHS travel vaccinations page
Health risks in Thailand include:
- dengue fever
See the ‘Other risks’ section of the TravelHealthPro Thailand guide for more on health risks .
To avoid mosquito-borne viruses, such as dengue fever and Zika virus, take steps to avoid being bitten by mosquitoes.
Air quality
There can be high levels of air pollution in large cities. This includes Bangkok and Chiang Mai, which are also affected by seasonal regional smoke haze from the burning of trees. The high pollution and particulate count sometimes reach dangerous levels. This may worsen bronchial, sinus or asthma conditions.
Check air quality levels for many cities on the World Air Quality Index website .
The legal status and regulation of some medicines prescribed or bought in the UK can be different in other countries.
Hospitals and pharmacies across Thailand will usually accept UK prescriptions. Brand name medication can often be more expensive than locally produced medication.
Medication sold on the street may not be genuine or may have been stolen. Taking medication without medical advice or a prescription can have serious health consequences.
Read best practice when travelling with medicines on TravelHealthPro . The NHS has information on whether you can take your medicine abroad .
Healthcare facilities in Thailand
FCDO has a list of English-speaking doctors in Thailand . All hospitals require guarantee of payment before treating patients. Make sure you have adequate health insurance.
Private hospitals in Thailand are of a high standard but can be expensive. Public hospitals and clinics do not always meet UK standards, particularly outside Bangkok.
COVID-19 healthcare in Thailand
Check the latest information on risk from COVID-19 risk for Thailand on TravelHealthPro .If you have severe symptoms, or any questions related to COVID-19, while in Thailand, call the Thai COVID-19 Hotline on 1422. There is more information on the PR Thai Government Facebook page .
Travel and mental health
Read FCDO guidance on travel and mental health . There is also mental health guidance on TravelHealthPro .
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
- Open access
- Published: 08 January 2024
Early warning systems for malaria outbreaks in Thailand: an anomaly detection approach
- Oraya Srimokla 1 ,
- Wirichada Pan-Ngum 2 , 3 ,
- Amnat Khamsiriwatchara 4 ,
- Chantana Padungtod 5 ,
- Rungrawee Tipmontree 5 ,
- Noppon Choosri 6 &
- Sompob Saralamba 2
Malaria Journal volume 23 , Article number: 11 ( 2024 ) Cite this article
1296 Accesses
6 Altmetric
Metrics details
Malaria continues to pose a significant health threat. Rapid identification of malaria infections and the deployment of active surveillance tools are crucial for achieving malaria elimination in regions where malaria is endemic, such as certain areas of Thailand. In this study, an anomaly detection system is introduced as an early warning mechanism for potential malaria outbreaks in countries like Thailand.
Unsupervised clustering-based, and time series-based anomaly detection algorithms are developed and compared to identify abnormal malaria activity in Thailand. Additionally, a user interface tailored for anomaly detection is designed, enabling the Thai malaria surveillance team to utilize these algorithms and visualize regions exhibiting unusual malaria patterns.
Nine distinct anomaly detection algorithms we developed. Their efficacy in pinpointing verified outbreaks was assessed using malaria case data from Thailand spanning 2012 to 2022. The historical average threshold-based anomaly detection method triggered three times fewer alerts, while correctly identifying the same number of verified outbreaks when compared to the current method used in Thailand. A limitation of this analysis is the small number of verified outbreaks; further consultation with the Division of Vector Borne Disease could help identify more verified outbreaks. The developed dashboard, designed specifically for anomaly detection, allows disease surveillance professionals to easily identify and visualize unusual malaria activity at a provincial level across Thailand.
An enhanced early warning system is proposed to bolster malaria elimination efforts for countries with a similar malaria profile to Thailand. The developed anomaly detection algorithms, after thorough comparison, have been optimized for integration with the current malaria surveillance infrastructure. An anomaly detection dashboard for Thailand is built and supports early detection of abnormal malaria activity. In summary, the proposed early warning system enhances the identification process for provinces at risk of outbreaks and offers easy integration with Thailand’s established malaria surveillance framework.
Malaria remains a life-threatening and preventable disease in many parts of the world [ 1 ]. While significant progress in reducing Thai malaria cases has occurred in the past two decades, continued efforts are necessary to achieve elimination [ 2 , 3 ]. The Operational Plan 2017–2021, aligned with Thailand’s National Malaria Elimination Strategy 2017–2026, emphasizes the need to enhance rapid identification of infections and implement timely and active surveillance and response measures to prevent further transmission [ 4 ]. The Division of Vector-Borne Disease (DVBD) leads the national malaria programme and is responsible for implementing surveillance initiatives in Thailand [ 3 ]. The DVBD, operating under the Department of Disease Control of the Ministry of Public Health, facilitated and oversees real-time aggregation of electronic malaria case data [ 4 , 5 ]. The electronic malaria information system (eMIS) was developed by the Center of Excellence for Biomedical and Public Health Informatics (BIOPHICS), Faculty of Tropical Medicine at Mahidol University aiming to replace paper-based malaria reporting with near-real-time electronic reporting [ 5 ]. BIOPHICS currently hosts all eMIS data, acting as the ongoing technical system support for the ministry [ 5 ].
With the development of eMIS, Thailand has conducted the 1-3-7 strategy to improve malaria elimination [ 6 ]. This strategy involves notifying each malaria case within 1 day of testing positive for malaria, classifying the case within 3 days, and completing a response within 7 days [ 6 ]. Responses involve case investigation and the deployment of appropriate interventions for vector control [ 4 ]. Depending on the case classification, interventions include blood sampling, distributing insecticide-treated bed nets, indoor residual spraying, and health education [ 4 ]. Seasonal malaria chemoprevention (SMC) has been used as preventative treatment in areas with seasonal transmission and require adaptable thresholds to define disease patterns over time and space. These thresholds are used as a surveillance method to identify suitable areas for SMC and require input from health districts as they are often challenging to define [ 7 ]. Overall, these methods require a broad workforce, high data quality, continued leadership, and are costly. To successfully eliminate malaria in Thailand, it is crucial to incorporate well supported community-based health workers and establish an affordable and efficient detection system. This system should quickly identify outbreaks in their early stages, be adaptable to various health districts’ needs, and reduce the malaria burden more rapidly in the remaining localized high transmission foci [ 8 ].
Early warning systems give advance warnings of impending epidemics and play a crucial role in the malaria surveillance program overseen by the DVBD [ 9 , 10 ]. Malaria outbreaks are defined as higher than usual malaria case activity in a specific area. Currently, the warning system relies on a 3 year median approach, where an alert is triggered if weekly malaria cases exceed the 3 year median of weekly cases from previous years and prompt investigation by the DVBD [ 11 ]. The publicly available online dashboard for the Thailand Malaria Elimination Programme ( https://malaria.ddc.moph.go.th/malariaR10/index_newversion.php ), provides information on provincial case counts, weekly case counts, 3 year median thresholds, and the implementation of the 1-3-7 strategy throughout Thailand. This tool provides general case visualization across Thailand, but it does not support identification of unusual malaria case activity across Thailand [ 11 ]. The development of improved early warning mechanisms and a robust dashboard is needed to optimize the response time and allocation of resources to areas with impending epidemics and to support effective implementation of preventive measures.
Anomaly detection is used to discover unexpected or rate events in data streams and can be applied to health data to identify outliers in a system [ 12 ]. Anomaly detection algorithms are dynamic and can include a combination of statistical and machine learning approaches and threshold-based methods that detect highly abnormal activities in the data. Examples of uses are fraud detection in insurance and banking, intrusion detection of computer networks, and medical informatics for disorder detection [ 12 ]. Three types of machine learning-based anomaly detection algorithms are supervised, unsupervised, and semi-supervised [ 12 ]. While no single anomaly detection method is universally effective, several approaches are suited for time series anomaly detection. These approaches include predictive confidence levels, statistical profiling, clustering, and density-based profiling [ 12 , 13 , 14 , 15 , 16 ]. Anomaly detection presents a promising approach in disease detection. Previous studies have explored the application of density-based anomaly detection algorithms to health data including heart disease, diabetes, and hepatitis [ 17 , 18 ].
Similarly, the use of unsupervised anomaly detection methods have been used to discover implausible electronic health records in cancer registries [ 19 ] and adverse health conditions for people living dementia using sensor-base data [ 20 ]. In a study exploring the use of unsupervised anomaly detection for disease surveillance, Brazilian Amazon malaria surveillance data is used as a case study for early detection of outbreaks [ 21 ]. As anomaly detection algorithms are a promising technique for early identification of abnormal malaria activity, the use of both unsupervised clustering and time series-based anomaly detection methods are explored for endemic malaria environments similar to Thailand. This study focuses on using anomaly detection algorithms as a method to strengthen malaria surveillance systems with Thailand as an example setting. The early detection of impending outbreaks can be integrated with the existing eMIS and enhance the current 1-3-7 strategy to effectively respond to any anomaly identification within 7 days using appropriate interventions [ 4 ].
The aim of this research is to propose an early detection system to support the malaria elimination programs in countries where malaria is endemic, similar to Thailand. Additionally, the aim is to improve methods for early detection of malaria in areas with impending outbreaks. To achieve these aims and using Thailand as an example setting, the main research objectives are:
Develop anomaly detection algorithms and early detection thresholds that are suitable for malaria data in Thailand.
Compare the developed algorithms to Thailand’s current early warning threshold.
Develop a prototype user interface for Thai public health professionals that supports early identification of outbreaks and enables focused attention on anomalous areas.
To support the objectives of this study, the methods are separated into five main sections: data, algorithms, algorithm comparison, code structure, and user interface.
The data for this analysis was provided by the Ministry of Public Health and used under a research protocol approved by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Bangkok. This study encompasses all 77 provinces of Thailand (see Additional file 1 ), a region characterized by its warm, humid tropical climate and seasonal monsoon winds [ 22 ]. Thailand has an annual cycle of wet and dry seasons with a concentration of rainfall during the wet season [ 23 ]. Thailand is located in Southeast Asia and is bordered by Myanmar in the west, Laos in the north, Cambodia in the east, and Malaysia in the south [ 24 ]. The data contains Thailand malaria cases reported daily from 2012 to 2022 for all Thai provinces with personal identifiers excluded from the analyses. The data contains 31 variables including the blood draw date, nationality, sex, age, province, province ID, subdistrict, species of malaria, border type, occupation, and treatment for 180256 observations of malaria cases. All province names are translated into English based on their provincial ID (details in Additional file 1 ). The data is transformed into incidence data based on the case counts per date and then grouped based on province for further analysis. Depending on the method, the case data was aggregated either daily, weekly, or monthly (see Additional file 11 for more information about aggregation interval for each method). Initial visualization of the data is shown (see Fig. 1 and Additional file 2 ) and can be further visualized in the analytics tab of the final dashboard: https://moru.shinyapps.io/Malaria_Anomaly_Detection_App/ .
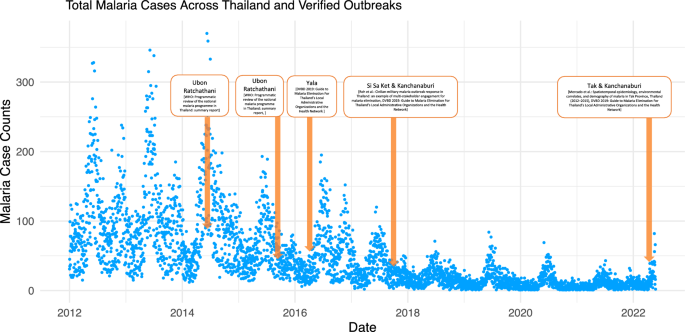
Total Malaria Cases Across Thailand from 2012 to 2022. The malaria case counts across Thailand are shown from 2012 to 2022. The verified outbreak dates, found in literature, are highlighted in orange and provide information on the province name and the reference used for each outbreak. These outbreak dates are used to compare and validate the anomaly detection algorithms presented in this paper
As climate and environmental factors could be one of the primary factors driving malaria transmission [ 25 , 26 , 27 ], daily precipitation and temperature data is incorporated in an unsupervised clustering method with daily malaria cases. From both the temperature and precipitation datasets, measurements from central Thailand are used for analysis on all provinces as the temperature and precipitation does not vary significantly across Thailand. The daily precipitation data for Thailand was extracted from Temperature and Precipitation Gridded Data for Global and Regional Domains Derived from In-situ and Satellite Observations from the Copernicus Climate Data Store [ 28 ]. Similarly, the daily temperature data for Thailand was extracted from the Berkeley Earth’s Global Temperature Gridded Data [ 29 ]. The daily precipitation and temperature data are added to the daily malaria incidence data frame based on date and scaled to be comparable to the malaria case data. The multivariate scaled data is then used as an input into density-based unsupervised clustering function DBSCAN. Unsupervised clustering approaches are further described below and in Additional file 11 .
Anomaly detection algorithms
Two main types of anomaly detection algorithms developed are clustering-based methods and time series-based methods. Each method will be used to identify anomalous or unusual malaria activity. The performance for each type of anomaly detection algorithm is compared in the following section. Table 1 shows the methods used for this analysis.
Unsupervised clustering approaches create measurements between different elements and cluster them base on their similarity without requiring training data [ 12 ]. Anomalous observations are labelled when they have a high distance to existing clusters or have a lower density when compare to other clusters [ 12 ]. Anomaly detection algorithms based on unsupervised clustering approaches include unsupervised time-series clustering, unsupervised density-base clustering with the malaria case data, and unsupervised density-based clustering with malaria case data, precipitation data, and temperature data (see Additional file 11 for detailed descriptions).
Time series-based anomaly detection approaches analyse the data based on a sliding window and at a specified time frame. These methods are able capture the change in malaria cases for an evolving time series and can involve the comparison of cumulative cases, mean cases, and standard deviation along the time series. Time series-based anomaly detection algorithms include statistical profiling, predictive confidence interval, weekly and monthly malaria case comparisons, rolling historical averages, and weekly 3 year median case comparisons (see Additional file 11 for detailed descriptions).
As an initial test, early detection methods are applied and visualized at a provincial level to see if unusual case activity can be identified using this dataset. All methods can be selected in the dropdown menu in the analytics tab of the final dashboard ( https://moru.shinyapps.io/Malaria_Anomaly_Detection_App/ ) and are grouped by clustering-based (orange) and time series-based (blue) (see Fig. 3 ).
Algorithm validation and comparison
To validate the algorithms, additional literature review, the online Thailand Malaria Elimination Program tool, and consultation with BIOPHICS provided information on dates and provinces where malaria outbreaks were previously reported. To match available malaria data, outbreaks reported from 2012 to 2022 were selected. The two main goals for the validation stage are to identify the number of outbreaks caught for each method up to two weeks prior to the verified outbreak date, and the number of alerts triggered by each method.
From literature, the Thailand Malaria Elimination Program online tool, and consultation with BIOPHICS, 7 outbreak dates were identified. 6 of the 7 outbreaks were reported at a provincial level while 1 (2017 Kanchanaburi) was reported at a subdistrict level. Reported outbreaks are generally clustered along provinces bordering Laos, Cambodia, and Myanmar and could have resulted from factors like migrant movement, limited access to malaria prevention and diagnostics, inadequate monitoring measures, dense forest regions, and political and social unrest [ 30 ]. The summary of outbreak dates are shown in Table 2 (see Additional file 12 for detailed descriptions).
All anomaly detection methods are run through all the provinces. Each province and method were assessed to determine if it could generate warnings within a two-week window leading up to the outbreak date. The exact outbreak date, shown as a peak in cases, is found using the Thailand Malaria Elimination Programme online tool and compared to estimates reported in literature. The function summed the total real outbreak dates each method caught and the total number of alerts each method produced. The pseudocode for validating and comparing various anomaly detection methods can be found in Additional file 13 and the final result from testing is shown in the analytics tab of the final dashboard.
In addition to reporting verified outbreaks, the total number of alerts reported from each method are also tracked. Each anomaly detection method is applied to all the malaria data from 2012 to 2022 and reports the number of anomalies or alerts each method triggers. The purpose of tracking these alerts is to ensure that the method used for anomaly detection is not highly sensitive to every irregularity found in the case data and reporting is done for only highly anomalous activity.
Code structure
The code is structured to conduct anomaly analysis at a provincial level, with a user-defined method, time frame, and malaria species (see Additional file 10 ). The data is converted into incidence data based on the resolution of analysis and grouped at a provincial level. The resolution of analysis can be increased to smaller regions; however, this will be more computationally intensive as increasing the resolution to the subdistrict level will take 45 times as long to run. After the user-specified method is applied to each province, the daily anomalous activity is reported for the time frame defined and stored in an outer data frame. The final activity data frame is used for further analysis and is connected to visualizations in the user interface in the form of a map highlighting anomalous provinces.
The user interface is designed for the DVBD surveillance team with consultation through BIOPHICS. For easy visualization and prototyping, a wireframe of the inter-face was developed using Canva [ 31 ]. An R Shiny application was developed to test and debug functions, integrating visualization tools like raster, rworldmap, and ggplot to highlight anomalous activities [ 32 , 33 , 34 , 35 ].
The final application was created using R Shiny and bs4Dash and has three main pages [ 36 ]. The first page describes the project and the algorithms available for analysis. The second page provides a weekly summary, including information on provinces with detected anomalies. The third page allows the user to conduct further analysis by inputting the time frame, method, and species of malaria used for analysis. Two main visualizations are updated every time a new analysis is initiated: one highlighting provinces with anomalies detected and another showing the standardized incidence ratio of malaria incidence across Thailand. Additional information such as trend lines, percentage of provinces with anomalies detected, and names of provinces with unusual activity are also included.
Algorithm development and validation
A total of 9 anomaly detection algorithms were created and initially tested and visualized to confirm correctly implemented alerts were produced for observations exceeding thresholds or bands defining anomalous activity for the Tak province (see Fig. 2 and Additional file 3 ). From this initial test, anomalous observations are distinguished from normal malaria case activity.
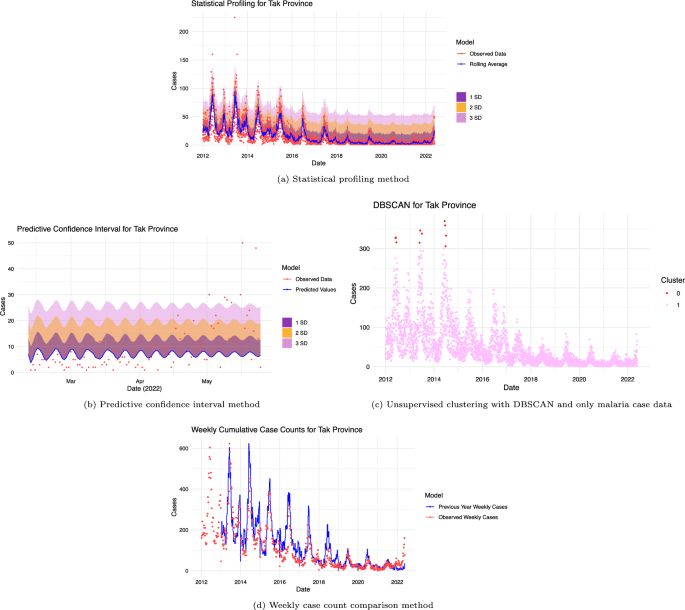
Visual results from testing algorithms with the Tak Province. Anomaly detection algorithms tested with Tak provincial malaria data from 2012 to 2022. a the statistical profiling method shows 3 standard deviation bands. Observations falling outside the 3 standard deviation bands are classified as anomalous. b the predictive confidence interval method is used to create 3 standard deviation bands from the mean standard error. Observations falling outside the 3 standard deviation band are classified as anomalous. c the unsupervised method using DBSCAN is used to cluster observations. Observations in cluster 0 (smallest cluster) are defined as anomalous while observations in cluster 1 are not. d the weekly cumulative case comparison method is used to compare observations. Weeks where cumulative cases are higher than the previous year’s weekly cases (blue) are classified as anomalous
After developing and validating the anomaly detection algorithms in the Tak province, tested each method was tested across all provinces to evaluate their effectiveness in identifying confirmed outbreaks. These results are shown in Table 3 . In this table, the ✘ symbol shows that the method used did not trigger anomalous alerts at least two weeks before the verified outbreak and the ✔ symbol shows that the method used triggered anomalous alerts at least two weeks before this verified outbreak. The sensitivity for each method is calculated by taking the number of verified outbreaks found over the total number of verified outbreaks. In the analysis using time-series methods, varying levels of sensitivity was observed. Specifically, for the monthly case comparison, statistical profiling, and predictive confidence interval methods, the sensitivities were 0/7, 1/7, and 3/7, respectively. In contrast, the historical average, weekly case comparison, and weekly 3 year median methods demonstrated a higher sensitivity, each achieving a rate of 6/7. However, for the clustering-based methods, the sensitivity was consistently found to be 0/7. The highest number of verified anomalies found was 6 out of the 7. Methods able to identify 6 outbreaks were historical average, weekly case counts, and the weekly 3 year median method. Of these three methods, the historical average method produced the lowest number of alerts (see Additional file 4 for visualizations of true anomalies caught using the historical average and DBSCAN method applied to Ubon Ratchathani). Of the 9 methods, 4 methods were unable to identify the labelled outbreaks. These methods are density-based profiling with DBSCAN, density-based profiling with DBSCAN including temperature and precipitation data, unsupervised clustering with tsclust [ 37 ], and monthly case comparison. The method reporting the most alerts at 32630 is the weekly 3 year median while the method reporting the lowest number of alerts at 5 is density-based profiling with DBSCAN.
Code structure and functionalization
After the algorithms’ performance were tested, they were converted into functions with easily adaptable outbreak definitions. Data handling and filtering functions are created to allow user input into the analysis. Additional functions were created to run anomaly detection algorithms across all provinces based on user-defined inputs, such as malaria species and time period for analysis, and to store the anomaly status of each province for map visualization. The code structure (see Fig. 2 ) was achieved. All the code files can also be found here: https://github.com/mghDissertation/malaria_anomaly_detect .
User interface
To aid in developing the optimal design and layout for the final dashboard, a wireframe was developed (refer to Additional file 5 ), specifically tailored for anomaly detection. An intermediate application (refer to Additional file 5 ) was used to validate code functionality, offering a visual depiction of provinces marked for unusual malaria activity. The dashboard’s design was refined based on feedback from BIOPHICS and fellow researchers, ensuring effective anomaly detection and granting users the flexibility to choose essential parameters. The final dashboard contains three main pages with information on methods, generated visuals, and method-specific accuracy. The aim is to allow users to easily compare different methods, species, and time frames used for analysis. The final dashboard, as shown in Fig. 3 and Additional file 5 , will feature the best method on its summary page for DVBD’s use. The final application is hosted here: https://moru.shinyapps.io/Malaria_Anomaly_Detection_App/ .
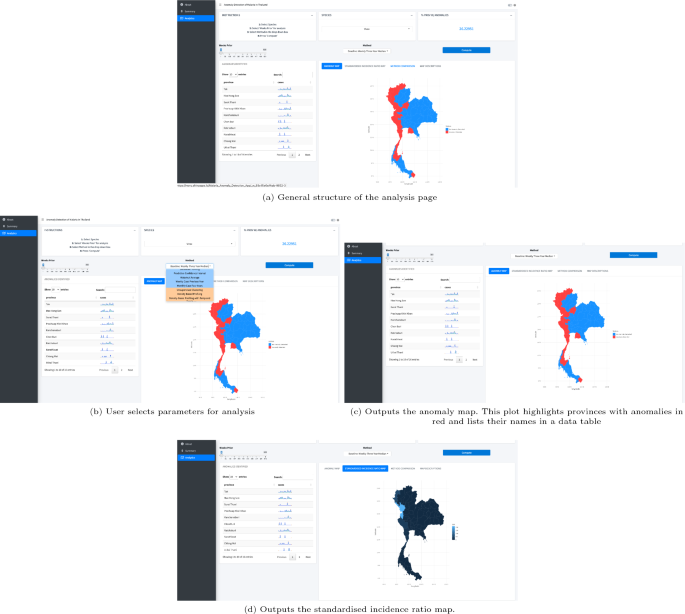
Final user interface. Output from the “Analytics” tab showing maps, anomalous province names, and case trends in the application https://moru.shinyapps.io/Malaria_Anomaly_Detection_App/ . The user selects the species, method, and time period of interest to run the analysis. The methods are grouped by machine-learning-based (orange) and threshold or statistical-based (blue). After the investigation is complete, the anomaly map, the standardized incidence ratio map, and the anomalous provincial names are shown. Additional map descriptions are shown in the map descriptions tab
The creation of effective anomaly detection algorithms combined with a user inter-face tailored for anomaly detection supports progress towards the Thailand Malaria Elimination Programme.
Through the evaluation of algorithms, it was found that three methods—historical average, weekly case comparison, and weekly 3 year median—successfully identified 86% of the labeled outbreaks. However, these methods varied significantly in their alert efficiency, with the total number of alerts generated to verified anomalies detected being 1813, 5075, and 5438, respectively. As observed in Table 3 , these three methods detected 6 out of 7 outbreaks. The historical average method was able to detect all verified outbreak dates except for the 2014 Ubon Rachathani outbreak. Given that the dataset begins in 2012 and the historical average method requires data from the previous 3 years, the alert threshold value might have been set higher than intended, preventing the alert from being triggered. In contrast, the weekly case comparison method identified all verified outbreaks except for the 2015 Ubon Ratchathani observation. The weekly case comparison method relies on the weekly cumulative counts from the previous year and because an outbreak was reported in Ubon Ratchathani from the previous year, a slight decrease in case values would not have been able to trigger an alert for this method even if an outbreak was declared. Similarly, the 3 year median method identified all outbreaks except for the one in Kanchanaburi in 2017. Since this outbreak was reported at a subdistrict level, it was more difficult to catch these irregularities when the analysis was completed at a provincial level. Other methods that failed to detect this subdistrict outbreak include statistical profiling, predictive confidence interval, unsupervised clustering with tsclust package [ 37 ], density-based profiling using only case data, density-based profiling combining case data with temperature and precipitation data, and monthly case comparison. Although the currently implemented 3 year median method identified 6 out of 7 actual outbreaks, it generated approximately three times as many predictions (or total reported alerts) compared to the historical average method. The primary objective of these algorithms is to guide the DVBD on which areas to prioritize, especially in resource-limited scenarios, to pre-emptively control potential outbreaks. In practice, a low false positive rate combined with a high true positive rate is crucial for DVBD to effectively respond to outbreaks.
The statistical profiling method detected 14.2% of the labelled outbreaks, while the predictive confidence interval method detected 43%. Despite having fewer alerts, the statistical profiling and predictive confidence interval methods reported a ratio of the total number of alerts generated to verified anomalies detected of 882 and 785. For instance, the statistical profiling method identified anomalies solely for the 2016 Yala outbreak. In contrast, the predictive confidence interval method detected the 2016 Yala outbreak and also the 2017 Si Sa Ket and 2014 Ubon Ratchathani outbreaks. By collaborating further with the DVBD, acceptable false positive rates and sensitivity levels can be determined. This will help in refining the customization of warning methods for specific health districts. In the context of clustering-based methods, this analysis found that techniques such as clustering with tsclust [ 37 ] and DBSCAN using malaria case data were ineffective in identifying any labelled outbreak data. This was also the case when combining malaria case data with precipitation and temperature metrics. While these methods were tested at a provincial level, their outcomes might vary when implemented at district or village levels.
Compared to time series-based methods, clustering-based anomaly detection methods showed lower accuracy in identifying verified outbreaks when tested with malaria data from 2012 to 2022. Table 3 shows how different methods were able to capture different anomalous activities.
Through further visualization of these methods applied to the Kanchanaburi province (Additional file 14 ) it becomes evident why some methods are able to capture more anomalies than others. The historical average and statistical profiling use daily malaria cases for analysis and can capture seasonal changes in malaria cases more than the predictive confidence interval method. The statistical profiling method was only able to capture one verified anomaly since the threshold use to classify anomalous observations was much higher than other methods using daily malaria cases. As a result, less anomalies are reported, and fewer verified outbreaks are caught. Compared to the statistical profiling method and the predictive confidence interval method, the historical average method has a lower threshold that outlines the general shape of the daily cases and as a result, more anomalies are reported, and more verified outbreaks are caught early. This is similarly observed in the weekly case comparison and weekly 3 year median methods. These two methods use weekly malaria cases and can capture malaria seasonality while creating a threshold which is high enough that not all observations are anomalous, but low enough to capture weeks with higher than usual malaria cases. As a result, these two methods had a better performance than other methods. Similar to the statistical profiling method, the monthly case comparison method is capable of identifying seasonal malaria trends. However, its threshold is significantly higher than the observed data, attributable to the elevated averages of malaria cases from the preceding 4 years. As a result, the monthly case comparison method captured few anomalies and was not able to capture any of the verified outbreaks. Figure 2 shows that clustering-based methods defined observations at large malaria peaks as anomalous. These methods were not able to capture anomalies between peaks and for smaller malaria waves that preceded larger ones.
A combination of these methods can be used to capture different types of anomalies across countries with a similar malaria profile to Thailand and should be tested with more verified outbreak dates. In this context, the historical average method outperformed others due to its high accuracy in identifying outbreaks and its low false positive rate. Observations deemed anomalous are categorized based on threshold definitions. These thresholds can be adjusted to match the tolerance levels set by health districts, comparable to the criteria used for SMC area identification. Depending on the application and scenario, tailored algorithm thresholds can be designed based on health district needs. Easy integration is possible as all methods and code are functionalized and adaptable to requirements set by different health districts.
The final dashboard, tailored specifically for anomaly detection, has been designed to be user-friendly, allowing disease surveillance professionals to easily navigate and interact with the detection algorithms. It offers tools for visualizing anomalies and user-defined analysis parameters, and it facilitates in-depth analysis of atypical patterns in malaria data.
The dashboard application has three main pages. The ‘Introduction’ page presents the application’s objectives and methodologies. The ‘Summary’ page provides weekly insights on anomalous provinces and malaria cases, categorized by border types, based on a default method determined by the health district.
The analysis page allows users to expand their analysis through user-defined methods, malaria species, and time frames. Its core aim is to showcase how different methods and time frames affect provincial alerts. Method options are grouped into clustering-based (orange) or time series-based (blue) in a dropdown methods section in the analysis page of the dashboard.
The analysis page provides step-by-step guidance, highlighting anomalous provinces on a map and showing standardized malaria incidence across Thailand. After each analysis, anomalous provinces are listed, and an interactive widget displays malaria cases over time per province.
Limitations
Certain limitations were present in this study. Specific statistical methods relied on literature to classify anomalies as values surpassing 3 standard deviations above the mean. As each province follows its own protocol for defining malaria out-breaks and resource allocation, collaborating with different health districts to establish outbreak thresholds is essential to identify the most suitable method for them. This cooperative approach, combined with user feedback for both the algorithms and user interface, can help identify the most suitable anomaly detection method for each province. For the dataset used, observations started in 2012 and ended in May 2022, and lacks real-time integration with the malaria reporting database. Although functions are compatible with raw data, real-time integration should be conducted. While this analysis focused developing a proof-of-concept on a provincial level for efficiency, it could be extended to subdistrict or subvillage scales to represent the surveillance resolution implemented in the 1-3-7 program. More outbreak data points and working directly with the DVBD surveillance team would improve validation, algorithm sensitivity, and the final interface.
Conclusions
An enhanced early warning system is proposed to bolster malaria elimination efforts in regions where malaria is endemic, such as certain areas of Thailand. Clustering-based and time series-based methods were developed and compared. Compared to the current method analysing malaria case data from 2012 to 2022, the historical average-based method demonstrated equivalent sensitivity with a reduced false positive rate. A user interface tailored for anomaly detection is developed and aids in early detection by summarizing anomalies on a weekly basis across provinces. The code has been optimized for functionality and is configured to synchronize with the real-time malaria database. The anomaly detection algorithms could be integrated at the case identification stage of the 1-3-7 protocol and applied at a sub village level. This approach would assist in determining the allocation of resources to prevent the spread of atypical malaria cases. The proposed early warning system enhances the timely identification of provinces at risk of epidemics and seamlessly integrates with Thailand’s malaria surveillance system.
Availability of data and materials
The Thai malaria data is not publishable, however, a summary of the data is found in Additional file 2 . Additional file 6 outlines the outbreak dates used for the method comparison section. The daily precipitation data can be downloaded from the Temperature and Precipitation Gridded Data for Global and Regional Domains Derived from In-situ and Satellite Observations from the Copernicus Climate Data Store ( https://cds.climate.copernicus.eu/cdsapp#!/dataset/insitu-gridded-observations-global-and-regional?tab=overview ) and the daily temperature data can be downloaded from Berkeley Earth’s Global Temperature Gridded Data ( https://berkeleyearth.org/data/ ). The precipitation and temperature data is visualized in Additional file 2 . Additional file 7 and 8 shows the precipitation and temperature data used for this report. The provincial population data is available through the National Statistical Office ( http://statbbi.nso.go.th/staticreport/page/sector/en/01.aspx ) (details in Additional file 9 ).
Code availability
The code is available on Github at ( https://github.com/mghDissertation/malaria_anomaly_detect ).
Abbreviations
Division of Vector Borne Disease
Electronic Malaria Information System
Center of Excellence for Biomedical and Public Health Informatics
Density-Based Spatial Clustering of Applications with Noise
World Health Organization
Seasonal Malaria Chemoprevention
Autoregressive Integrated Moving Average
WHO. Fact sheet about malaria. Geneva: World Health Organization; 2023.
Google Scholar
Chareonviriyaphap T, Bangs MS, Ratanatham S. Status of malaria in Thailand. Southeast Asian J Trop Med Public Health. 2000;31:225–37.
CAS PubMed Google Scholar
WHO. Thailand gears up to eliminate malaria by 2024. Geneva: World Health Organization; 2023.
Lertpiriyasuwat C, Sudathip P, Kitchakarn S, Areechokchai D, Naowarat S, Shah JA, et al. Implementation and success factors from Thailand’s 1-3-7 surveillance strategy for malaria elimination. Malar J. 2021;20:201.
Article PubMed PubMed Central Google Scholar
Ma S, Lawpoolsri S, Soonthornworasiri N, Khamsiriwatchara A, Jandee K, Taweeseneepitch K, et al. Effectiveness of implementation of electronic malaria information system as the national malaria surveillance system in Thailand. JMIR Public Health Surveill. 2016;2:e20.
Shah JA. Learnings from Thailand in building strong surveillance for malaria elimination. Nat Commun. 2022;13:2677.
Article CAS PubMed PubMed Central Google Scholar
Jongdeepaisal M, Khonputsa P, Prasert O, Maneenet S, Pongsoipetch K, Jatapai A, et al. Forest malaria and prospects for anti-malarial chemoprophylaxis among forest goers: findings from a qualitative study in Thailand. Malar J. 2022;21:47.
Smithuis FM, White NJ. Spend wisely to eliminate malaria. Lancet Infect Dis. 2022;22:e171–5.
Article PubMed Google Scholar
Maharaj R. Early warning systems for the detection of malaria outbreaks. Indian J Med Res. 2017;146:560–2.
PubMed PubMed Central Google Scholar
Konchom S, Singhasivanon P, Kaewkungwal J, Chuprapawan S, Thimasarn K, Kidson C, et al. Early detection of malaria in an endemic area: model development. Southeast Asian J Trop Med Public Health. 2006;37:1067–71.
PubMed Google Scholar
Thailand Malaria Elimination Programme. https://malaria.ddc.moph.go.th/malariar10/index_newversion.php
Schneider P, Xhafa F. Anomaly detection and complex event processing over IoT data streams. Cambridge: Academic Press; 2022.
Pang J, Liu D, Peng Y, Peng X. Optimize the coverage probability of prediction interval for anomaly detection of sensor-based monitoring series. Sensors. 2018;18:967.
Salik JFN. Sub-band anomaly detection and spatial localization. In: 2007 IEEE Northeast Workshop on Circuits and Systems. 2007
Syarif I, Prugel-Bennett A, Wills G. Unsupervised clustering approach for network anomaly detection. In: Benlamri R, editor. Networked digital technologies. Berlin, Heidelberg: Springer; 2012. p. 135–45.
Chapter Google Scholar
Thang TM, Kim J. The anomaly detection by using DBSCAN clustering with multiple parameters. In: International Conference on Information Science and Applications. 2011.
Samariya D, Ma J, Aryal S, Zhao X. Detection and explanation of anomalies in healthcare data. Health Inf Sci Syst. 2023;11:20.
Nanehkaran YA, Licai Z, Chen J, Jamel AAM, Shengnan Z, Navaei YD, et al. Anomaly detection in heart disease using a density-based unsupervised approach. Wireless Commun Mobile Comput. 2022;2022:e6913043.
Article Google Scholar
Röchner P, Rothlauf F. Unsupervised anomaly detection of implausible electronic health records: a real-world evaluation in cancer registries. BMC Med Res Methodol. 2023;23:125.
Bijlani N, Nilforooshan R, Kouchaki S. An unsupervised data-driven anomaly detection approach for adverse health conditions in people living with dementia: cohort study. JMIR Aging. 2022;5:e38211.
Eze PU, Geard N, Mueller I, Chades I. Anomaly detection in endemic disease surveillance data using machine learning techniques. Healthcare. 2023;11:1896.
Thailand - Climatology. Climate Change Knowledge Portal. https://climateknowledgeportal.worldbank.org/country/thailand/climate-data-historical
Kiguchi M, Takata K, Hanasaki N, Archevarahuprok B, Champathong A, Ikoma E, et al. A review of climate-change impact and adaptation studies for the water sector in Thailand. Environ Res Lett. 2021;16:023004.
World Bank Climate Change Knowledge Portal- Thailand. https://climateknowledgeportal.worldbank.org/country/thailand
Dabaro D, Birhanu Z, Negash A, Hawaria D, Yewhalaw D. Effects of rainfall, temperature and topography on malaria incidence in elimination targeted district of Ethiopia. Malar J. 2021;20:104.
Oheneba-Dornyo TV, Amuzu S, Maccagnan A, Taylor T. Estimating the impact of temperature and rainfall on malaria incidence in Ghana from 2012 to 2017. Environ Model Assess. 2022;27:473–89.
Tiu LA, Wahid WE, Andriani WY, Mirnawati M, Tosepu R. Literature review: impact of temperature and rainfall on incident malaria. IOPSci Conf Ser. 2021. https://doi.org/10.1088/1755-1315/755/1/012084/meta .
Copernicus Climate Change Service. Temperature and precipitation gridded data for global and regional domains derived from in-situ and satellite observations. ECMWF. 2021. https://doi.org/10.2438/cds.11dedf0c .
Berkeley Earth. Environmental science, data, and analysis of the highest qualityIndependent, non-governmental, and open-source. https://berkeleyearth.org/
Ammatawiyanon L, Tongkumchum P, Lim A, McNeil D. Modelling malaria in southernmost provinces of Thailand: a two-step process for analysis of highly right-skewed data with a large proportion of zeros. Malar J. 2022;21:334.
Canva. Canva. https://www.canva.com/
Chang W. Shiny. https://www.rdocumentation.org/packages/shiny/versions/1.7.4.1
raster. https://cran.r-project.org/web/packages/raster/index.html
South A. rworldmap. https://github.com/AndySouth/rworldmap/
ggplot2. https://cran.r-project.org/web/packages/ggplot2/index.html
Granjon D. bs4Dash. https://rinterface.github.io/bs4Dash/index.html
Montero P, Vilar J. TSclust: an R package for time series clustering. J Stat Softw. 2014;62:1–43.
Mullineaux DR, Irwin G. Error and anomaly detection for intra-participant time-series data. Int Biomech. 2017;4:28–35.
Article PubMed Central Google Scholar
Nekorchuk DM, Gebrehiwot T, Lake M, Awoke W, Mihretie A, Wimberly MC. Comparing malaria early detection methods in a declining transmission setting in northwestern Ethiopia. BMC Public Health. 2021;21:788.
Hay SI, Simba M, Busolo M, Noor AM, Guyatt HL, Ochola SA, et al. Defining and detecting malaria epidemics in the highlands of Western Kenya. Emerg Infect Dis. 2002;8:555–62.
Cullen JR, Chitprarop U, Doberstyn EB, Sombatwattanangkul K. An epidemiological early warning system for malaria control in northern Thailand. Bull World Health Organ. 1984;62:107–14.
CAS PubMed PubMed Central Google Scholar
Kulanuwat L, Chantrapornchai C, Maleewong M, Wongchaisuwat P, Wimala S, Sarinnapakorn K, et al. Anomaly detection using a sliding window technique and data imputation with machine learning for hydrological time series. Water. 2021;13:1862.
Kozitsin V, Katser I, Lakontsev D. Online forecasting and anomaly detection based on the ARIMA model. Appl Sci. 2021;11:3194.
Article CAS Google Scholar
Ye F, Liu Z, Liu Q, Wang Z. Hydrologic time series anomaly detection based on Flink. Math Probl Eng. 2020;2020:e3187697.
Xue S, Chen H, Zheng X. Detection and quantification of anomalies in communication networks based on LSTM-ARIMA combined model. Int J Mach Learn Cyber. 2022;13:3159–72.
Sahu RT, Verma MK, Ahmad I. Density-based spatial clustering of application with noise approach for regionalisation and its effect on hierarchical clustering. Int J Hydrol Sci Technol. 2023;16:240–69.
Hahsler M. dbscan: density-based spatial clustering of applications with noise (DBSCAN) and related algorithms. https://cran.r-project.org/web/packages/dbscan/index.html
Roh M, Lausatianragit K, Chaitaveep N, Jongsakul K, Sudathip P, Raseebut C, et al. Civilian-military malaria outbreak response in Thailand: an example of multi-stakeholder engagement for malaria elimination. Malar J. 2021;20:458.
WHO. Programmatic review of the national malaria programme in Thailand: summary report. WHO Regional Office for South-East Asia; 2016. https://apps.who.int/iris/handle/10665/253958
Guide to Malaria Elimination For Thailand’s Local Administrative Organizations and the Health Network. Bureau of Vector Borne Diseases, Department of Disease Control, Ministry of Public Health
Mercado CEG, Lawpoolsri S, Sudathip P, Kaewkungwal J, Khamsiriwatchara A, Pan-ngum W, et al. Spatiotemporal epidemiology, environmental correlates, and demography of malaria in Tak Province, Thailand (2012–2015). Malar J. 2019;18:240.
Download references
Acknowledgements
I would like to express my gratitude to everyone who contributed to the completion of this research. I am extremely grateful to my supervisors (Dr. Sompob Saralamba, Dr. Wirichada Pan-Ngum, and Dr. Noppon Choosri), for their support, feedback, and mentorship throughout this project. I would also like to thank my current supervisor Dr. Ricardo Aguas for his guidance and feedback for this project. Lastly, I would like to thank all my collaborators for their input and suggestions throughout the research process.
This research was funded in part by the Wellcome Trust (Grant number 220211). For the purposes of open access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and affiliations.
Nuffield Department of Medicine, University of Oxford, Broad St, Oxford, OX13AZ, UK
Oraya Srimokla
Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Ratchawithi Rd, Bangkok, 10400, Thailand
Wirichada Pan-Ngum & Sompob Saralamba
Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Ratchawithi Rd, Bangkok, 10400, Thailand
Wirichada Pan-Ngum
Center of Excellence for Biomedical and Public Health Informatics, Faculty of Tropical Medicine, Mahidol University, Ratchawithi Rd, Bangkok, 10400, Thailand
Amnat Khamsiriwatchara
Division of Vector Borne Diseases, Department of Disease Control, Ministry of Public Health, Talat Kwan, Bangkok, Nonthaburi, 11000, Thailand
Chantana Padungtod & Rungrawee Tipmontree
College of Arts, Media and Technology, Chiang Mai University, Sukhothai 5 Alley, Mueang Chiang Mai, Chiang Mai, 50200, Thailand
Noppon Choosri
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: OS, WPN, SS. Formal Analysis: OS. Software: OS. Visualization: OS. Data Curation: OS, WPN, AK. Methodology: OS, SS. Validation: OS, WPN, AK. Writing and Editing: OS, WPN, SS. All authors reviewed the manuscript.
Corresponding author
Correspondence to Sompob Saralamba .
Ethics declarations
Ethics approval and consent to participate.
This study was based on aggregate P. vivax surveillance data in Thailand, provided by the Ministry of Health. No confidential information was included because mathematical analyses were performed at the aggregate level. All methods were performed under a research protocol approved by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Bangkok (reference TMEC 22–056).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
List of Provinces in Thailand.
Additional file 2:
Summary of Malaria Case, Temperature, and Precipitation Data.
Additional file 3:
Monthly Case Comparison Methods.
Additional file 4:
Algorithm Validation Example with the Ubon Ratchathani Province.
Additional file 5:
Interface Development: Wireframe, Intermediate Application, and Final Application.
Additional file 6:
List of the confirmed outbreaks.
Additional file 7:
The precipitation data.

Additional file 8:
The temperature data.
Additional file 9:
The provincial population data.
Additional file 10:
A High-Level Overview of the Code Structure.
Additional file 11:
Details of Anomaly Detection Methods Used for Analysis.
Additional file 12:
Detailed Descriptions of Verified Outbreaks.
Additional file 13:
The pseudocode for validating and comparing various anomaly detection methods.
Additional file 14:
Visualisation of Thresholds for Time Series Methods.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Srimokla, O., Pan-Ngum, W., Khamsiriwatchara, A. et al. Early warning systems for malaria outbreaks in Thailand: an anomaly detection approach. Malar J 23 , 11 (2024). https://doi.org/10.1186/s12936-024-04837-x
Download citation
Received : 09 October 2023
Accepted : 03 January 2024
Published : 08 January 2024
DOI : https://doi.org/10.1186/s12936-024-04837-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early detection
- Anomaly detection
Malaria Journal
ISSN: 1475-2875
- Submission enquiries: [email protected]
- Skip to main content
- Skip to "About this site"
Language selection
Search travel.gc.ca.
Help us to improve our website. Take our survey !
COVID-19: travel health notice for all travellers
Thailand travel advice
Latest updates: Health – editorial update
Last updated: April 2, 2024 07:28 ET
On this page
Safety and security, entry and exit requirements, laws and culture, natural disasters and climate, thailand - exercise a high degree of caution.
Exercise a high degree of caution in Thailand due to ongoing political tensions and sporadic demonstrations in Bangkok and elsewhere in the country.
Southern provinces of Narathiwat, Pattani, Songkhla and Yala - Avoid all travel
Back to top
Southern provinces of Narathiwat, Pattani, Songkhla and Yala
Separatist insurgents periodically perpetrate criminally and politically motivated attacks in the southernmost provinces of Narathiwat, Pattani, Songkhla and Yala.
These deadly attacks include shootings, bombings and arson, and are usually directed at military, government and security buildings and personnel. They have also occurred in a variety of public places.
Martial law and heavily enhanced security measures are in place in Narathiwat, Pattani, Yala, and Sadao District in Songkhla.
Increased enforcement powers allow authorities to:
- detain suspects without charge
- conduct searches
- seize objects or documents
- impose curfews
You risk becoming a collateral victim of an attack if you travel in these provinces.
Myanmar border areas in the provinces of Mae Hong Son and Tak
Exercise a high degree of caution when travelling to the Thailand–Myanmar border areas in the provinces of Mae Hong Son and Tak.
Occasional violence, banditry and clashes between government forces and drug traffickers occur.
Border crossing points may be closed without notice. Cross at designated border crossing points only, with the required travel documentation.
Preah Vihear Temple area and surrounding border region
Thailand and Cambodia have an ongoing border dispute in the region. There are reports of landmines in the Preah Vihear temple area.
Exercise a high degree of caution if you are travelling to any other Thai–Cambodian border areas.
Political tensions
Political instability in Thailand has created a volatile and unpredictable security environment throughout the country, particularly in Bangkok.
Legal provisions may allow the military to retain and exercise sweeping powers that could include the right to:
- prevent public gatherings
- censor media
- set up checkpoints
- restrict movement
- search for weapons
- exercise force in response to violence
Such measures could be enforced at any time. Some television, radio stations and web sites may be unavailable, and access to social media services may be intermittently suspended.
Petty crime, such as purse snatching, pickpocketing and theft, is common. Thieves sometimes use razors to cut purses and bags open to remove their contents.
- Don’t leave bags unattended
- Ensure that your personal belongings, including your passport and travel documents, are secure at all times, especially in tourist areas, crowded markets and bus or train stations
- Avoid walking in dark alleys or isolated areas
Thefts occur on cross-country buses and vans. Personal belongings, including passports, have been stolen from luggage compartments under buses, especially on long-distance journeys. Use only reputable transportation companies.
Break-ins occur at budget guesthouses, sometimes while guests are asleep in their rooms.
Be careful at night in entertainment areas throughout the country, including in Koh Pha Ngan and Koh Tao, particularly during full moon parties, Songkran, and other events in popular tourist locations. Robberies and assaults (including sexual assaults) can occur during these events. Passport thefts and losses are common.
Violent crime against foreigners occurs occasionally.
You should report all criminal incidents to the Thai police in the jurisdiction where the incident occurred before leaving Thailand.
Many Canadians fall victim to a variety of scams while visiting Thailand. You should report all incidents to the tourist police.
Credit card and ATM fraud
Credit card and ATM fraud occurs. Be cautious when using debit or credit cards:
- pay careful attention when your cards are being handled by others
- use ATMs located in well-lit public areas or inside a bank or business
- avoid using card readers with an irregular or unusual feature
- cover the keypad with one hand when entering your PIN
- check for any unauthorized transactions on your account statements
Rental scams
Rental companies have at times accused renters of causing damage upon return of the equipment. In some cases, renters who refused to pay were harassed and threatened, and their passports (left as collateral) were withheld. Some companies have also stolen the motorcycle and then claimed compensation from the renter.
Before renting a motorcycle or personal watercraft, read all rental contracts thoroughly to ensure that the vehicle is insured to cover damage and theft. Take photos of existing damage on rented vehicles as proof of pre-existing damage.
You must never use your Canadian passport as collateral for rental. If your passport is inaccessible or stolen because of such a situation, you may be subject to investigation by Passport Canada and may receive limited passport services.
Only rent from reputable companies.
Entertainment venues
Some bars, nightclubs and entertainment venues may try to charge exorbitant prices. Discussions about overcharging may lead to threats of violence.
- Confirm the prices before consumption
- Avoid running a tab
- Avoid leaving your credit card with bar or restaurant staff
Travel agencies
When dealing with travel agencies, ensure that the company is a reputable tour organization before providing payment.
Investment fraud
If you plan on buying property or making other investments in Thailand seek legal advice in Canada and Thailand. Do so before making commitments. Related disputes could take time and be costly to resolve.
Gems and jewellery purchases
In scams involving gems and jewellery, merchants sell lower-quality items at inflated prices with promises that the items can be resold at a profit. The guarantees that merchants offer are not always honoured.
Carefully consider all purchases if you are not knowledgeable about gems and jewellery. The Government of Canada cannot assist in obtaining refunds for purchases made.
Overseas fraud
Spiked food and drinks
Never leave food or drinks unattended or in the care of strangers. Be wary of accepting snacks, beverages, gum or cigarettes from new acquaintances. These items may contain drugs that could put you at risk of sexual assault and robbery.
Seek immediate medical attention if you suspect that you have been drugged.
Women’s safety
Sexual assaults against foreign women have occurred. Be particularly vigilant during full moon parties, Songkran, and other events in popular tourist locations.
If you are victim of a sexual assault, you should seek medical attention and report the situation immediately to local authorities and the nearest Canadian office.
Advice for women travellers
There is a threat of terrorism in Thailand. Although infrequent outside of the southern provinces of Narathiwat, Pattani, Songkhla and Yala, small-scale bomb attacks have occurred in public places. Further attacks are possible.
Targets could include:
- government buildings, including schools
- places of worship
- airports and other transportation hubs and networks
- public areas such as tourist attractions, restaurants, bars, coffee shops, shopping centres, markets, hotels and other sites frequented by foreigners
Always be aware of your surroundings when in public places.
Demonstrations
Large demonstrations are taking place regularly in Bangkok and across the country. There are social tensions, and demonstrations are likely to continue.
Even peaceful demonstrations can turn violent at any time. They can also disrupt traffic and public transportation when they block major roads and intersections and may cause the closure of mass transit stations.
Maintain a high level of personal security awareness at all times.
Demonstration sites in Bangkok include:
- the areas around the Victory Monument
- Thammasat University
- the Bangkok Arts and Cultural Centre
- the Democracy Monument
- Ratchaprasong intersection
Other areas of the city may also be affected by protests and associated movements. Demonstrations have also taken place in other cities.
- Avoid military installations and concentrations of security personnel
- Expect a heightened security presence in several areas
- Carry identification documents at all time
- Avoid areas where demonstrations and large gatherings are taking place
- Follow the instructions of local authorities
- Monitor local media for information on ongoing demonstrations
Mass gatherings (large-scale events)
Water activities
Deaths have occurred due to contact with poisonous jellyfish off Koh Lanta, Koh Pha Ngan, Koh Phi Phi, Krabi and Phuket.
Riptides in coastal areas can be strong, including in the popular destinations of Cha-am/Hua Hin, Koh Samui, Pattaya, Phuket and Rayong. There have been several deaths due to drowning.
Diving schools and rescue services may not adhere to international standards.
- Rent water sports equipment only from operators affiliated with major international training organizations
- Exercise extreme caution when swimming or practising water activities
- Heed flag warnings and don’t swim when a red flag is displayed
- If stung by a jellyfish, seek immediate medical assistance
Water safety abroad
Adventure tourism
If you undertake adventure sports, such as zip-lining, rock climbing, speleology, elephant trekking or parasailing, choose a well-established and reputable company that has insurance.
Tour operators may not adhere to international standards. If you have any doubt concerning the safety of the installation or equipment, don’t use them. Ensure that your travel insurance covers the recreational activities you choose.
If engaging in adventure tourism:
- never do so alone
- always hire an experienced guide from a reputable company
- buy travel insurance that includes helicopter rescue and medical evacuation
- ensure that your physical condition is good enough to meet the challenges of your activity
- don’t venture off marked trails
- ensure that you’re properly equipped
- ensure that you’re well informed about weather and other conditions that may pose a hazard
- inform a family member or friend of your itinerary
- obtain detailed information on each activity before setting out
Chemical pesticide poisoning
There have been cases of poisoning linked to the use of chemical pesticides, including phosphine. Seek immediate medical assistance if you believe that you have been exposed to a chemical pesticide and are experiencing unusual symptoms.
Seek information on whether or not chemical pesticides are used in your accommodations.
Road safety
Accidents involving vehicles and pedestrians are extremely frequent in Thailand.
Hazardous road conditions, adverse weather conditions, local disregard for traffic laws and drunk driving result in frequent accidents.
Some vehicles may drive against the flow of traffic and on the sidewalks, particularly motorcycles.
Drunk driving and accidents are much more frequent around the western New Year (January 1) and Thai New Year (Songkran, mid-April). Be particularly vigilant when driving during these holiday periods.
Slow-moving trucks limit speed and visibility. Avoid driving on mountain roads at night, especially during the rainy season (June to October). Paved roads connect major cities, but most have only two lanes. Some roads can become impassable, particularly during the rainy season.
Pedestrians and cyclists should be particularly careful. You should always use elevated walkways/pedestrian bridges whenever possible, especially in Bangkok.
Motorcycles
Motorcycle accidents are common and are responsible for the majority of road deaths. Rental scooters and motorcycles are often poorly maintained, making them unsafe to their riders and others on the road.
Helmets are mandatory for motorcycle riders (including passengers), but many helmets don’t meet international safety standards.
Insurance claims could be denied if you were driving without a motorcycle licence.
Avoid driving or riding motorcycles in Thailand, even if you are an experienced motorcyclist
Public transportation
Use licensed taxis from official taxi stands, limousine services or a trusted ride-sharing app.
If arriving by air, arrange to be picked up by hotel shuttle services, use a trusted ride-sharing app, the airport rail-link service or official airport buses.
Unlicensed vehicles (bearing black and white licence plates) are not correctly insured to carry passengers and may not use meters. Many taxis may not be equipped with backseat seatbelts.
Don’t share a taxi with strangers.
Disputes with taxis operators, tuk-tuks (motorized rickshaws), etc., occur and have occasionally resulted in violence or intimidation. Should a dispute occur and you feel threatened, seek local police's assistance to settle the matter.
Marine transportation
Passenger boats accidents have occurred due to overloading and poor maintenance of some vessels. Vessels often lack adequate safety equipment.
Don’t board vessels that appear overloaded or unseaworthy.
In the past, rail lines in the far south have been the targets of sabotage and armed attacks.
Train accidents in recent years have caused injuries and deaths.
Pirate attacks and armed robbery against ships occur in coastal waters. Mariners should take appropriate precautions.
Live piracy report - International Maritime Bureau
We do not make assessments on the compliance of foreign domestic airlines with international safety standards.
Information about foreign domestic airlines
Every country or territory decides who can enter or exit through its borders. The Government of Canada cannot intervene on your behalf if you do not meet your destination’s entry or exit requirements.
We have obtained the information on this page from the Thai authorities. It can, however, change at any time.
Verify this information with the Foreign Representatives in Canada .
Entry requirements vary depending on the type of passport you use for travel.
Before you travel, check with your transportation company about passport requirements. Its rules on passport validity may be more stringent than the country’s entry rules.
Regular Canadian passport
Your passport must be valid at least 6 months upon entry into Thailand.
Passport for official travel
Different entry rules may apply.
Official travel
Passport with “X” gender identifier
While the Government of Canada issues passports with an “X” gender identifier, it cannot guarantee your entry or transit through other countries. You might face entry restrictions in countries that do not recognize the “X” gender identifier. Before you leave, check with the closest foreign representative for your destination.
Other travel documents
Different entry rules may apply when travelling with a temporary passport or an emergency travel document. Before you leave, check with the closest foreign representative for your destination.
Useful links
- Foreign Representatives in Canada
- Canadian passports
Tourist visa: not required for stays of up to 30 days Business visa: required Student visa: required Working visa: required
If you’re travelling to Thailand for tourism with a regular Canadian passport, you can obtain a 30-day visa upon arrival.
If you obtain a multiple-entry tourist visa, you can stay for up to 60 days. The visa is valid for 6 months and must be obtained before travelling.
If you wish to stay longer than 60 days or work or study in Thailand, you must obtain the appropriate visa from a Thai embassy or consulate. Local authorities are actively monitoring and enforcing compliance with visa regulations.
Those applying for non-immigrant visas of category "O-A" need to show proof of a valid health insurance meeting specific criteria.
Guidelines Non-Immigrant Visa (O-A) - Thai General Insurance Association
Other entry requirements
Thai Border officials may ask you to show them a return or onward ticket and proof that you have sufficient funds to support yourself for the duration of your stay.
If you are unable to do so, you may be denied entry.
Entry stamp
You must get an entry stamp from an immigration officer at the point of entry into Thailand. Don’t get your visa, visa extension or entry stamp from visa shops or travel agents in Thailand.
A passport that has been altered or that contains counterfeit visas, and entry/exit stamps is deemed invalid. Offenders can expect jail sentences, fines and deportation, and may also be prohibited from entering Thailand in the future.
Length of stay
The date indicated on your Thai entry stamp determines how long you may stay in the country, even if your visa shows a different date.
All foreigners staying in Thailand longer than 3 months must notify Thailand’s immigration bureau of their residence every 90 days.
The Royal Thai Police perform random visa checks and strict penalties are enforced for overstaying. Canadians overstaying their visa have been arrested and detained until deportation. Deportation procedures are at the foreigner’s own expense and can be lengthy. Detention conditions in immigration detention centres are poor.
If you overstay, regardless of whether you leave Thailand voluntarily or are deported, you may be banned from re-entering Thailand for 1 to 10 years.
Notification of stay longer than 90 days - Thailand’s immigration bureau
Dual citizenship
If you are a dual citizen, you must enter and exit Thailand with the same nationality passport.
Children and travel
Learn more about travelling with children .
Yellow fever
Learn about potential entry requirements related to yellow fever (vaccines section).
Relevant Travel Health Notices
- Global Measles Notice - 13 March, 2024
- Zika virus: Advice for travellers - 31 August, 2023
- COVID-19 and International Travel - 13 March, 2024
- Mpox (monkeypox): Advice for travellers - 20 February, 2024
This section contains information on possible health risks and restrictions regularly found or ongoing in the destination. Follow this advice to lower your risk of becoming ill while travelling. Not all risks are listed below.
Consult a health care professional or visit a travel health clinic preferably 6 weeks before you travel to get personalized health advice and recommendations.
Routine vaccines
Be sure that your routine vaccinations , as per your province or territory , are up-to-date before travelling, regardless of your destination.
Some of these vaccinations include measles-mumps-rubella (MMR), diphtheria, tetanus, pertussis, polio, varicella (chickenpox), influenza and others.
Pre-travel vaccines and medications
You may be at risk for preventable diseases while travelling in this destination. Talk to a travel health professional about which medications or vaccines may be right for you, based on your destination and itinerary.
Yellow fever is a disease caused by a flavivirus from the bite of an infected mosquito.
Travellers get vaccinated either because it is required to enter a country or because it is recommended for their protection.
- There is no risk of yellow fever in this country.
Country Entry Requirement*
- Proof of vaccination is required if you are coming from or have transited through an airport of a country where yellow fever occurs.
Recommendation
- Vaccination is not recommended.
- Discuss travel plans, activities, and destinations with a health care professional.
- Contact a designated Yellow Fever Vaccination Centre well in advance of your trip to arrange for vaccination.
About Yellow Fever
Yellow Fever Vaccination Centres in Canada * It is important to note that country entry requirements may not reflect your risk of yellow fever at your destination. It is recommended that you contact the nearest diplomatic or consular office of the destination(s) you will be visiting to verify any additional entry requirements.
There is a risk of hepatitis A in this destination. It is a disease of the liver. People can get hepatitis A if they ingest contaminated food or water, eat foods prepared by an infectious person, or if they have close physical contact (such as oral-anal sex) with an infectious person, although casual contact among people does not spread the virus.
Practise safe food and water precautions and wash your hands often. Vaccination is recommended for all travellers to areas where hepatitis A is present.
Measles is a highly contagious viral disease. It can spread quickly from person to person by direct contact and through droplets in the air.
Anyone who is not protected against measles is at risk of being infected with it when travelling internationally.
Regardless of where you are going, talk to a health care professional before travelling to make sure you are fully protected against measles.
Japanese encephalitis is a viral infection that can cause swelling of the brain. It is spread to humans through the bite of an infected mosquito. Risk is very low for most travellers. Travellers at relatively higher risk may want to consider vaccination for JE prior to travelling.
Travellers are at higher risk if they will be:
- travelling long term (e.g. more than 30 days)
- making multiple trips to endemic areas
- staying for extended periods in rural areas
- visiting an area suffering a JE outbreak
- engaging in activities involving high contact with mosquitos (e.g., entomologists)
Hepatitis B is a risk in every destination. It is a viral liver disease that is easily transmitted from one person to another through exposure to blood and body fluids containing the hepatitis B virus. Travellers who may be exposed to blood or other bodily fluids (e.g., through sexual contact, medical treatment, sharing needles, tattooing, acupuncture or occupational exposure) are at higher risk of getting hepatitis B.
Hepatitis B vaccination is recommended for all travellers. Prevent hepatitis B infection by practicing safe sex, only using new and sterile drug equipment, and only getting tattoos and piercings in settings that follow public health regulations and standards.
Malaria is a serious and sometimes fatal disease that is caused by parasites spread through the bites of mosquitoes. There is a risk of malaria in certain areas and/or during a certain time of year in this destination.
Antimalarial medication may be recommended depending on your itinerary and the time of year you are travelling. Consult a health care professional or visit a travel health clinic before travelling to discuss your options. It is recommended to do this 6 weeks before travel, however, it is still a good idea any time before leaving. Protect yourself from mosquito bites at all times: • Cover your skin and use an approved insect repellent on uncovered skin. • Exclude mosquitoes from your living area with screening and/or closed, well-sealed doors and windows. • Use insecticide-treated bed nets if mosquitoes cannot be excluded from your living area. • Wear permethrin-treated clothing. If you develop symptoms similar to malaria when you are travelling or up to a year after you return home, see a health care professional immediately. Tell them where you have been travelling or living.
In this destination, rabies is carried by dogs and some wildlife, including bats. Rabies is a deadly disease that spreads to humans primarily through bites or scratches from an infected animal. While travelling, take precautions , including keeping your distance from animals (including free-roaming dogs), and closely supervising children.
If you are bitten or scratched by an animal while travelling, immediately wash the wound with soap and clean water and see a health care professional. Rabies treatment is often available in this destination.
Before travel, discuss rabies vaccination with a health care professional. It may be recommended for travellers who are at high risk of exposure (e.g., occupational risk such as veterinarians and wildlife workers, children, adventure travellers and spelunkers, and others in close contact with animals).
Coronavirus disease (COVID-19) is an infectious viral disease. It can spread from person to person by direct contact and through droplets in the air.
It is recommended that all eligible travellers complete a COVID-19 vaccine series along with any additional recommended doses in Canada before travelling. Evidence shows that vaccines are very effective at preventing severe illness, hospitalization and death from COVID-19. While vaccination provides better protection against serious illness, you may still be at risk of infection from the virus that causes COVID-19. Anyone who has not completed a vaccine series is at increased risk of being infected with the virus that causes COVID-19 and is at greater risk for severe disease when travelling internationally.
Before travelling, verify your destination’s COVID-19 vaccination entry/exit requirements. Regardless of where you are going, talk to a health care professional before travelling to make sure you are adequately protected against COVID-19.
Safe food and water precautions
Many illnesses can be caused by eating food or drinking beverages contaminated by bacteria, parasites, toxins, or viruses, or by swimming or bathing in contaminated water.
- Learn more about food and water precautions to take to avoid getting sick by visiting our eat and drink safely abroad page. Remember: Boil it, cook it, peel it, or leave it!
- Avoid getting water into your eyes, mouth or nose when swimming or participating in activities in freshwater (streams, canals, lakes), particularly after flooding or heavy rain. Water may look clean but could still be polluted or contaminated.
- Avoid inhaling or swallowing water while bathing, showering, or swimming in pools or hot tubs.
Cholera is a risk in parts of this country. Most travellers are at very low risk.
To protect against cholera, all travellers should practise safe food and water precautions .
Travellers at higher risk of getting cholera include those:
- visiting, working or living in areas with limited access to safe food, water and proper sanitation
- visiting areas where outbreaks are occurring
Vaccination may be recommended for high-risk travellers, and should be discussed with a health care professional.
Travellers' diarrhea is the most common illness affecting travellers. It is spread from eating or drinking contaminated food or water.
Risk of developing travellers' diarrhea increases when travelling in regions with poor standards of hygiene and sanitation. Practise safe food and water precautions.
The most important treatment for travellers' diarrhea is rehydration (drinking lots of fluids). Carry oral rehydration salts when travelling.
Typhoid is a bacterial infection spread by contaminated food or water. Risk is higher among children, travellers going to rural areas, travellers visiting friends and relatives or those travelling for a long period of time.
Travellers visiting regions with a risk of typhoid, especially those exposed to places with poor sanitation, should speak to a health care professional about vaccination.
Insect bite prevention
Many diseases are spread by the bites of infected insects such as mosquitoes, ticks, fleas or flies. When travelling to areas where infected insects may be present:
- Use insect repellent (bug spray) on exposed skin
- Cover up with light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- Minimize exposure to insects
- Use mosquito netting when sleeping outdoors or in buildings that are not fully enclosed
To learn more about how you can reduce your risk of infection and disease caused by bites, both at home and abroad, visit our insect bite prevention page.
Find out what types of insects are present where you’re travelling, when they’re most active, and the symptoms of the diseases they spread.
There is a risk of chikungunya in this country. The risk may vary between regions of a country. Chikungunya is a virus spread through the bite of an infected mosquito. Chikungunya can cause a viral disease that typically causes fever and pain in the joints. In some cases, the joint pain can be severe and last for months or years.
Protect yourself from mosquito bites at all times. There is no vaccine available for chikungunya.
- In this country, dengue is a risk to travellers. It is a viral disease spread to humans by mosquito bites.
- Dengue can cause flu-like symptoms. In some cases, it can lead to severe dengue, which can be fatal.
- The level of risk of dengue changes seasonally, and varies from year to year. The level of risk also varies between regions in a country and can depend on the elevation in the region.
- Mosquitoes carrying dengue typically bite during the daytime, particularly around sunrise and sunset.
- Protect yourself from mosquito bites . There is no vaccine or medication that protects against dengue.
Zika virus is a risk in this country.
Zika virus is primarily spread through the bite of an infected mosquito. It can also be sexually transmitted. Zika virus can cause serious birth defects.
During your trip:
- Prevent mosquito bites at all times.
- Use condoms correctly or avoid sexual contact, particularly if you are pregnant.
If you are pregnant or planning a pregnancy, you should discuss the potential risks of travelling to this destination with your health care provider. You may choose to avoid or postpone travel.
For more information, see Zika virus: Pregnant or planning a pregnancy.
Animal precautions
Some infections, such as rabies and influenza, can be shared between humans and animals. Certain types of activities may increase your chance of contact with animals, such as travelling in rural or forested areas, camping, hiking, and visiting wet markets (places where live animals are slaughtered and sold) or caves.
Travellers are cautioned to avoid contact with animals, including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats, and to avoid eating undercooked wild game.
Closely supervise children, as they are more likely to come in contact with animals.
Human cases of avian influenza have been reported in this destination. Avian influenza is a viral infection that can spread quickly and easily among birds and in rare cases it can infect mammals, including people. The risk is low for most travellers.
Avoid contact with birds, including wild, farm, and backyard birds (alive or dead) and surfaces that may have bird droppings on them. Ensure all poultry dishes, including eggs and wild game, are properly cooked.
Travellers with a higher risk of exposure include those:
- visiting live bird/animal markets or poultry farms
- working with poultry (such as chickens, turkeys, domestic ducks)
- hunting, de-feathering, field dressing and butchering wild birds and wild mammals
- working with wild birds for activities such as research, conservation, or rehabilitation
- working with wild mammals, especially those that eat wild birds (e.g., foxes)
All eligible people are encouraged to get the seasonal influenza shot, which will protect them against human influenza viruses. While the seasonal influenza shot does not prevent infection with avian influenza, it can reduce the chance of getting sick with human and avian influenza viruses at the same time.
Person-to-person infections
Stay home if you’re sick and practise proper cough and sneeze etiquette , which includes coughing or sneezing into a tissue or the bend of your arm, not your hand. Reduce your risk of colds, the flu and other illnesses by:
- washing your hands often
- avoiding or limiting the amount of time spent in closed spaces, crowded places, or at large-scale events (concerts, sporting events, rallies)
- avoiding close physical contact with people who may be showing symptoms of illness
Sexually transmitted infections (STIs) , HIV , and mpox are spread through blood and bodily fluids; use condoms, practise safe sex, and limit your number of sexual partners. Check with your local public health authority pre-travel to determine your eligibility for mpox vaccine.
Tuberculosis is an infection caused by bacteria and usually affects the lungs.
For most travellers the risk of tuberculosis is low.
Travellers who may be at high risk while travelling in regions with risk of tuberculosis should discuss pre- and post-travel options with a health care professional.
High-risk travellers include those visiting or working in prisons, refugee camps, homeless shelters, or hospitals, or travellers visiting friends and relatives.
HIV (Human Immunodeficiency Virus) is a virus that attacks and impairs the immune system, resulting in a chronic, progressive illness known as AIDS (Acquired Immunodeficiency Syndrome).
High risk activities include anything which puts you in contact with blood or body fluids, such as unprotected sex and exposure to unsterilized needles for medications or other substances (for example, steroids and drugs), tattooing, body-piercing or acupuncture.
Medical services and facilities
Excellent healthcare is available in major cities, particularly in private hospitals and clinics. Quality of care varies significantly in rural areas.
Establishments may require confirmation of health insurance coverage, a guarantee of payment or an upfront deposit before admitting patients.
Psychiatric or psychological facilities and services in Thailand may not meet international standards. Canadians with mental illness have been committed to state facilities, detained and deported.
Medical evacuation can be very expensive and you may need it in case of serious illness or injury.
Make sure you get travel insurance that includes coverage for medical evacuation and hospital stays.
Travel health and safety
You must abide by local laws.
Learn about what you should do and how we can help if you are arrested or detained abroad .
Overview of the criminal law system in Thailand
Identification
You must carry identification at all times. Carry a photocopy of your passport bio-data page and Thai visa or entry stamp.
Police may still require that you produce the original document. If you fail to do so, you could be detained.
Penalties for possession, use or trafficking of illegal drugs, including cannabis, are very severe. Convicted offenders can expect heavy fines, jail sentences or even the death penalty.
Police regularly perform spot checks to search for illegal drugs, particularly in and around entertainment venues. Uniformed or undercover police may conduct physical searches and may screen your belongings. You may be asked to provide a urine sample.
If you carry prescription drugs or other medicines, keep them in clearly marked, original packaging.
Certain prescription drugs are frequently sold without prescription in entertainment areas and coastal resorts, including on the street. You should never buy controlled drugs without prescription or on the street. These may be counterfeit or could contain illegal substances. If you purchase these drugs, you could be subject to scrutiny or detained.
The legal drinking age in Thailand is 20.
It is illegal to promote the consumption of alcohol. You could be fined or taken to court for posting on social media any pictures that include alcoholic beverages or people consuming alcohol.
Drugs, alcohol and travel
It is prohibited to import, possess or use e-cigarettes, vaporisers, e-baraku (e-hashish) and their refills. Convicted offenders can expect heavy fines or jail sentences of up to 10 years.
A smoking ban is in effect on several beaches across the country and is punishable by a 100,000-baht fine and up to 1 year in prison.
Check with local authorities and look for no-smoking signs before smoking on a beach.
Gambling, with some exceptions, is illegal.
Lèse-majesté
Actions or words that are considered offensive or insulting to the king or the royal family are illegal and may result in criminal prosecution and lengthy prison sentences.
Don’t make any public statement, including online, that could be perceived as critical of:
- the monarchy
- the political situation in Thailand
- the Royal Thai Army
Restricted goods
There are strict regulations regarding the importation and exportation of images of the Buddha, counterfeit goods, pornographic material and other items.
Consult the complete list of restricted and prohibited items before travelling.
Restricted goods - Thai Customs
Feeding fish
Feeding fish in the ocean is illegal and punishable by a 100000-baht fine and up to 1 year in prison.
Do not feed fish in the ocean and avoid boat tour operators who encourage tourists to do so.
Traffic drives on the left.
You must be at least 18 years old to drive a car in Thailand.
You must carry an international driving permit or a Thai driver’s licence to drive in Thailand.
It is illegal to operate a motorcycle without a valid Thai motorcycle licence or an international driving permit with a motorcycle endorsement.
Helmets are mandatory for motorcycle riders (including passengers), but many helmets do not meet international safety standards.
Carry your identification card, driver’s licence and vehicle registration book at all times.
International Driving Permit
Housing foreign citizens
All hosts, including hotel staff and homeowners, must notify local authorities that they are housing foreign citizens within 24 hours of the arrival of these foreigners.
Commercial surrogacy
Commercial surrogacy is illegal in Thailand.
If you’re planning to visit Thailand for the purpose of commissioning surrogacy arrangements, you should consider the potential challenges involved in pursuing international surrogacy and seek specialist legal advice on Thai and Canadian laws prior to making any arrangements.
It is also recommended that you consult with Immigration, Refugees and Citizenship Canada (IRCC) on current policies regarding citizenship through descent and the issuance of Canadian travel documents.
Dual citizenship is not legally recognized in Thailand.
If local authorities consider you a citizen of Thailand, they may refuse to grant you access to Canadian consular services. This will prevent us from providing you with those services.
Travellers with dual citizenship
Compulsory military service
Male Thai citizens are subject to compulsory military service when they reach the age of 21. If you’re a dual Canadian–Thai citizen, you may be subject to this requirement.
International Child Abduction
The Hague Convention on the Civil Aspects of International Child Abduction is an international treaty. It can help parents with the return of children who have been removed to or retained in certain countries in violation of custody rights. It does not apply between Canada and Thailand.
If your child was wrongfully taken to, or is being held in Thailand by an abducting parent:
- act as quickly as you can
- consult a lawyer in Canada and in Thailand to explore all the legal options for the return of your child
- report the situation to the nearest Canadian government office abroad or to the Vulnerable Children’s Consular Unit at Global Affairs Canada by calling the Emergency Watch and Response Centre.
If your child was removed from a country other than Canada, consult a lawyer to determine if The Hague Convention applies.
Be aware that Canadian consular officials cannot interfere in private legal matters or in another country’s judicial affairs.
- International Child Abduction: A Guidebook for Left-Behind Parents
- Travelling with children
- Canadian embassies and consulates by destination
- Emergency Watch and Response Centre
The currency of Thailand is the Thai baht (THB).
Seismic activity
Thailand is located in an active seismic zone and is prone to earthquakes and tsunamis.
In case of an earthquake or a tsunami alert, follow the instructions of local authorities.
Tsunami alerts - U.S. Tsunami Warning System
The rainy (or monsoon) season extends from June to October. Seasonal flooding can hamper overland travel and reduce the provision of essential services. Roads may become impassable and bridges damaged.
Jungle treks are not advisable during the rainy season due to the possibility of mudslides. Flash flooding in caves has caused fatalities.
- Weather warnings - Thai Meteorological department
- Mekong river levels - Mekong River Commission
- Tornadoes, cyclones, hurricanes, typhoons and monsoons
Air pollution
Air pollution fluctuates greatly and can be hazardous in urban areas, including Bangkok and Chiang Mai. Seasonal smog during the dry season is recurrent. In the northern provinces, including Chiang Mai, air quality can also be affected by agricultural burning.
You should monitor air pollution levels, especially if you suffer from respiratory ailments or if you have a pre-existing medical condition.
Local authorities recommend that children, seniors and pregnant women wear anti-pollution masks, and minimize outdoor activities, when air pollution levels are high.
Air pollution in Thailand – World Air Quality Index
Local services
In case of emergency, dial:
- police: 191
- tourist police: 1155
- medical assistance: 1669
- firefighters: 199
General services
The Tourism Authority of Thailand offers general advice for tourists. Dial 1672 and press 9 for English.
Consular assistance
Online appointment requests
Thailand, Cambodia, Laos
For emergency consular assistance, call the Embassy of Canada to Thailand, in Bangkok, and follow the instructions. At any time, you may also contact the Emergency Watch and Response Centre in Ottawa.
The decision to travel is your choice and you are responsible for your personal safety abroad. We take the safety and security of Canadians abroad very seriously and provide credible and timely information in our Travel Advice to enable you to make well-informed decisions regarding your travel abroad.
The content on this page is provided for information only. While we make every effort to give you correct information, it is provided on an "as is" basis without warranty of any kind, expressed or implied. The Government of Canada does not assume responsibility and will not be liable for any damages in connection to the information provided.
If you need consular assistance while abroad, we will make every effort to help you. However, there may be constraints that will limit the ability of the Government of Canada to provide services.
Learn more about consular services .
Risk Levels
take normal security precautions.
Take similar precautions to those you would take in Canada.
Exercise a high degree of caution
There are certain safety and security concerns or the situation could change quickly. Be very cautious at all times, monitor local media and follow the instructions of local authorities.
IMPORTANT: The two levels below are official Government of Canada Travel Advisories and are issued when the safety and security of Canadians travelling or living in the country or region may be at risk.
Avoid non-essential travel
Your safety and security could be at risk. You should think about your need to travel to this country, territory or region based on family or business requirements, knowledge of or familiarity with the region, and other factors. If you are already there, think about whether you really need to be there. If you do not need to be there, you should think about leaving.
Avoid all travel
You should not travel to this country, territory or region. Your personal safety and security are at great risk. If you are already there, you should think about leaving if it is safe to do so.

IMAGES
VIDEO
COMMENTS
Malaria: CDC recommends that travelers going to certain areas of Thailand take prescription medicine to prevent malaria. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about which malaria medication you should take.
Rare to few cases in other parts of Thailand, including the cities of Bangkok, Chiang Mai, and Chiang Rai, and the islands of Koh Phangan, Koh Samui, and Phuket. ... All travelers should seek medical attention in the event of fever during or after return from travel to areas with malaria. 5. Primaquine and tafenoquine can cause hemolytic anemia ...
Malaria in humans is caused by protozoan parasites of the genus Plasmodium, including Plasmodium falciparum, P. malariae, P. ovale, and P. vivax. In addition, zoonotic forms have been documented as causes of human infections and some deaths, especially P. knowlesi, a parasite of Old World (Eastern Hemisphere) monkeys, in Southeast Asia.
All other areas with malaria transmission (including the provinces of Buri Ram and Satun): No chemoprophylaxis recommended (insect bite precautions and mosquito avoidance only) 4; Related Maps. Map 2-16 Malaria prevention in Thailand. Other Vaccines to Consider. See Health Information for Travelers to Thailand.
M A P 2 -2 6. Malaria in Thailand (updated August 8, 2019) CHIANG RAI Thiang Rai LOEI Malaria Recommendations LAOS. Vientiane NONC UDON NAKHON SAKON PH 0M NONC NAKHON LAM PHU HON KAEN KALASIN MUKDA AN Chemoprophylaxis Mosquito avoidance only Tourist Destination VIE MAE SON Chiang Mat CHIANG M PHAYAO NAN LAMPANG RAN PHANC 6LAMPHUN PHRAE ...
Thailand is one of 8 new countries which have been recently identified by WHO as having the potential to eliminate malaria by 2025. In 1949, malaria was the leading cause of mortality in Thailand, resulting in 38 046 deaths a year. Despite resurgences of multidrug-resistant malaria over the decades, Thailand only recorded 13 deaths in 2019.
The country list is a compilation of key information to facilitate safe international travel. The country list is a compilation of key information to facilitate safe international travel. Global; Regions. WHO Regional websites. Africa; Americas; South-East Asia; ... and malaria situation per country - 2022 edition. 19 November 2022 | Publication.
Thailand aims to eliminate malaria by 2024, following China's malaria elimination certification in 2021 and Sri Lanka's in 2016. The country reported just 2893 malaria cases last year, down ...
Thailand's National Malaria Elimination Strategy 2017-2026 (NMES) reoriented the malaria control program into an elimination program centered on upgraded surveillance. Thus, in 2017, Thailand ...
The number of malaria cases in Thailand decreased 90% between 2012 and 2020, yet elimination has remained a major public health challenge with persistent transmission foci and ongoing importation. There are three main hotspots of malaria transmission in Thailand: Ubon Ratchathani and Sisaket in the Northeast; Tak in the West; and Yala in the South.
Call us in Washington, D.C. at 1-888-407-4747 (toll-free in the United States and Canada) or 1-202-501-4444 (from all other countries) from 8:00 a.m. to 8:00 p.m., Eastern Standard Time, Monday through Friday (except U.S. federal holidays). See the State Department's travel website for the Worldwide Caution and Travel Advisories.
BANGKOK (NNT) - Thailand is striving to be malaria-free by 2024, with authorities urging people to take part in online World Malaria Day 2022 activities. According to Dr Opas Karnkawinpong, director-general of the Department of Disease Control (DDC), the World Health Organization (WHO) observes World Malaria Day every year on April 25 to highlight the commitment of global communities in ...
INTRODUCTION. Thailand aims to eliminate malaria by 2026. Over the past decade, malaria incidence in the total population has significantly decreased, declining from 3.6 cases per 1,000 people in 2012 to 0.2 cases per 1,000 people in 2021. 1 This success in reducing malaria burden is due to intense intervention activities based on timely case investigation, case classification, and foci ...
Malaria Information and Prophylaxis, by Country [L] The information presented in this table is consistent 1 with the information in the CDC Health Information for International Travel (the "Yellow Book"). All, except none in the city of Vientiane. Along the Laos-Burma (Myanmar) border in the provinces of Bokeo and Louang Namtha and along ...
Check the latest information on risk from COVID-19 risk for Thailand on TravelHealthPro.If you have severe symptoms, or any questions related to COVID-19, while in Thailand, call the Thai COVID-19 ...
Malaria continues to pose a significant health threat. Rapid identification of malaria infections and the deployment of active surveillance tools are crucial for achieving malaria elimination in regions where malaria is endemic, such as certain areas of Thailand. In this study, an anomaly detection system is introduced as an early warning mechanism for potential malaria outbreaks in countries ...
Credit: Permsak Tosawad, Inform Asia. Thailand has seen incredible progress against malaria over the past decade - with an 88 percent decline in malaria cases since 2012 and a 74.7 percent reduction in the number of villages with malaria transmission, the country is well on its way to reaching its goal of eliminating malaria by 2024.
All foreigners staying in Thailand longer than 3 months must notify Thailand's immigration bureau of their residence every 90 days. The Royal Thai Police perform random visa checks and strict penalties are enforced for overstaying. Canadians overstaying their visa have been arrested and detained until deportation.