- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Is it Safe to Travel on an Airplane After a Stroke?
Many stroke survivors and families of stroke survivors worry about the safety of flying as a passenger in an airplane after a stroke. Is the concern warranted? It certainly is a common question, so common in fact, that a number of medical research studies have looked at this very question.
Can Flying Cause a Stroke?
Data shows that urgent medical ailments of all forms are relatively uncommon on airline flights, and the incidence of a stroke during a commercial flight is especially low.
An Australian group of medical researchers defined strokes related to air travel as any stroke occurring within 14 days of travel. After tracking 131 million passengers at Melbourne airport between 2003 and 2014, the researchers reported that stroke-related to air travel occurs in less than one in a million passengers. They found that that half of the people who had a stroke on a flight had a heart condition that is known to lead stroke . These heart conditions are fairly common, so the findings of the very low stroke rate suggest that there may not be a substantially increased risk of stroke from flying.
Another group of researchers from Spain found that a stroke occurred at a rate of one per every 35,000 flights. They found that over 70% of those who had a stroke on an airplane had carotid artery stenosis, which is narrowing of a blood vessel in the neck, a condition that is a risk factor for stroke.
Flying After a TIA or a Stroke
As it turns out, a history of stroke does not pose danger to the brain during an airline flight, and therefore, a past stroke is not a contraindication to flying on an airplane as a passenger.
A transient ischemic attack (TIA) is a mini-stroke that resolves without permanent brain damage. A TIA is very similar to a stroke and it is a warning of stroke risk. Most of the health conditions discovered during a medical TIA evaluation do not limit air travel.
However, it is important to note that a few of the medical disorders that lead to a TIA may pose a very small risk on airplane flights. These disorders include patent foramen ovale, paradoxical embolism, or hypercoagulability. If you have been diagnosed with any of these health conditions, you should get the appropriate medical treatment.
When It May Be Unsafe to Fly
Hypercoagulability is a condition that increases the tendency of blood clot formation. Several blood-clotting syndromes cause hypercoagulability.
Most strokes are caused by an interruption of blood flow due to a blood clot in the brain. Flying for long distances has been associated with an increase in blood clotting in those who are susceptible. If you have a hypercoagulable condition, it is best to talk to your healthcare provider about airplane travel and whether you need to take any special precautions.
What if a Stroke or TIA Happens in-Flight?
While it is unusual for a stroke to arise during flight, it does occur. When airline attendants are alerted of a passenger’s medical distress, they respond promptly, as they are trained to do.
If you or a loved one experiences a stroke on an airplane, nearby passengers and trained professionals are likely to notice and call for emergency medical help fairly quickly. On rare occasions, passenger flights have been diverted for medical emergencies, and emergency personnel can transport a passenger to a medical facility for diagnosis and treatment.
A Word From Verywell
A stroke causes a wide range of neurological deficits. Some of the disabilities that result from a stroke, such as impaired speech, vision changes, and trouble walking, may impair your ability to get around and communicate with others in the air travel setting.
Stroke survivors may suffer from deficits in spatial perception, which can increase the risk of getting lost in an airport. Communication problems after a stroke can lead to a misunderstanding of detailed flight information. Weakness and coordination problems can make it difficult to walk long distances through an airport. Consequently, for practical reasons, many stroke survivors should travel either with a companion or with professional assistance.
If you are a stroke survivor, you can travel safely with a reasonable amount of planning.
Álvarez-velasco R, Masjuan J, Defelipe A, et al. Stroke in commercial flights . Stroke . 2016;47(4):1117-9. doi:10.1161/STROKEAHA.115.012637
Humaidan H, Yassi N, Weir L, Davis SM, Meretoja A. Airplane stroke syndrome . J Clin Neurosci . 2016;29:77-80. doi:10.1016/j.jocn.2015.12.015
Cleveland Clinic. Transient ischemic attack (TIA) or mini stroke .
Messerli FH, Rimoldi SF, Scherrer U, Meier B. Economy class syndrome, patent foramen ovale and stroke . Am J Cardiol . 2017;120(3):e29. doi:10.1016/j.amjcard.2016.07.047
Dusse LMS, Silva MVF, Freitas LG, Marcolino MS, Carvalho MDG. Economy class syndrome: what is it and who are the individuals at risk? . Rev Bras Hematol Hemoter . 2017;39(4):349–353. doi:10.1016/j.bjhh.2017.05.001
By Heidi Moawad, MD Heidi Moawad is a neurologist and expert in the field of brain health and neurological disorders. Dr. Moawad regularly writes and edits health and career content for medical books and publications.
- Open access
- Published: 01 December 2020
Historic review: select chapters of a history of stroke
- Axel Karenberg ORCID: orcid.org/0000-0002-2016-0701 1
Neurological Research and Practice volume 2 , Article number: 34 ( 2020 ) Cite this article
11k Accesses
5 Citations
14 Altmetric
Metrics details
There is no shortage of books, chapters and papers on the history of stroke focusing predominantly on the last 150 years and enumerating endless “milestones”. Instead of adding another article to this body of knowledge, this essay aims at ensuring awareness for the “big picture”, the “grandes routes”, and the “striking breakes” without overloading the reader with too much detail.
From a medical point of view, the history of stroke consists of two periods: the early era from the beginnings to 1812, and the following period from 1812 up to the present. It is argued that both periods require different methodical approaches, including disparate historiographical perspectives and varying forms of interpretation. In order to fully understand medical writings of the Greco-Roman era (Hippocratic writings, Galenic corpus) on “apoplexy”, a solid knowledge of ancient doctrines concerning health and disease is indispensable. During the Middle Ages, the spiritual perspective can be highlighted by focusing on miracle healing and patron saints. While stroke basically remained a conundrum for many doctors and patients in early modern times (ca. 1500–1800; Platter, Wepfer), the revolutionary perception and definition of the disease as a result of a lesion in the 1810s (Rochoux, Rostan) opened the door to a productive relationship of the upcoming discipline “neurology” with the natural sciences during the nineteenth century and beyond (Virchow et al.). The mostly unwritten history of stroke in the twentieth century should not only include the medical, but also the patient’s and the societal perspective.
A deeper insight into the recent and distant past will produce better educated strokologists – physicians who are able to put their own work into perspective.
“The true protagonists on the stage of medical history are the diseases”. Unfortunately, historical research often neglected this statement by French medical historian Charles Daremberg. We know a lot about famous physicians [ 1 ] and the social framing of medicine in the past [ 2 ], but comparatively little about the story of diseases themselves. Moreover, if and when they are studied by historians, the focus was and is usually put on epidemics and infectious diseases. 95% of the publications are on the history of plague, tuberculosis, syphilis and AIDS. In contrast, this essay argues that we can learn a lot about our medical past from non-epidemic, non-infectious illnesses. An excellent illustration of this approach is studying the history of stroke.
Stroke is today the second most common cause of death worldwide after heart disease, but before cancer [ 3 ]. In 2010, approximately 17 million people suffered a stroke, and another 33 million people have previously had a stroke and are still alive [ 4 ]. Obviously, we are really dealing with a “protagonist”. There seems to be just one open question to be resolved: how to assess appropriately the role of stroke in history?
Historical models and perspectives
From a medical point of view, the history of stroke comprises two periods: A first era from the beginnings to 1812, and a second timeframe from 1812 to the present (see below). However, these different time intervals require different approaches by the historian.
The modern period (i.e., the 19th and 20th centuries) can convincingly be described using a model of medical progress, which can also be called the “embryonic knowledge approach” [ 5 ]. The scientific findings of one decade can be seen as the nucleus of knowledge to be discovered in the next decade, and so on and so forth. In this perspective, Virchow’s description of thrombosis and embolism of 1846 is somehow the basis for almost all knowledge about these conditions up to the end of the twentieth century. This story of progress was mainly played out in hospitals, dissection rooms and labs, and these institutions were and are predominantly located in parts of Europe, Australasia, and the US. Thus the historian dealing with this modern period needs only a working knowledge in few modern languages to read the primary sources, if, for instance, she or he wants to find out since when blood pressure and cerebral haemorrhage were connected or how the story of secondary prevention developed.
However, this model of progressing science is not a very suitable one for the pre-1800 period. For centuries, there were no advancements at all in a modern sense of the word, and if so, they were very slow. Hence a different concept is needed for that period, and an appropriate one is the “strange object approach” [ 5 ]. According to this approach, a contemporary physician has to admit that her/his present-day medical knowledge is of very little help to understand peculiar early teachings about stroke, because they differ so much from the current actual knowledge.
The only pre-modern illustration depicting a stroke victim provides an excellent example for a “strange object” [Fig. 1 ]. The patient suffers from a so-called “chronic stroke”. Some very strange things are happening: the physician, kneeling on the floor behind the sickbed, holds a hot iron in his hand and starts to cauterize the patient’s stomach (or head?) with the glowing instrument. The patient is not unconscious and doesn’t seem to suffer from paralysis, since he is defending himself. To understand this scenery, our present-day knowledge of stroke is obviously not sufficient. In this case, the historian has to act like an ethnologist – looking not only at the medical, but also at the cultural context. All in all, however, the early story of stroke is taking place in scriptoria and scholars’ parlors, not at the bedside of hospitals or in labs. The study of its Western variant requires a solid knowledge of Ancient Greek and Latin. Additional reading ability in Arabic, Hebrew, Syriac, and other Semitic languages are quite helpful, too.
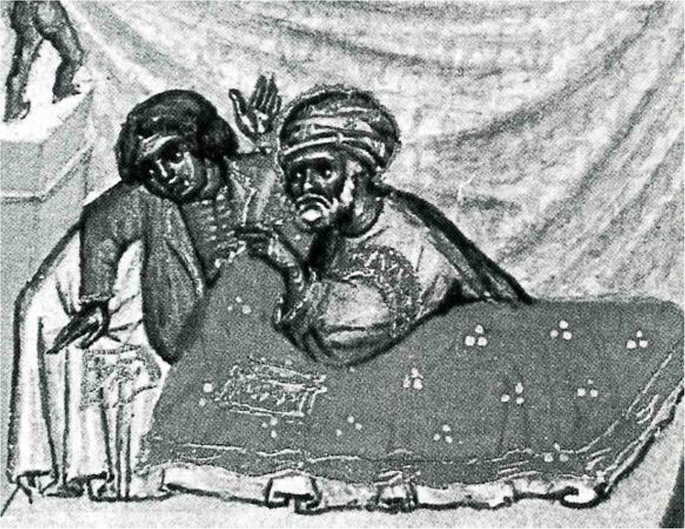
Treatment of chronic apoplexy. Miniature from ABU’L QĀSIM, Codex Series Nova 2641, Fol. 6ra. Reprinted in: (1979) Chirurgia. Lateinisch von Gerhard von Cremona. Vollständige Faksimile-Ausgabe im Originalformat. Graz: Akademische Druck- u. Verlagsanstalt. With permission of Austrian National Library, Vienna
Assuming we are able to combine these two different models successfully – from which point of view do we want to look at the evolving drama?
For doctors it seems clear that they are mainly interested in a medical perspective, in the reconstruction of changing medical knowledge. They will exclusively look at medical writings, perhaps also at medical illustrations, instruments, and institutions.
But this is of course not the whole story. What about patients suffering from stroke? Granted they are somehow part of the parcel, we have to broaden our historical horizon and consult their diaries, autobiographies and other source material [ 6 ]. Not an easy task: There are few so called ego-documents from the pre-1800 period and we are dealing with a condition including aphasic and agraphic disturbances.
How and where does society come into play? Every civilization is characterized by a spectrum of attitudes towards severe diseases of its members. Vice versa, severe diseases like stroke have a certain “image” generated within a social framework [ 7 , 8 ]. To understand societal and financial aspects, historians may therefore want to resort to various other sources including balance sheets of hospitals, communities or ministries of health as well as the archives of the health industry. Finally, for assessing the public image of stroke, fictional literature [ 9 , 10 ] as well as films, music and artwork constitute very important repositories.
Why bother with all this theoretical stuff? It is important to understand that there will never be a single, all-encompassing history of stroke. There will only be various histories characterized by one or the other perspective and one or the other objective. This assertion is supported by a brief look at the number of available sources [Fig. 2 ]. Whereas the study of medical writings from antiquity, Middle Ages and Early Modern Times is manageable, no single historian will ever be able to read more than a minute part of the materials produced after 1800.
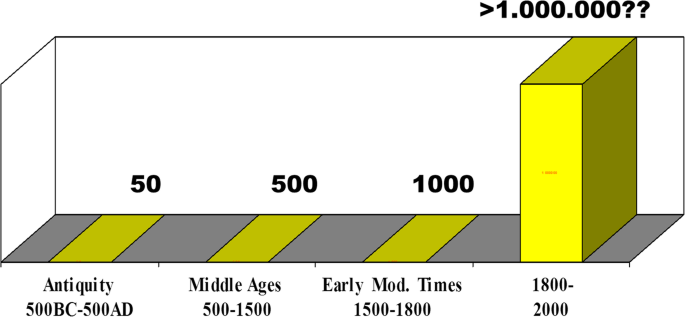
Estimated numbers of medical sources in the history of stroke across centuries. Drawing by the author
An outline of the history of stroke usually begins with the Greco-Roman civilization [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ]. It is, however, less conventional to follow the Socratic method based on the premise that one lived in a time of complete ignorance.
In antiquity, there were no dissections and no experiments besides some remarkable exceptions. The system of blood circulation was unknown, and regarding early antiquity no distinction could be made between arteries and veins. There was no consensus whether the brain or the heart was the instrumental organ for motor and sensory activities: whereas Plato, and most of the Hippocratic authors and Galen insisted on the brain [ 19 ], Aristotle and the physician-philosophers of the Stoic and Epicurean school favoured the heart [ 20 , 21 ] – for good reasons, by the way.
Nevertheless, the ancients came up with many insights worth mentioning today. First, they produced descriptions of the disease such as: “Pain suddenly seizes the head in a healthy person, and he at once becomes speechless … and gapes with his mouth” [ 22 ]. In a further Hippocratic writing, one can read: “In apoplexy, drowsiness befalls this patient, he is senseless … mild fever is present, and his body is powerless. He dies on the third or fifth day, and generally does not reach the seventh” [ 23 ]. The authors of these statements did not use the word stroke, but apoplexy, which was the preferred medical term to label stroke-like conditions up to 1800 [ 24 , 25 , 26 ]. The explanation for its use is simple. Many early civilizations were convinced that acute diseases with loss of consciousness were sent by the gods. In Homeric Greek, some four centuries before Hippocratic physicians appeared on the scene, stroke meant “plex” or “plexy” and god meant “theos” or “dios”. Thus “theoplexy” or “dioplex” were common denominations for stroke, and apoplexy is nothing but a secularized version for a “very severe blow”. The definitions mentioned above and the etymology of the word make it clear that the ancient term “apoplexy” and its modern sequel “stroke” are all but equivalent. Apoplexy is an umbrella term under which one can easily summarize what we today call stroke, but one can also subsume myocardial infarction or pulmonary embolism triggering disturbances of consciousness.
Secondly, the Greeks realized that apoplexy was characterized by a different set of symptoms and a different course in comparison to various other medical conditions they called epilepsy, catalepsy, lethargy etc. [ 27 ]. Thirdly, ancient physicians wrote at length about treatment and prognostics including the world famous aphorism “It’s impossible to cure a violent attack of apoplexy, and difficult to cure a mild one” [ 28 ]. Finally, they set ethical standards how patients should be treated which did not change very much until today in many parts of the world.
But how did Greco-Roman physicians explain the disease? Now it’s time to remember the “strange object approach”. Galen, a Greek physician practising and writing around the year 200 of our era in Rome, developed the idea that a vital spirit built in the heart was carried towards the brain via the arteries. In a structure called retiform plexus (which he found in several animal species in the region around the pituitary gland) this vital spirit was then transformed into the so-called animal spirit. Only the animal spirit was stored in the cerebral ventricles from where it acted on demand as a “fuel” for the transmission of motor impulses and sensory data to the periphery. That’s, in a nutshell, how the brain worked according to Galen [ 29 ].
In individuals with apoplexy, a noxious humour called phlegm accumulated in the body: “When the vessels drew phlegm into themselves, the blood must, on account of the coldness of the phlegm, stand more still than before and be cooled, and so, with the blood immobile, it is impossible for the body not to become still and numb … But if the phlegm predominates, the blood is cooled and congeals more, and if it reaches a certain stage of cooling and congelation, it congeals completely, the person becomes cold, and he dies” [ 22 ]. The accumulation of noxious mucus thus blocked the flow of the animal spirit, and the blockage eventually resulted in palsies, sensory dysfunctions, loss of consciousness, and possibly death [Fig. 3 ]. Phlegm was a cold, moist and viscous fluid which could accumulate in the brain when the body was exposed to too much cold, e.g. during the winter, in old age etc. [ 30 ]. This theory was the fundamental etiological doctrine of stroke and other brain diseases which dominated European thinking for 1500 years. No text on brain disorders up to 1750 can be understood without a solid knowledge of these principles.
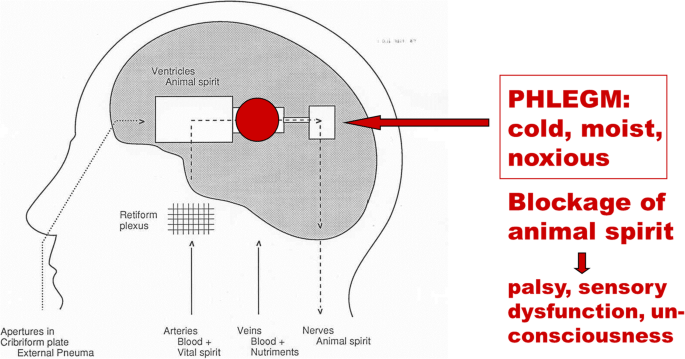
Galen’s doctrine of apoplexy. Drawing by the author
This doctrine was also the basis for various therapeutic actions. A practising physician and adherent of this teaching had two basic options: either evacuation – meaning “cleansing brain and body” in order to get rid of the superfluous fluid, or counter-action – i. e. applying something hot and dry to combat the cold and moist humour. Evacuation and counter-action are two of the major meta-strategies of medical treatment until today. If one adds the four major realms of pre-1800 treatment – physical therapy, dietetics, herbal pharmacology and surgery – a wide spectrum of therapeutic measures is available, ranging from hot bathing to various surgical procedures including cauterization [ 31 ].
So what we see in ancient times is a rational, but speculative explanation of symptoms. This explanation was only loosely tied to the observation of nature, focused on “hidden causes” of disease but deeply embedded in ancient philosophy. Harmony between man and world, and harmony between the various parts of the body were its key principles. It is this holistic approach which makes certain aspects of ancient medicine still attractive for a couple of contemporary physicians representing alternative forms of medicine [ 19 ].
The medieval period
Between 500 and 1500 Galen’s brain-centred doctrine of neuropsychiatric symptoms was important, but it was, as mentioned before, not the only one. Aristotle and his followers had propagated a powerful cardiocentric theory: a teaching based on the assumption that the origins of motion, sensation and consciousness were located in the heart. “Tell me where is fancy bread, or in the heart or in the head”: with regard to stroke this question formulated by William Shakespeare centuries later was the neurological hotspot around the year 1000 [ 32 ]. Especially the best physician-philosophers of the rising Islamic civilization tried to reconcile both doctrines. Rhazes and Avicenna (ar-Razi and ibn-Sina) felt that Aristotle as well as Galen had good arguments [ 33 ]. From the eleventh century on, the issue was transferred from Bagdad and Cairo to the Latin West, to the emerging centres of learning in Italy, Spain, France, England, and finally the German speaking territories. Since there were still no dissections or experiments at hand, the problem couldn’t be solved in a modern way. But it was solved in a medieval way: by playing with words and quoting authorities. There are about a dozen truly scholastic texts on stroke, full of arguments and counter-arguments, pseudo-problems and pseudo-answers [ 32 ]. A folio page of a writing by the Italian physician-philosopher Pietro d’Abano [Fig. 4 ] [ 34 , 35 ], who taught in Padova in the early fourteenth century, provides insight into these sophisticated discussions and their fruitlessness from the patient’s point of view. By the way: the final medieval solution of the brain-heart-issue was to emphasize that a stroke began in the brain but terminated in the heart. This solution was accepted until the seventeenth century.
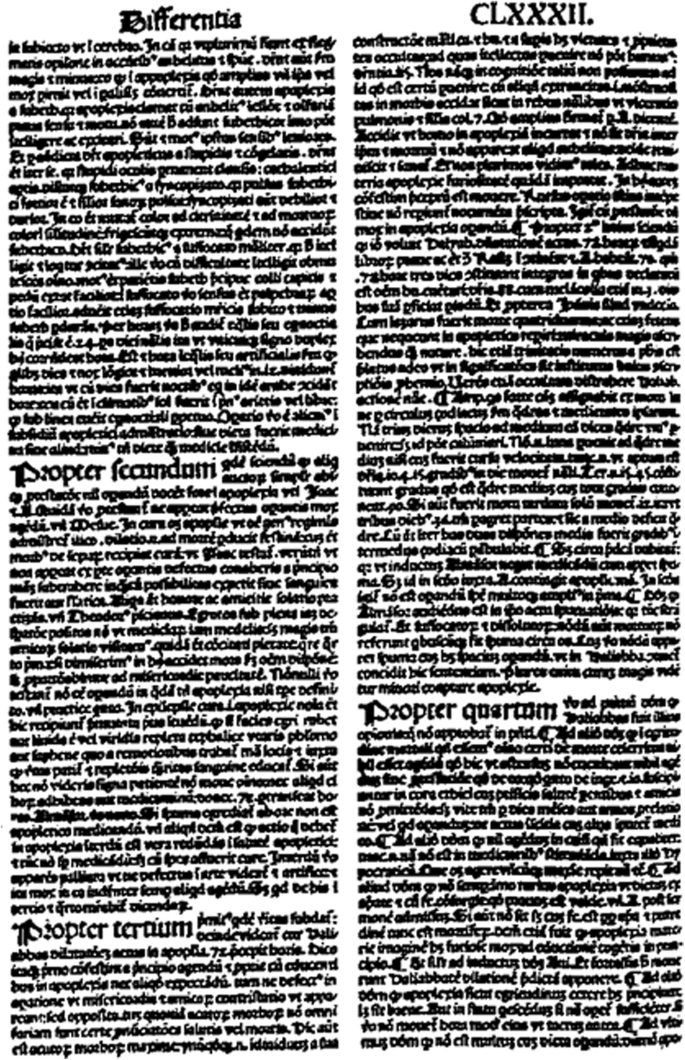
Folio page from Pietro d’Abano’s Conciliator (1496). With permission of the University and City Library of Cologne
Another “highlight” of the medieval era is the occurrence of miracles and patron saints. Early examples of faith healing in stroke and other medical conditions can be found in the Byzantine Empire, later ones in the Latin West and the Orthodox church of the East. These documents are ranking among the most important sources that have come down to us from these centuries. To quote just one miracle story which took place in Italy around the year 1250 in a Franciscan monastery, about one generation after St. Francis died:
“A certain young man … was subjected to a terrible fright that provoked mental confusion and paralysis of the right side of the body. Through his severe illness, he also lost hearing and the movement and sensation of the tongue. He had been confined to bed for some day in this pitiful state … One morning St. Francis appeared in the infirmary … stretched out his hand, running it lightly over the novice’s right side from head to foot, touching him gently, and placed his fingers in the young man’s ears, saying: ‘This shall be for you a sign that God has through me … completely restored your health’. With these words … the young man arose and entered the church with his health of body and mind, to the great astonishment of the brothers” [ 36 ].
This “case report” can be analysed in various ways [ 37 ]. A contemporary neurologist may think of a reversible ischemic neurological deficit or a psychogenic condition. A historian will certainly look for the theological and literary context. It is all but easy to arrive at a satisfactory conclusion here, also because this trove of miracle cures is largely unexplored yet.
A closing remark about stroke and religious healing in the Middle Ages. For epileptics, there were more than a dozen patron saints which could be addressed for prevention and/or cure of the illness [ 38 ]. For apoplectics, there was none. St. Wolfgang and St. Andreas Avellino only had a minor local significance [ 39 ]. For the scholar studying medieval medicine this shortage is quite surprising, and of course such a negative result needs an explanation. It certainly has to do with the high fatality rate of stroke: Patron Saints are no emergency room. But it may also be linked to the high rate of post-stroke disabilities hindering victims to travel to a place of pilgrimage. On the other hand, there was definitely a lack of commercial interest on the part of these places of pilgrimage – one of the first “management mechanisms” in the care of stroke patients.
Books and chapters about medicine in the Renaissance often use the metaphor of a “wind of change”, alluding to a fresh breeze blowing constantly over the European continent and sweeping away the medieval dust. But is that really true? As far as the history of stroke is concerned: yes, and no.
Following the first anatomical dissections of human bodies around 1300, from 1450 onward an increasing number of post-mortem examinations were carried out, leading to a better knowledge of brain anatomy and brain vasculature. About a century later, the first autopsies were performed in order to discover bodily changes in certain diseases: pathological anatomy was born. And in 1628 William Harvey used a variety of sophisticated experiments to prove that there is really something like a circulation of the blood, a circulation through the whole body including the head and the brain. New methods, revolutionary findings: but their significance for the understanding of stroke was practically zero, at least at the beginning.
In 1602, the Swiss physician Felix Platter carried out a brain autopsy after the death of one of his stroke patients. He summarized his findings of the post-mortem with the following words:“ a phlegmatic humour is obstructing the inner passages of the brain” [ 40 ]. This short statement highlights two pivotal insights that the study of historical diseases provides. First: every scientific observation is theory-laden, then and now. Second: obviously it is very difficult to get rid of traditional beliefs. Platter and practically all of his colleagues [ 41 , 42 , 43 , 44 ] subscribed to Galen’s age-old idea that apoplexy was caused by phlegm in the cerebral ventricles. And what did brain autopsy reveal: phlegm in the cerebral cavities.
Yet brain autopsies plus the idea of a circulation marked the end of the pre-modern era of stroke. A true figure of transition was another Swiss physician named.
Johann Jakob Wepfer, who authored one of the most famous monographs on stroke of all times [Fig. 5 ]. For a long time, clinicians tended to classify Wepfer as a modernist and true reformer, for a couple of good reasons. With his research apoplexy became a cerebrovascular disorder. Moreover, he was convinced that the pathological changes were located in the cerebral substance and not in the ventricles. He also gave the hitherto most precise description of the encephalic arteries including the circle of Willis. In this context, Wepfer discovered during his dissections “pituitous formations” in brain arteries and hypothesized that these formations (clots?) play an important role in stroke. In addition, he found a hemorrhage in about 50% of the brains of stroke victims, thus proving that the rupture of a cerebral artery is responsible for the subsequent attack [ 45 ]. Wepfer was therefore praised as one of the harbingers of modern medicine [ 46 , 47 , 48 , 49 ]. However, a careful reading of his 400-pages book [ 50 , 51 , 52 ] – a tedious task, because it is written in a difficult Latin – leads to striking results. Wepfer was a modernist, but at the same time still also a true follower of Galen with more than old-fashioned ideas on cerebral physiology and the etiology of stroke. According to him, the obstruction of brain arteries was harmful because the little clots blocked the flow of the vital spirit from the heart to the brain. A hemorrhage in the brain was disastrous because the animal spirit couldn’t flow freely towards the spinal cord and the nerves, and so on. Basically, Wepfer’s concept of stroke was still an ancient one dealing with humours and spirits, only supplemented by the latest anatomical and pathoanatomical discoveries.
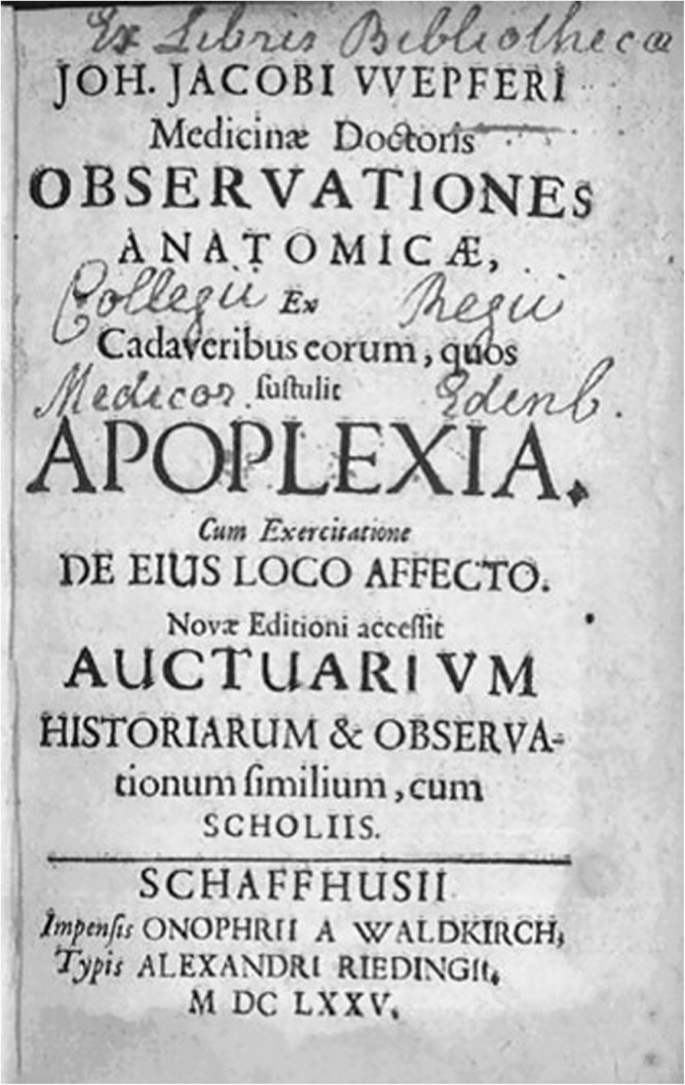
Title page of Wepfer’s 1658 monograph on stroke. New edition 1675. With permission of the Institute for the History of Medicine and Medical Ethics, University of Cologne
The modern era
The decisive difference between the pre-1800 and the modern period in the history of stroke is therefore not to be found in a single discovery or a set of new methods, but in a change of the basic notion of what a disease is [ 53 ]. From Galen to Wepfer, stroke (like many other neurological conditions) was defined as a collection of certain symptoms. With the beginning of the nineteenth century, however, stroke is for the first time defined as a result of a lesion. The morphological lesion, and only the morphological lesion, became the decisive criterion for an operational definition of stroke; the symptoms were now only seen as “indicatory signs”. Henceforth morbid anatomy, and nothing but morbid anatomy, became the key basis of all knowledge about stroke.
The birth of this new way of perceiving a disease is inseparably linked to the Paris school of medicine. Therefore, it is no surprise that the first truly modern definition of stroke is to be found in a French publication. In 1812, the young physician Jean-André Rochoux [ 54 ] produced what can be called the most important dissertation in the history of neurology [Fig. 6 ]. His text started with a phrase that is a platitude today, but indicated a scientific revolution when it was printed: “Apoplexy is a hemorrhage of the brain, by rupture, with more or less serious alteration of its substance” [ 55 ]. First Rochoux explained the lesion, its size, colour and location, then traced the signs and course of stroke, and concluded with a few remarks on treatment and prognosis. Undoubtedly, his dissertation and the monograph he produced 2 years later [ 56 ] are the first modern texts on stroke.
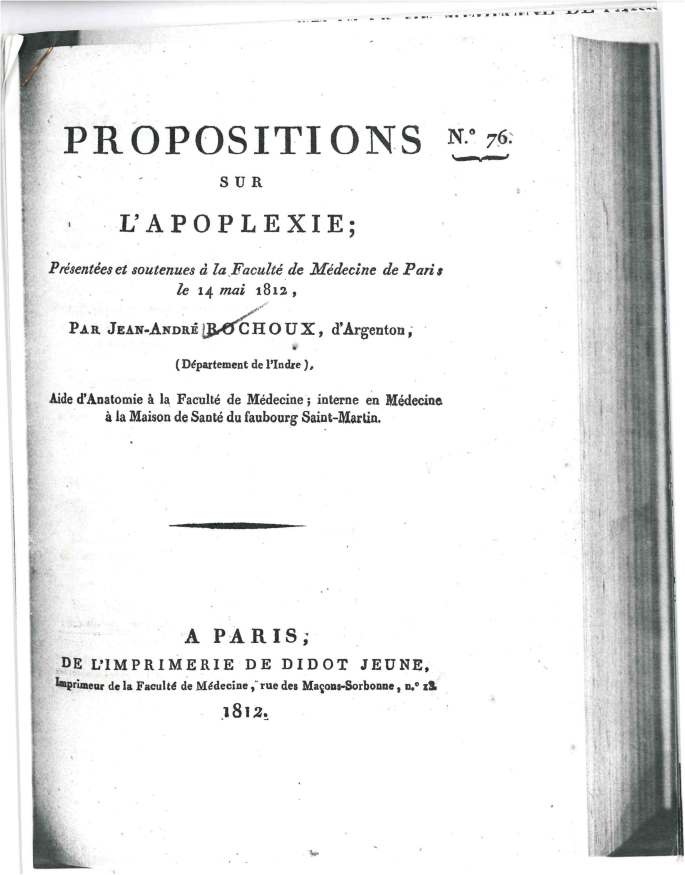
Title page of Rochoux’ 1812 dissertation on cerebral hemorrhage. With permission of the Institute for the History of Medicine and Medical Ethics, University of Cologne
But Rochoux’ thorough exposition remained not the only one. In the very same decade, another young French doctor by the name of Léon Rostan came up with the idea that stroke must be the result of a softening of the brain (“ramollissement du cerveau”) [ 57 ]. In modern terms: ischemic infarction of the brain. Thus by 1820, the two basic modern concepts of stroke had been discovered. They were both offspring from the anatomico-clinical method, i. e. the comparison of post-mortem lesions with in-vivo symptoms. They were both found through hospital-based research and grounded on statistical observations. What followed during the whole 19th and a good part of the twentieth century was nothing but a refinement of these two basic concepts. Therefore, one can now really talk about progress and milestones: for example, the discoveries made by Rudolf Virchow who described, starting in 1846, arterial thrombosis and embolism and recognized the interaction between blood and arterial wall. Furthermore, the Berlin pathologist clearly showed that vascular occlusions caused infarction [ 58 ]. Again, this is a triviality today, but was a matter of acrimonious scientific debates in the 1840s.
From the mid-nineteenth century onwards, medicine as a branch of knowledge was inextricably linked to the natural sciences. “No other theory as that of facts” was the positivistic credo of the epoch. A prominent German clinician put it even more bluntly: “Medicine will either be science or cease to exist”. Research on stroke profitted enormously from this positivistic movement. An increasing number of physicians, some of them specialized in neurology, contributed to the rapidly growing treasure of knowledge [ 59 , 60 , 61 , 62 ]. It is impossible to enumerate all the important contributions, but one can at least emphasize some historical trends. From 1850 to 1930, vascular anatomy and clinical-anatomical correlations were of special interest, including various brain stem lesions. Between the 1920s and the 1970s, the pathophysiology of vascular lesions reached its hey-day including figures like the Frenchman Charles Foix, Kapitoline Wolkoff from St. Petersburg, and the Canadian Charles Miller-Fisher [ 13 ].
From about 1975 onwards, research on risk factors, stroke registries, randomized trials, databases, as well as a general momentum for “new treatments” can be observed [ 63 ]. So by the end of the twentieth century, stroke medicine became a subspecialty of neurology, theoretically as well as practically. And another important fact should be emphasized: For the first time, treatment of stroke was characterized by what one can call “limited therapeutic optimism” [ 64 ]. To a large extent, however, this evolution was due to the technical development of diagnostics: the history of twentieth-century medicine is essentially a history of technology. In the case of neurology, new technologies were available almost every decade, from hands-on spinal tap around 1900 to the most sophisticated brain visualizations 100 years later [ 65 ]. Sometimes it was even difficult for the doctor’s brains to keep up with the speed of technical innovation. But what is certain is that the history of stroke in the twentieth century remains to be written.
Conclusions
What are the take home messages of this historical tour?
It is a matter of personal taste if one likes the allegory of the dwarfs standing on the shoulders of giants. However, knowledge about the history of one’s own field almost automatically leads to professional and personal modesty, which is always a good attitude, especially for physicians.
An intellectual tour through history may raise the awareness of how intimately we are connected to the intellectual, technical, and social context of our own epoch – we may or may not realize this frame. Galen, Wepfer, Rochoux, Rostan, Virchow and all the other important figures in the history of stroke: they were all products of their times sharing certain opportunities and certain limits – and so are we.
Perhaps the most valuable insight gained is that “unthinking” ideas of the past can be a key to great scientific success. The modern era in the history of stroke only came true because physicians of the early nineteenth century “unthought” all the misleading and constrictive presumptions which had been around for centuries. A fundamental conclusion therefore is: You can change history, yes you can!
This essay shall be concluded with an encouraging quote from the French poet André Gide expressing the very same idea in a much more elegant way:
“One does not discover new continents without consenting to lose sight of the shore for a very long time” [ 66 ].
Availability of data and materials
Not applicable.
Dumesnil, R., & Schadewaldt, H. (1970). Die berühmten Ärzte . Köln: Aulis Verlag Deubner & Co.
Google Scholar
Rosenberg, C. (1992). Framing disease . New Brunswick: Rutgers University Press.
World Health Organization (2018). The top 10 causes of death. Resource document . Geneva: WHO https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death . Accessed 10 May 2007.
Feigin, V. L., Forouzanfar, M. H., Krishnamurthi, R., Mensah, G. A., Connor, M., Bennett, D. A., et al. (2014). Global and regional burden of stroke during 1990–2010: findings from the global burden of disease study 2010. The Lancet , 383 , 245–254.
Karenberg, A., & Leitz, C. (2001). Headache in magical and medical papyri of ancient Egypt. Cephalalgia , 21 (9), 911–916.
CAS PubMed Google Scholar
Zimmermann, M. (2012). Narrating stroke: the life-writing and fiction of brain damage. Medical Humanities , 38 , 73–77.
PubMed Google Scholar
Moreno-Martinez, J. M., & Fernandez-Armayor, V. (2002). História e transcendência social da patologia vascular cerebral. Revista de Neurologia , 34 (11), 1092–1094.
Popovich, J. M. (2007). Coping with stroke: Psychological and social dimensions in U.S. patients. The International Journal of Psychiatric Nursing Research , 12 (3), 1474–1487.
Karenberg, A. (2011). Der Schlaganfall in der Literatur. In D. Schlaganfall-Gesellschaft (Ed.), 10 Jahre Deutsche Schlaganfall-Gesellschaft , (pp. 104–109). Berlin: Privatdruck.
Fischbein, M. (1965). Strokes. 1. Some literary descriptions. Postgraduate Medicine , 37 , A194–A198.
McHenry, L. C. (1981). A history of stroke. International Journal of Neurology , 18 (3–4), 314–326.
Gawel, M. (1982). The development of concepts concerning cerebral circulation. In F. C. Rose, & W. F. Bynum (Eds.), Historical aspects of the neurosciences , (pp. 171–178). New York: Raven Press.
Fields, W. S., & Lemak, N. A. (1989). A history of stroke. Its recognition and treatment . New York: Oxford University Press.
Quest, D. Q. (1990). Stroke: a selective history. Neurosurgery , 27 (3), 440–445.
Dening, T. R. (1995). Stroke and vascular disorders. In G. E. Berrios, & R. Porter (Eds.), A history of clinical psychiatry , (pp. 72–85). London: Athlone.
Heckmann, J. G., Erbguth, F. J., Hilz, M. J., Lang, C. J. G., & Neundörfer, B. (2001). Die Hirndurchblutung aus klinischer Sicht. Historischer Überblick, Physiologie, Pathophysiologie, diagnostische und therapeutische Aspekte. Medizinische Klinik , 96 (10), 583–592.
Warlow, C., van Gijn, J., Dennis, M., Wardlaw, J., Bamford, J., Hankey, G.,Sandercock, P., Rinkel, G., Langhorne, P., Sudlow, C, Rothwell, P. (2008). Development of knowledge about cerebrovascular disease. In: C. Warlow, J. Van Gijn et al. (Eds.). Stroke: practical management. 3rd ed.(pp. 7–34). Oxford: Blackwell.
Storey, C. E., & Pols, H. (2010). A history of cerebrovascular disease. In S. Finger, F. Boller, & K. L. Tyler (Eds.), History of neurology , (pp. 401–415). Edinburgh: Elsevier [Handbook of clinical neurology, 95].
Rose, F. C. (1994). The neurology of ancient Greece – an overview. Journal of the History of the Neurosciences , 3 (4), 237–260.
Finger, S. (1994). Origins of neuroscience. A history of exploration into brain function . Oxford: Oxford University Press.
Moog, F. P., & Karenberg, A. (2006). Aristotle on stroke. Sudhoffs Archiv , 90 (1), 123–124.
Hippocrates, Vol. V (1987). Diseases II. With an English translation by P. Potter . Cambridge: William Heinemann [The Loeb Classical Library, 472].
Hippocrates, Vol. VI (1988). Diseases III. With an English translation by P. Potter . Cambridge: William Heinemann [The Loeb Classical Library, 473].
Clarke, E. (1963). Apoplexy in the Hippocratic writings. Bulletin of the History of Medicine , 37 (4), 301–314.
Pound, P., Bury, M., & Ebrahim, S. (1997). From apoplexy to stroke. Age and Ageing , 26 , 331–337.
Patsioti, J. G., & Rose, F. C. (1995). What did the Greeks mean? Journal of the History of the Neurosciences , 4 (1), 67–76.
Moog, F. P., & Karenberg, A. (1997). Die Apoplexie im medizinischen Schrifttum der Antike. Fortschritte der Neurologie-Psychiatrie , 65 , 489–503.
Hippocrates, Vol. IV (1959). Aphorisms. With an English translation by W.H.S. Jones . Cambridge: William Heinemann [The Loeb Classical Library].
Rocca, J. (2003). Galen on the brain. Anatomical knowledge and physiological speculation the second century AD . Leiden: Brill.
Karenberg, A. (1994). Reconstructing a doctrine: Galen on apoplexy. Journal of the History of the Neurosciences , 3 , 85–101.
Karenberg, A. (1999). “Einen schweren Schlaganfall zu heilen ist unmöglich, einen leichten nicht einfach”. Zur Therapie der Apoplexie im medizinischen Schrifttum der Antike. In: J. M. Ternes (Ed.), La thérapeutique dans l’Antiquité. Pourquoi? Jusqu’où? (pp. 61-78). Luxemburg: Études luxembourgoises d’histoire et de littérature romaine, 3.
Karenberg, A., & Hort, I. (1998). Medieval descriptions and doctrines of stroke: Preliminary analysis of select sources, part I-III. Journal of the History of the Neurosciences , 7 (3), 162–200.
Karenberg, A., & Hort, C. (1999). Zwischen Galenismus und Aristotelismus: Der Schlaganfall in der islamischen Medizin des Mittelalters. Schriftenreihe der Deutschen Gesellschaft für Geschichte der Nervenheilkunde , 5 , 109–118.
Pietro d’Abano (1496). Conciliator differentiarum philosophorum et praecipue Medicorum … Venetiis, Bonetus Locatellus.
Paschetto, E. (1984). Pietro d’Abano medico e filosofo . Firenze: Nuovedizioni Enrico Vallecchi.
Analecta Franciscana, Tomus X (1941). Legendae S. Francisci Assisiensis saeculis XIII et XIV conscriptae … Fasciculus V: S. Bonaventura, Doctor Seraphicus, Legenda maior et Legenda minor S. Francisci … Ad Clara Aquas (Quaracchi): Typographia Coll. S. bonaventura e.
Moog, F. P., & Karenberg, A. (2003a). St. Francis came at dawn – The miracolous recovery of a hemiplegic monk in the middle ages. Journal of the Neurological Sciences , 213 , 15–17.
Frey, E. F. (1979). Saints in medical history. Clio Medica , 14 (1), 35–70.
Moog, F. P., & Karenberg, A. (2003b). Heilige als Patrone gegen den Schlaganfall. Early Science and Medicine , 8 , 196–209.
Platter F (1662). Praxeos seu de cognoscendis, praedicendis, praecavendis curandisque affectibus homini incommodantibus tractatus tres . Basel 1602-1608. Translated into English under the title: A Golden Practice of Physick . London: Peter Cole.
Coturri, E. (1971). La malattia apoplettica nel pensiero die G. B. Morgagni. In: Atti del 21. Congresso Nazionale di Storia della Medicina , Taranto-Bari, 1969 (pp. 324-329). Roma.
Jarcho, S. (1980). Some lost, obsolete, or discontinued diseases: serous apoplexy, incubus, and retrocedent ailments. Transactions and Studies of the College of Physicians of Philadelphia , 2 (4), 241–266.
Schutta, H. S. (2006). Seventeenth century concepts of “apoplexy” as reflected in Bonet’s “Sepulchretum”. Journal of the History of the Neurosciences , 15 (3), 250–268.
Schutta, H. S. (2009). Morgagni on apoplexy in De Sedibus: a historical perspective. Journal of the History of the Neurosciences , 18 (1), 1–24.
Wepfer, J. J. (1658). Observationes anatomicae, ex cadaverum eorum, quos sustulit apoplexia. Cum exercitatione de eius loco affecto . Schafhusii: Typis J.C. Suteri.
Donley, J. E. (1909). John James Wepfer, a renaissance student of apoplexy. Bulletin of the Johns Hopkins Hospital , 20 , 1–9.
Fischer, H. (1931). Johann Jakob Wepfer (1620–1695). Ein Beitrag zur Medizingeschichte des 17. Jahrhunderts . Zürich: Rudolf.
Major, R. H. (1978). Classic descriptions of disease , (3rd ed., ). Springfield: Charles C. Thomas.
Gurdjian, E. S., & Gurdjian, E. S. (1979). History of occlusive cerebrovascular disease. I. From Wepfer to Moniz. Archives of Neurology , 36 , 340–343.
Karenberg, A. (1998). Johann Jakob Wepfers Buch über die Apoplexie (1658). Kritische Anmerkungen zu einem Klassiker der Neurologie. Nervenarzt , 69 , 93–98.
Mani, N. (1978). Pathogenese, Diagnose und Prognose der Apoplexie bei Johann Jakob Wepfer (1658). In C. Habrich, F. Marguth, & J. H. Wolf (Eds.), Medizinische Diagnostik in Geschichte und Gegenwart. Festschrift für Heinz Goerke zum sechzigsten Geburtstag , (pp. 235–239). München: Fritsch.
Mani, N. (1982). Biomedical thought in Glisson’s hepatology and in Wepfer’s work on apoplexy. In L. G. Stevenson (Ed.), A celebration of medical history , (pp. 37–68). Baltimore: The Johns Hopkins Press.
Foucault, M. (1963). Naissance de la clinique: Une archéologie du regard médical . Paris: Presses universitaires de France.
Walusinski, O. (2017). Jean-André Rochoux (1787-1952), a physician philosopher at the dawn of vascular neurology. Revue Neurologique (Paris) , 173 (9), 532–541.
CAS Google Scholar
Rochoux, J.-A. (1812). Propositions sur l’apoplexie. Thesis no. 76 . Paris: De l’Imprimerie de Didot jeune.
Rochoux, J.-A. (1814). Recherches sur l’apoplexie . Paris: Méquignon-Marvis.
Poirier, J., & Derouesné, C. (2000). La neurologie à l’Assistance Publique et en particulier à la Salpêtrière avant Charcot. L’exemple de Rostan et du ramollissement cérébral. Revue Neurologique (Paris) , 156 (6-7), 607–615.
Schiller, F. (1970). Concepts of stroke before and after Virchow. Bulletin of the History of Medicine , 14 (2), 115–131.
Paciaroni, M., & Bogousslavsky, J. (2009). How did stroke become of interest to neurologists? A slow 19th century saga. Neurology , 73 , 724–728.
Bruetsch, W. L. (1971). Richard Bright (1789-1858) and apoplexy. Transactions of the American Neurological Association , 96 , 213–215.
Schutta, H. S. (2017). Richard Bright’s observations on diseases of the nervous system due to inflammation. Journal of the History of the Neurosciences , 27 (2), 165–185.
Engelhardt, E. (2017). Apoplexy, cerebrovascular disease, and stroke: Historical evolution of terms and definitions. Dement Neuropsychology , 11 (4), 449–453.
Caplan, L. R. (2004). Cerebrovascular disease: historical background, with an eye to the future. Cleveland Clinic Journal of Medicine , 71 (suppl. 1), 822–824.
Licht, S. (1973). Stroke: a history of its rehabilitation. Archives of Physical Medicine and Rehabilitation , 54 , 10–18.
Karenberg, A. (2008). Von der Traumdeutung zum Neuroenhancement. Die Entwicklung der Nervenheilkunde. In D. Groß, & H. J. Winckelmann (Eds.), Medizin im 20. Jahrhundert , (pp. 60–77). Redd Business Information: München.
Gide, A. (1925). Les faux-monnayeurs . Paris: Gallimard.
Download references
Acknowledgements
No funding.
Author information
Authors and affiliations.
Institute for the History of Medicine and Medical Ethics, Medical Faculty, University Hospital Cologne, University of Cologne, Joseph-Stelzmann-Str. 20, 50931, Köln, Germany
Axel Karenberg
You can also search for this author in PubMed Google Scholar
Contributions
It’s a one-author paper. The author(s) read and approved the final manuscript.
Author’s information
The author is Specialist for Neurology and Specialist for Psychiatry as well as Professor of the History of Medicine.
Corresponding author
Correspondence to Axel Karenberg .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The author declares that he has no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Karenberg, A. Historic review: select chapters of a history of stroke. Neurol. Res. Pract. 2 , 34 (2020). https://doi.org/10.1186/s42466-020-00082-0
Download citation
Received : 22 May 2020
Accepted : 22 July 2020
Published : 01 December 2020
DOI : https://doi.org/10.1186/s42466-020-00082-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Stroke/history
- Cerebrovascular disorders/history
- Intracranial hemorrhages/history
- Paralysis/history
- Neurology/history
- Stroke/pathology
- Historical article
Neurological Research and Practice
ISSN: 2524-3489
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Can You Fly After a Stroke?
by Flying Angels Editorial Team | Jun 22, 2020 | News & Resources

Many stroke survivors worry about if and when they can fly after a stroke. Medical research shows a person can fly after a stroke, but they should consider the type of stroke they had, how long it’s been since the stroke and whether they want medical travel assistance during the flight.
If you plan to travel after having a stroke, it’s comforting to know that research has found having a history of a stroke does not put a person in danger during an airline flight. Having a past stroke does not mean a person should not fly.
But if a stroke has been more recent or a person simply has concerns about flying, they should consider several factors before booking their trip.
Can I Hire a Nurse to Fly With Me?
Factors For Flying After a Stroke
Strokes vary in type and severity. Stroke victims should consider their own unique circumstances. Experts do not have hard and fast rules that apply to everyone who has had a stroke. But the following factors can help you decide about flying.
Type of Stroke
The advice on when to fly could depend on the stroke. A full stroke involves the sudden loss of blood flow to the brain. However, many people experience a transient ischemic attack (TIA), which is known as a “mini-stroke” that resolves without permanent brain damage.
A TIA is like a stroke and considered a warning sign of stroke risk. Also, some medical disorders that lead to a TIA could pose a “very small risk” on flights, according to research compiled by Very Well Health. Those conditions include patent foramen ovale, paradoxical embolism or hypercoagulability. It’s important to know if you have those conditions.
Get Help Leaving the Hospital After Discharge
Timing of Stroke
Experts may vary on when they recommend you can fly. The Stroke Association recommends that it is “probably best to avoid flying for the first two weeks. This is the time when your problems are likely to be most severe and other conditions related to your stroke may come up.”
In the most severe stroke cases, patients may want to wait as long as three months. However, with a TIA, many people are safe to fly in 10 days.
Before booking a flight, people should consult with their doctor.
Long Distance Medical Transport Cost
Medical Assistance For A Flight
Some people who have had a stroke may prefer to hire medical professionals to fly with them. Doing so provides them a high degree of security in making the flight and ensures they get proper medical care if needed. Such help is found with non-emergency transport (NEMT) companies like Flying Angels.
Flying Angels provides a number of services that can support stroke victims when they fly. A Flight Coordinator books your flight, sets up all the arrangements with both airports and airlines, gets you through security and provides a flight nurse to help you throughout your journey. The company hires only nurses with a great deal of experience working in emergency rooms and who have training in providing medical care at high altitudes.
Medical Transportation Options Explained
Stroke survivors may face challenges, but they still can live a full life. As with any serious condition, those who have had a stroke need to practice patience and planning. Travel by flight is certainly doable if they have the right amount of support. Consulting with a doctor and a medical transport service can give people the answers they seek about flying after a stroke. They also can provide the comfort, care and support they need to make the journey.
Popular Articles
- International Patient Transport: A Compassionate Solution for Returning Patients Home
- The Role of NEMT in Patient Centered Care for Long Distance Transfers
- Hiring a Medical Escort: Essential Questions and Guidance
- https://www.facebook.com/FlyingAngelsInc/
- https://www.linkedin.com/company/flying-angels/

Travelling after stroke
Everyone needs a holiday! It is good for your mind and body to rest and relax!
You may not be thinking about travelling immediately after your stroke but at some point you may consider taking a holiday. You may want to travel for rest and relaxation, to see new places, or visit family and friends.
Your doctor will let you know if it is safe for you to travel. Your healthcare team can also give you some tips to make travelling easier.
What do I need to know for traveling after stroke?
Considering your needs and planning ahead can help you have a safe and enjoyable holiday. It may be helpful to speak with your health care team for suggestions to make travel easier.
Learn from the experience of others. You can get ideas and suggestions from other people who have had strokes about what has worked well for them while travelling. For example, you may find answers to your travel questions at a peer support group or online.
Here are some things to consider when looking for a place to stay:
- Accessible bathroom. They offer grab-bars and toilet seats
- Elevator If there is no elevator, ask for a room on the ground floor
- Restaurants nearby. Stay in places that are close to things to do
- See online photos of the hotel. This helps you decide what you will need to bring
- Call and ask questions before you book your room
You may consider:
- Taking your own chair. Bring a folding cane-seat or a rollator if you can only walk short distances. Chairs or benches may not always be available when you need to take a break
- Renting a wheelchair or scooter. If you need to travel a long way
What are some tips for riding on an airplane?
- Choose a non-stop flight. If you have to make a connection, try to get more time between flights. Call the airport to find out how far you need to go to get the connecting flight
- Choose an aisle seat. This helps to give you a bit more room.
- Use a carry-on. Use a shoulder bag or back pack. Pack it with basic toiletries, medications, and travel information
- Wear shoes that are easy to take on and off. This makes security checks easier
- Travel with someone. It helps to travel with someone who can help you
Here are some tips at the airport:
- Check-in as much luggage as you can. This means less to carry
- Give yourself extra time.
- Use early boarding. Flight attendants can help you board the plane if you are using a cane or wheelchair
- Use an airport rental cart. It is often easier to push one cart than manage many bags
Tips for travelling with aphasia:
Write down all your travel information. If you have aphasia you can show the airline personnel or the taxi driver the information, so they know how to direct you. Have all important addresses and phone numbers in your notebook.
Having read the information in this section, consider the following questions.
- Do I know if it is safe for me to travel after my stroke?
- Is it safe for me to travel by car, train, boat or plane?
- Is there anything specific I need to be aware of when travelling after a stroke (for example: precautions, medications, vaccinations)?
- Do I know how to plan a safe trip?
- Can I make sure that my needs will be met at my destination (for example, equipment and accessibility needs)?
- Do I need to call ahead before I leave to ensure things are in place at my destination?
- Do I have travel insurance?
- As a caregiver, do I know what to do if something happens while we are away from home?
Where to get more information, help and support:
Ten Travel Tips for Stroke Survivors

Travel and Heart Disease

Travel precautions help people with heart disease
Traveling to a faraway place doesn’t need to be off limits because you have heart disease or are a caretaker of someone who has had a cardiac event like heart attack or stroke . A few simple precautions can help make your trip smooth.
Here are some travel tips:
- Keep medicines in their original, labeled containers. Ensure that they are clearly labeled with your full name, health care professional’s name, generic and brand name and exact dosage.
- Bring copies of all written prescriptions. Leave a copy of your prescriptions at home with a friend or relative in case you lose your copy or need an emergency refill. Download this medication chart (PDF) to keep track of your medicines.
- Ask your health care professional for a note if you use controlled substances, or injectable medicines, such as EpiPens and insulin. Tell your health care professional about your travel. Let your cardiologist or internist know where you’ll be. Your health care professional might know medical professionals or reputable heart institutes in the area you’re visiting if help is needed.
- Comprehensive travel insurance usually includes medical evacuation travel insurance. Coverage varies by plan, destination and duration of trip, so shop around. But the average cost is about $200, which is a small investment if it can cover tens of thousands dollars of potential medical expenses.
- Some health care professionals recommend taking a copy of your pertinent medical records with you while traveling.
High altitudes, exotic spots
Oxygen availability declines at higher altitudes, which can place unique stressors on the cardiovascular system. As such, patients who are at risk of or who have established cardiovascular disease may be at an increased risk of adverse events when staying at mountainous locations. However, these risks may be minimized by appropriate pretravel assessments and planning through shared decision‐making between patients and their managing health care professionals.
Talk to your health care team before your trip to understand what you should do to prepare. You may wish to gradually move up the mountain and acclimate at lower elevations before moving to the higher altitudes. People with coronary artery disease and angina should anticipate that reduced oxygen levels may increase angina. Your heart has to work harder, especially if you already have blockage. Watch out for shortness of breath or other symptoms that could indicate you’re tipping from a stable to an unstable state.
Be mindful of your fluid consumption and sodium (salt) intake if you have cardiomyopathy or a history of heart failure . A balanced fluid intake is important in these conditions.
If you’re traveling to a country where certain vaccines are needed to guard against disease, it’s not likely the immunization will affect your heart. The bigger concern may be consistent access to quality medical care.
Consider selecting destinations in parts of the world that both interest you and have many options for health care you may need while you are visiting.
Long distance precautions
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person’s risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a large vein may also increase your risk of blood clots. Getting up and walking around when possible is recommended for long flights, just be sure the seatbelt light is not on when you do so. Stopping to take a quick break during long car rides may help as well.
Tell your health care professional about your travel plans to get the best advice on what precautions, if any, you may need to take. For example, some people might need compression stockings or additional oxygen. Others might need to watch fluids closely or avoid alcohol. And some may not be able to fly.
Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff .
Last Reviewed: Jan 16, 2024
- Patient Care & Health Information
- Diseases & Conditions
- What is a stroke? A Mayo Clinic expert explains
Learn more from neurologist Robert D. Brown, Jr. M.D., M.P.H.
I'm Dr. Robert Brown, neurologist at Mayo Clinic. In this video, we'll cover the basics of a stroke. What is it, who it happens to, the symptoms, diagnosis, and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available. You've likely heard the term stroke before. They affect about 800,000 people in the United States each year. Strokes happen in two ways. In the first, a blocked artery can cut off blood to an area of the brain. And this is known as an ischemic stroke. 85% of strokes are of this type. The second type of stroke happens when a blood vessel can leak or burst. So the blood spills into the brain tissue or surrounding the brain. And this is called a hemorrhagic stroke. Prompt treatment can reduce brain damage and the likelihood of death or disability. So if you or someone you know is experiencing a stroke, you should call 911 and seek emergency medical care right away.
Anyone can have a stroke, but some things put you at higher risk. And some things can lower your risk. If you're 55 and older, if you're African-American, if you're a man, or if you have a family history of strokes or heart attacks, your chances of having a stroke are higher. Being overweight, physically inactive, drinking alcohol heavily, recreational drug use. Those who smoke, have high blood pressure or high cholesterol, have poorly controlled diabetes, suffer from obstructive sleep apnea, or have certain forms of heart disease are at greater risk as well.
Look for these signs and symptoms if you think you or someone you know is having a stroke: Sudden trouble speaking and understanding what others are saying. Paralysis or numbness of the face, arm or leg on one side of the body. Problems seeing in one or both eyes, trouble walking, and a loss of balance. Now many strokes are not associated with headache, but a sudden and severe headache can sometimes occur with some types of stroke. If you notice any of these, even if they come and go or disappear completely, seek emergency medical attention or call 911. Don't wait to see if symptoms stop, for every minute counts.
Once you get to the hospital, your emergency team will review your symptoms and complete a physical exam. They will use several tests to help them figure out what type of stroke you're having and determine the best treatment for the stroke. This could include a CT scan or MRI scan, which are pictures of the brain and arteries, a carotid ultrasound, which is a soundwave test of the carotid arteries which provide blood flow to the front parts of the brain, and blood tests.
Once your doctors can determine if you're having an ischemic or hemorrhagic stroke, they'll be able to figure out the best treatment. If you're suffering an ischemic stroke, it's important to restore blood flow to your brain as quickly as possible, providing the oxygen and other nutrients your brain cells need to survive. To do this, doctors may use an intravenous clot buster medicine, dissolving the clot that is obstructing the blood flow or they may perform an emergency endovascular procedure. This involves advancing a tiny plastic tube called a catheter up into the brain arteries, allowing the blockage in the artery to be removed directly. Unlike ischemic strokes, the goal for treating a hemorrhagic stroke is to control the bleeding and reduce pressure in the brain. Doctors may use emergency medicines to lower the blood pressure, prevent blood vessel spasms, encourage clotting and prevent seizures. Or, if the bleeding is severe, surgery may be performed to remove the blood that is in the brain.
Every stroke is different, and so every person's road to recovery is different. Management of a stroke often involves a care team with several specialties. This may include a neurologist and a physical medicine and rehabilitation physician, among others. Now, in the end, our goal is to help you recover as much function as possible so that you can live independently. A stroke is a life-changing event that can affect you emotionally as much as it can physically. You may feel helpless, frustrated, or depressed. So look for help and support from friends and family. Accept that recovery will take hard work and most of all time. Strive for a new normal and remember to celebrate your progress. If you'd like to learn even more about strokes, watch our other related videos or visit mayoclinic.org. We wish you all the best.
An ischemic stroke occurs when the blood supply to part of the brain is blocked or reduced. This prevents brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes. Another type of stroke is a hemorrhagic stroke. It occurs when a blood vessel in the brain leaks or bursts and causes bleeding in the brain. The blood increases pressure on brain cells and damages them.
A stroke is a medical emergency. It's crucial to get medical treatment right away. Getting emergency medical help quickly can reduce brain damage and other stroke complications.
The good news is that fewer Americans die of stroke now than in the past. Effective treatments also can help prevent disability from stroke.
Products & Services
- A Book: Future Care
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Products for Independent Living from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
If you or someone you're with may be having a stroke, pay attention to the time the symptoms began. Some treatments are most effective when given soon after a stroke begins.
Symptoms of stroke include:
- Trouble speaking and understanding what others are saying. A person having a stroke may be confused, slur words or may not be able to understand speech.
- Numbness, weakness or paralysis in the face, arm or leg. This often affects just one side of the body. The person can try to raise both arms over the head. If one arm begins to fall, it may be a sign of a stroke. Also, one side of the mouth may droop when trying to smile.
- Problems seeing in one or both eyes. The person may suddenly have blurred or blackened vision in one or both eyes. Or the person may see double.
- Headache. A sudden, severe headache may be a symptom of a stroke. Vomiting, dizziness and a change in consciousness may occur with the headache.
- Trouble walking. Someone having a stroke may stumble or lose balance or coordination.
When to see a doctor
Seek immediate medical attention if you notice any symptoms of a stroke, even if they seem to come and go or they disappear completely. Think "FAST" and do the following:
- Face. Ask the person to smile. Does one side of the face droop?
- Arms. Ask the person to raise both arms. Does one arm drift downward? Or is one arm unable to rise?
- Speech. Ask the person to repeat a simple phrase. Is the person's speech slurred or different from usual?
- Time. If you see any of these signs, call 911 or emergency medical help right away.
Call 911 or your local emergency number immediately. Don't wait to see if symptoms stop. Every minute counts. The longer a stroke goes untreated, the greater the potential for brain damage and disability.
If you're with someone you suspect is having a stroke, watch the person carefully while waiting for emergency assistance.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
There are two main causes of stroke. An ischemic stroke is caused by a blocked artery in the brain. A hemorrhagic stroke is caused by leaking or bursting of a blood vessel in the brain. Some people may have only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA). A TIA doesn't cause lasting symptoms.
- Ischemic stroke
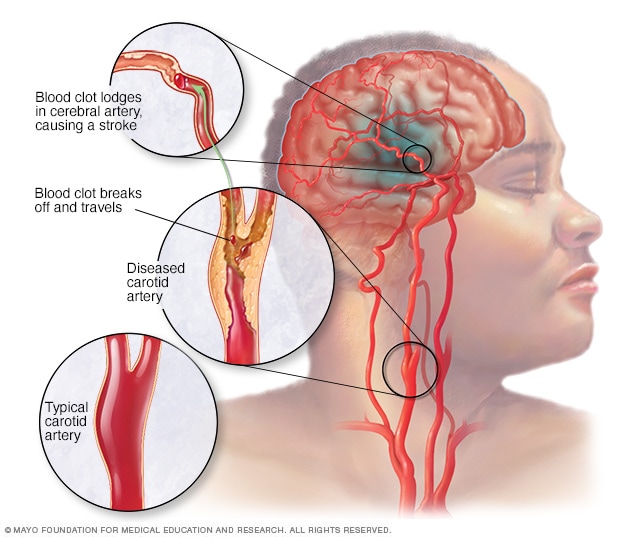
An ischemic stroke occurs when a blood clot, known as a thrombus, blocks or plugs an artery leading to the brain. A blood clot often forms in arteries damaged by a buildup of plaques, known as atherosclerosis. It can occur in the carotid artery of the neck as well as other arteries.
This is the most common type of stroke. It happens when the brain's blood vessels become narrowed or blocked. This causes reduced blood flow, known as ischemia. Blocked or narrowed blood vessels can be caused by fatty deposits that build up in blood vessels. Or they can be caused by blood clots or other debris that travel through the bloodstream, most often from the heart. An ischemic stroke occurs when fatty deposits, blood clots or other debris become lodged in the blood vessels in the brain.
Some early research shows that COVID-19 infection may increase the risk of ischemic stroke, but more study is needed.
Hemorrhagic stroke
Hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures. Bleeding inside the brain, known as a brain hemorrhage, can result from many conditions that affect the blood vessels. Factors related to hemorrhagic stroke include:
- High blood pressure that's not under control.
- Overtreatment with blood thinners, also known as anticoagulants.
- Bulges at weak spots in the blood vessel walls, known as aneurysms.
- Head trauma, such as from a car accident.
- Protein deposits in blood vessel walls that lead to weakness in the vessel wall. This is known as cerebral amyloid angiopathy.
- Ischemic stroke that leads to a brain hemorrhage.
A less common cause of bleeding in the brain is the rupture of an arteriovenous malformation (AVM). An AVM is an irregular tangle of thin-walled blood vessels.
Transient ischemic attack
A transient ischemic attack (TIA) is a temporary period of symptoms similar to those of a stroke. But a TIA doesn't cause permanent damage. A TIA is caused by a temporary decrease in blood supply to part of the brain. The decrease may last as little as five minutes. A transient ischemic attack is sometimes known as a ministroke.
A TIA occurs when a blood clot or fatty deposit reduces or blocks blood flow to part of the nervous system.
Seek emergency care even if you think you've had a TIA . It's not possible to tell if you're having a stroke or TIA based only on the symptoms. If you've had a TIA , it means you may have a partially blocked or narrowed artery leading to the brain. Having a TIA increases your risk of having a stroke later.
Risk factors
Many factors can increase the risk of stroke. Potentially treatable stroke risk factors include:
Lifestyle risk factors
- Being overweight or obese.
- Physical inactivity.
- Heavy or binge drinking.
- Use of illegal drugs such as cocaine and methamphetamine.
Medical risk factors
- High blood pressure.
- Cigarette smoking or secondhand smoke exposure.
- High cholesterol.
- Obstructive sleep apnea.
- Cardiovascular disease, including heart failure, heart defects, heart infection or irregular heart rhythm, such as atrial fibrillation.
- Personal or family history of stroke, heart attack or transient ischemic attack.
- COVID-19 infection.
Other factors associated with a higher risk of stroke include:
- Age — People age 55 or older have a higher risk of stroke than do younger people.
- Race or ethnicity — African American and Hispanic people have a higher risk of stroke than do people of other races or ethnicities.
- Sex — Men have a higher risk of stroke than do women. Women are usually older when they have strokes, and they're more likely to die of strokes than are men.
- Hormones — Taking birth control pills or hormone therapies that include estrogen can increase risk.
Complications
A stroke can sometimes cause temporary or permanent disabilities. Complications depend on how long the brain lacks blood flow and which part is affected. Complications may include:
- Loss of muscle movement, known as paralysis. You may become paralyzed on one side of the body. Or you may lose control of certain muscles, such as those on one side of the face or one arm.
- Trouble talking or swallowing. A stroke might affect the muscles in the mouth and throat. This can make it hard to talk clearly, swallow or eat. You also may have trouble with language, including speaking or understanding speech, reading or writing.
- Memory loss or trouble thinking. Many people who have had strokes experience some memory loss. Others may have trouble thinking, reasoning, making judgments and understanding concepts.
- Emotional symptoms. People who have had strokes may have more trouble controlling their emotions. Or they may develop depression.
- Pain. Pain, numbness or other feelings may occur in the parts of the body affected by stroke. If a stroke causes you to lose feeling in the left arm, you may develop a tingling sensation in that arm.
- Changes in behavior and self-care. People who have had strokes may become more withdrawn. They also may need help with grooming and daily chores.
You can take steps to prevent a stroke. It's important to know your stroke risk factors and follow the advice of your healthcare professional about healthy lifestyle strategies. If you've had a stroke, these measures might help prevent another stroke. If you have had a transient ischemic attack (TIA), these steps can help lower your risk of a stroke. The follow-up care you receive in the hospital and afterward also may play a role.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
- Control high blood pressure, known as hypertension. This is one of the most important things you can do to reduce your stroke risk. If you've had a stroke, lowering your blood pressure can help prevent a TIA or stroke in the future. Healthy lifestyle changes and medicines often are used to treat high blood pressure.
- Lower the amount of cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fats and trans fats, may reduce buildup in the arteries. If you can't control your cholesterol through dietary changes alone, you may need a cholesterol-lowering medicine.
- Quit tobacco use. Smoking raises the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting lowers your risk of stroke.
- Manage diabetes. Diet, exercise and losing weight can help you keep your blood sugar in a healthy range. If lifestyle factors aren't enough to control blood sugar, you may be prescribed diabetes medicine.
- Maintain a healthy weight. Being overweight contributes to other stroke risk factors, such as high blood pressure, cardiovascular disease and diabetes.
- Eat a diet rich in fruits and vegetables. Eating five or more servings of fruits or vegetables every day may reduce the risk of stroke. The Mediterranean diet, which emphasizes olive oil, fruit, nuts, vegetables and whole grains, may be helpful.
- Exercise regularly. Aerobic exercise reduces the risk of stroke in many ways. Exercise can lower blood pressure, increase the levels of good cholesterol, and improve the overall health of the blood vessels and heart. It also helps you lose weight, control diabetes and reduce stress. Gradually work up to at least 30 minutes of moderate physical activity on most or all days of the week. The American Heart association recommends getting 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous aerobic activity a week. Moderate intensity activities can include walking, jogging, swimming and bicycling.
- Drink alcohol in moderation, if at all. Drinking large amounts of alcohol increases the risk of high blood pressure, ischemic strokes and hemorrhagic strokes. Alcohol also may interact with other medicines you're taking. However, drinking small to moderate amounts of alcohol may help prevent ischemic stroke and decrease the blood's clotting tendency. A small to moderate amount is about one drink a day. Talk to your healthcare professional about what's appropriate for you.
- Treat obstructive sleep apnea (OSA). OSA is a sleep disorder that causes you to stop breathing for short periods several times during sleep. Your healthcare professional may recommend a sleep study if you have symptoms of OSA . Treatment includes a device that delivers positive airway pressure through a mask to keep the airway open while you sleep.
- Don't use illicit drugs. Certain illicit drugs such as cocaine and methamphetamine are established risk factors for a TIA or a stroke.
Preventive medicines
If you have had an ischemic stroke, you may need medicines to help lower your risk of having another stroke. If you have had a TIA , medicines can lower your risk of having a stroke in the future. These medicines may include:
Anti-platelet drugs. Platelets are cells in the blood that form clots. Anti-platelet medicines make these cells less sticky and less likely to clot. The most commonly used anti-platelet medicine is aspirin. Your healthcare professional can recommend the right dose of aspirin for you.
If you've had a TIA or minor stroke, you may take both an aspirin and an anti-platelet medicine such as clopidogrel (Plavix). These medicines may be prescribed for a period of time to reduce the risk of another stroke. If you can't take aspirin, you may be prescribed clopidogrel alone. Ticagrelor (Brilinta) is another anti-platelet medicine that can be used for stroke prevention.
Blooding-thinning medicines, known as anticoagulants. These medicines reduce blood clotting. Heparin is a fast-acting anticoagulant that may be used short-term in the hospital.
Slower acting warfarin (Jantoven) may be used over a longer term. Warfarin is a powerful blood-thinning medicine, so you need to take it exactly as directed and watch for side effects. You also need regular blood tests to monitor warfarin's effects.
Several newer blood-thinning medicines are available to prevent strokes in people who have a high risk. These medicines include dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and edoxaban (Savaysa). They work faster than warfarin and usually don't require regular blood tests or monitoring by your healthcare professional. These medicines also are associated with a lower risk of bleeding complications compared to warfarin.
Stroke care at Mayo Clinic
- Walls RM, et al., eds. Stroke. In: Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed Sept. 13, 2023.
- Ferri FF. Ferri's Clinical Advisor 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Sept. 13, 2023.
- Patients and caregivers. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/public-education/know-stroke/patients-and-caregivers#. Accessed Sept. 13, 2023.
- Stroke. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/stroke. Accessed Sept. 13, 2023.
- Oliveira-Filho J, et al. Initial assessment and management of acute stroke. https://www.uptodate.com/contents/search. Accessed Sept. 13, 2023.
- About stroke. Centers for Disease Control and Prevention. https://www.cdc.gov/stroke/healthy_living.htm. Accessed Sept. 13, 2023.
- Effects of stroke. American Stroke Association. https://www.stroke.org/en/about-stroke/effects-of-stroke. Accessed Sept. 13, 2023.
- Rehab therapy after a stroke. American Stroke Association. https://www.stroke.org/en/life-after-stroke/stroke-rehab/rehab-therapy-after-a-stroke. Accessed Sept. 13, 2023.
- Arteriovenous malformations (AVMs). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/arteriovenous-malformations-avms?search-term=arterial#. Accessed Oct. 2, 2023.
- Cerebral aneurysms. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/cerebral-aneurysms-fact-sheet. Accessed Sept. 13, 2023.
- Transient ischemic attack. Merck Manual Professional Version. https://www.merckmanuals.com/professional/neurologic-disorders/stroke/transient-ischemic-attack-tia?query=transient%20ischemic%20attack#. Accessed Sept. 13, 2023.
- Stroke. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Stroke-Rehabilitation-Fact-Sheet. Accessed Sept. 13, 2023.
- Rose NS, et al. Overview of secondary prevention of ischemic stroke. https://www.uptodate.com/contents/search. Accessed Sept. 13, 2023.
- Prevent stroke: What you can do. Centers for Disease Control and Prevention. https://www.cdc.gov/stroke/prevention.htm#print. Accessed Sept. 13, 2023.
- Know your risk for stroke. Centers for Disease Control and Prevention. https://www.cdc.gov/stroke/risk_factors.htm#. Accessed Oct. 2, 2023.
- Powers WJ, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke — A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; doi:10.1161/STR.0000000000000211.
- Papadakis MA, et al., eds. Quick Medical Diagnosis & Treatment 2023. McGraw Hill; 2023. https://accessmedicine.mhmedical.com. Accessed Sept. 13, 2023.
- Tsao CW, et al. Heart disease and stroke statistics — 2023 update: A report from the American Heart Association. Circulation. 2023; doi:10.1161/CIR.0000000000001123.
- Grotta JC, et al., eds. Stroke: Pathophysiology, Diagnosis, and Management. 7th ed. Elsevier, 2022. https://www.clinicalkey.com. Accessed Sept. 15, 2023.
- Suppah M, et al. An evidence-based approach to anticoagulation therapy comparing direct oral anticoagulants and vitamin K antagonists in patients with atrial fibrillation and bioprosthetic valves: A systematic review, meta-analysis and network meta-analysis. American Journal of Cardiology. 2023; doi:10.1016/j.amjcard.2023.07.141.
- Tyagi K, et al. Neurological manifestations of SARS-CoV-2: Complexity, mechanism and associated disorders. European Journal of Medical Research. 2023; doi:10.1186/s40001-023-01293-2.
- Siegler JE, et al. Cerebrovascular disease in COVID-19. Viruses. 2023; doi:10.3390/v15071598.
- Lombardo M, et al. Health effects of red wine consumption: A narrative review of an issue that still deserves debate. Nutrients. 2023; doi:10.3390/nu15081921.
- Jim J. Complications of carotid endarterectomy. https://www.uptodate.com/contents/search. Accessed Oct. 2, 2023.
- Van Nimwegan D, et al. Interventions for improving psychosocial well-being after stroke: A systematic review. International Journal of Nursing Studies. 2023; doi:10.1016/j.ijnurstu. 2023.104492 .
- Hasan TF, et al. Diagnosis and management of acute ischemic stroke. Mayo Clinic Proceedings. 2018; doi:10.1016/j.mayocp.2018.02.013.
- Ami TR. Allscripts EPSi. Mayo Clinic. Sept. 4, 2023.
- Barrett KM, et al. Ambulance-based assessment of NIH stroke scale with telemedicine: A feasibility pilot study. Journal of Telemedicine and Telecare. 2017; doi:10.1177/1357633X16648490.
- Sener U, et al. Ischemic stroke in patients with malignancy. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2022.09.003.
- Quality check. The Joint Commission. https://www.qualitycheck.org/search/?keyword=mayo%20clinic. Accessed Oct. 4, 2023.
- Quality care you can trust. American Heart Association. https://www.heart.org/en/professional/quality-improvement/hospital-maps. Accessed Oct. 4, 2023.
- Attig JM. Allscripts EPSi. Mayo Clinic. Oct. 9, 2023.
- How much physical activity do you need? American Heart Association. https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-infographic. Accessed Oct. 12, 2023.
- Graff-Radford J (expert opinion). Mayo Clinic. Oct. 11, 2023.
- Healthcare. DNV Healthcare USA, Inc. https://www.dnvhealthcareportal.com/hospitals?search_type=and&q=mayo+clinic&c=&c=20806&c=&c=&prSubmit=Search. Accessed Nov. 1, 2023.
- Brain hemisphere connections
- Cerebral angiogram
- CT scan of brain tissue damaged by stroke
- Stroke rehabilitation
- Strokes FAQ Neurologist Robert D. Brown, Jr. M.D., M.P.H., answers the most frequently asked questions about strokes.
- Typing with Brain Waves
Associated Procedures
- Carotid angioplasty and stenting
- Carotid endarterectomy
- Carotid ultrasound
- Coronary angioplasty and stents
- Echocardiogram
- Home enteral nutrition
News from Mayo Clinic
- Mayo Clinic Minute: How extreme temperatures can increase stroke risk July 20, 2023, 04:30 p.m. CDT
- Mayo Clinic Minute: What women need to know about stroke May 30, 2023, 04:15 p.m. CDT
- From lift off to splash down: An update on Mayo Clinic stem cells in space May 26, 2023, 04:39 p.m. CDT
- Mayo Clinic Minute: How to reduce your stroke risk May 10, 2023, 01:30 p.m. CDT
- A cheeseburger's role in one man's stroke recovery Nov. 11, 2022, 05:30 p.m. CDT
- Florida mom reunites with ICU team after stroke Oct. 28, 2022, 04:30 p.m. CDT
- Mayo Clinic Q&A podcast: World Stroke Day -- know the warning signs, take action Oct. 28, 2022, 12:30 p.m. CDT
- Mayo Clinic Minute: Flu vaccine may reduce risk of stroke Oct. 24, 2022, 04:00 p.m. CDT
- Mayo Clinic experts say time is most critical factor for better stroke outcomes Oct. 20, 2022, 05:58 p.m. CDT
- Sean Bretz reflects on overcoming stroke, becoming a dad Sept. 19, 2022, 04:30 p.m. CDT
- Mayo Clinic in Arizona receives comprehensive stroke center certification May 24, 2022, 04:00 p.m. CDT
- Mayo Clinic Q&A podcast: Don't ignore the warning signs of stroke May 24, 2022, 01:30 p.m. CDT
- Tips to reduce stroke in the diverse communities May 10, 2022, 03:00 p.m. CDT
- Mayo Clinic Minute: African Americans at higher risk of stroke May 06, 2022, 04:30 p.m. CDT
- Heart procedure to reduce stroke risk should manage small leaks April 04, 2022, 03:00 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.

Life After Stroke: 10 Tips to Help You With Holiday Travel
These post-stroke tips can help take the hassle out of flights and car rides.
Crowds, traffic, and the potential for bad weather can make holiday travel daunting for anyone. But if you’ve recently had a stroke, it can be especially challenging. Depending on your level of disability — if any — travel skills you may have once taken for granted, such as sprinting through the airport or carrying your own luggage, may seem impossible.
Still, you don’t have to let a prior stroke stop you. The trick is to be prepared so you can enjoy the journey. These tips will help you get to your destination on time so you can celebrate the holidays with peace of mind.
1. Get Cleared by a Doctor for Travel
Before traveling by plane or car, get your doctor’s okay. Flying at 30,000 feet or driving won’t cause another stroke, but timing matters. If you’ve had a stroke, including a ministroke or a transient ischemic attack (TIA) , within the last 30 days, you’re at slightly increased risk for having another one, says Thomas Maldonado, MD , professor of surgery at NYU Langone Health in New York City.
As the saying goes, “time is brain” when it comes to stroke treatment . Getting to a stroke center quickly for treatment can mean the difference between making a full recovery or not. Before putting yourself in a situation in which you can’t get treatment fast, such as when you’re in flight, make sure you’ve had all necessary tests to determine the cause of the stroke and a solid treatment plan .
Overall, there are no one-size-fits-all guidelines for traveling after a stroke. It can depend on where the stroke occurred in your brain, the resulting disabilities or symptoms, the cause, and its severity. “But if you don’t have definitive treatment for the cause of the stroke, you should not travel,” Dr. Maldonado says.
Also, don’t do the driving until you’ve received clearance from your doctor as well.
2. Request a Wheelchair if Walking Is Difficult
If a stroke has slowed your walking pace or walking is difficult, request a wheelchair at the airport. “It’s the fastest way to get to the gate,” says Stephanie Mensh, whose husband, Paul Berger, had a stroke more than 30 years ago . The couple runs Stroke Survivor, a site that offers post-stroke life-management guidelines in a quarterly newsletter.
Although Berger experienced paralysis on the right side of his body, he can walk slowly now, with the help of a foot brace. But wheelchair assistance helps Berger speed through airport security and beyond quickly. “Over the holidays, there will be lots of people waiting for wheelchair assistance. You may have to wait for a porter,” Mensh says.
Be sure to get to the airport plenty early — at least three hours ahead of time. Contact your airline ahead of time to request wheelchair assistance at arrival.
3. Apply for TSA Precheck
If you wear a foot brace like Berger does, walking in stocking feet isn’t safe. TSA Precheck allows you to avoid having to take your shoes off when going through airport security, which can be a lifesaver if wheelchair assistance isn’t available.
4. Bring a Ziplock Bag to Retrieve Pocket Belongings More Easily
If you have limited manual dexterity, a ziplock bag can come in handy. When going through airport security, put your wallet and the contents of your pockets into the ziplock bag, then put the bag on the security belt. It helps you avoid having to retrieve individual items from the bin, which can take extra time.
5. Make Frequent Pit Stops
When traveling by car during high traffic times, such as Thanksgiving or Christmas week, take a route with rest stops, such as a major highway, and plan for breaks at least every two hours. “After a stroke, it can be hard to sit for long periods without using the bathroom,” Mensh says. Build rest stop time into your itinerary.
6. Come Equipped With Mobility Aids
If you require a foot brace or other mobility aids, such as a tub seat for the shower, pack an extra one in case it gets lost or damaged.
7. Stay at a Hotel With Accessible Rooms
“A hotel is easier than staying at someone’s home,” Mensh says. Even if you don’t require a wheelchair, hotels have accessible bathrooms, with grab bars and a shower seat. If there’s no elevator, ask for a room on the ground floor. Hotel architecture can vary widely. Checking out the hotel online before booking can help you decide if the place is right for you.
8. Use a Cane to Help With Walking on Uneven Pavement
Even if you don’t need a cane to get around, consider using one when you’re traveling, especially if a stroke has affected your walking. “A cane helps with balance on uneven pavement. It also gives other people notice, alerting them, for example, that you won’t be able to run when you’re in the crosswalk to get out of the way of an oncoming car,” Mensh says.
9. Don’t Forget Your Medication
Pharmacies can close on major holidays, so make sure you have all of the medication you will need while traveling, plus some extra in case you get delayed or snowed in.
10. Bring a Written Itinerary and Make Copies for Your Travel Party
A stroke can affect memory and processing abilities. But bringing a detailed schedule can make it easier to stay on track. “We type up a travel itinerary by date and time, including all the information about the flights, hotel address and phone, car rental information, confirmation numbers, and anything else important,” Berger says. “We give copies to our families and pet sitter, pack a copy, and each have one in our pockets. I refer to it constantly.”
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

A newer edition of this book is available.
- < Previous chapter
- Next chapter >

4 History-taking in the stroke patient
- Published: January 2010
- Cite Icon Cite
- Permissions Icon Permissions
General principles of history-taking in the stroke patient
Stroke is defined as a sudden-onset focal neurological deficit lasting for 24 hours or more, or leading to earlier death attributed to a vascular cause.
General points about history-taking
Make the patient central.
Stroke affects a wide variety of patients but particularly older people. It can be very challenging to get a coherent history. By definition stroke is sudden onset—one moment a person is well and the next they are not, and so acute stroke patients are often frightened. Patients may be drowsy, disorientated, frightened, dysphasic or even demented as a result of the stroke or other comorbidity. Therefore, the history, the most vital part of clinical evaluation, may be very difficult.
Always start by allowing the patient to give their version of events. If allowed to speak, most patients will not talk for more than a couple of minutes and often that amount of time will provide all the information you need to make a diagnosis.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.

Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Skip to main content
- Keyboard shortcuts for audio player
The Francis Scott Key bridge in Baltimore collapses, 6 feared dead

Jonathan Franklin
Jason Breslow
Rachel Treisman
Ayana Archie

In an aerial view, the cargo ship Dali sits in the water after running into and collapsing the Francis Scott Key Bridge in Baltimore on Tuesday. Tasos Katopodis/Getty Images hide caption
In an aerial view, the cargo ship Dali sits in the water after running into and collapsing the Francis Scott Key Bridge in Baltimore on Tuesday.
At least six people are presumed dead following the collapse of the Francis Scott Key Bridge in Baltimore early Tuesday morning, officials said.
The bridge fell into the Patapsco River after it was struck by a nearly 1,000-foot-long container ship, sending several people plunging into the frigid waters below.
During a news update Tuesday evening, the U.S. Coast Guard told reporters they are ending an active search and rescue operation for the six people left unaccounted for at 7:30 p.m. local time.
More from WYPR in Baltimore:
- Construction worker says friends, colleagues missing in bridge collapse
- Federal government pledges full support to rebuild FSK bridge, reopen port
For the latest from member station WYPR in Baltimore head to wypr.org
Rear Adm. Shannon Gilreath said that based on the length of time since the bridge collapsed and the water temperatures, they don't believe that search teams are going to find any of these individuals still alive.
Gilreath told reporters that the Coast Guard is not leaving, but is going to "transition to a different phase."
The recovery phase will begin at 6 a.m. local time Wednesday when divers will begin searching for remains of all missing victims , Gilreath said.
Col. Roland L. Butler, Jr., Secretary of Maryland State Police, told reporters the conditions have changed and made it dangerous for first responders and divers to be in the water.
He emphasized that police will still have surface ships out in the water overnight.
"We're hoping to put those divers in the water and begin a more detailed search to do our very best to recover those six missing people," Butler said.
The collision set off a rapid search-and-rescue operation. Eight people from a construction crew that was working to repair potholes on the bridge are thought to have fallen into the water, Maryland Transportation Secretary Paul Wiedefeld told reporters.
Authorities did not believe any drivers were submerged in their cars, Wiedefeld said.
The bridge collapsed instantly
Eyepress/Reuters
The bridge, which is part of Interstate 695, collapsed around 1:30 a.m. when it was struck by a massive cargo vessel named the Dali. Dramatic video of the collision shows the hulking ship–the length of more than three football fields– slamming into one of the bridge's pillars, and then an expanse of the bridge falling into the water instantly.
The Dali, a Singapore-flagged ship, had left Baltimore at 1 a.m. and was bound for Colombo, Sri Lanka, according to Marine Traffic , a maritime data site.

The Picture Show
Photos: baltimore's key bridge collapses; search and rescue efforts continue.
Synergy Marine Group, the company that manages the ship, said in a statement that all 22 crew members are accounted for and that there were no injuries resulting from the crash. The company also said there was no pollution to the water.
In a briefing for the media, Moore said the crew of the container ship had notified authorities about a power outage onboard shortly before the collision. The crew notified authorities of "a power issue," Moore said, confirming earlier reports that they had lost power on the ship.
The ship was traveling at approximately 8 knots when it hit the bridge, Moore said. In the immediate aftermath of the collision, officials feared motorists might be submerged in the river, but Moore said that a mayday signal was issued with enough time for authorities to stop the flow of traffic coming over the bridge.

A collapsed section of the Francis Scott Key Bridge in Baltimore is seen in the waters of the Patapsco River. The bridge collapsed early Tuesday after it was struck by a 984-foot-long cargo ship. Win McNamee/Getty Images hide caption
A collapsed section of the Francis Scott Key Bridge in Baltimore is seen in the waters of the Patapsco River. The bridge collapsed early Tuesday after it was struck by a 984-foot-long cargo ship.
"I have to say I'm thankful for the folks who once the warning came up, and once notification came up that there was a mayday, who literally by being able to stop cars from coming over the bridge, these people are heroes. They saved lives," Moore said.
FBI and state officials said the preliminary investigation points to an accident and that there was no credible evidence of any terrorist attack. Moore said the Francis Scott Key Bridge was fully up to code and there was no structural issue with the bridge.
"In fact, the bridge was actually fully up to code," Moore said.
The ship has had at least one previous accident
Vessel traffic in and out of the Port of Baltimore, one of the busiest on the East Coast, was suspended "until further notice," port officials announced, as search-and-rescue operations continued and the preliminary investigation into the crash was getting underway.
"This does not mean the Port of Baltimore is closed," port officials said in a statement. "Trucks are being processed within our marine terminals."
Gov. Moore declared a state of emergency and said his office was in close communication with Secretary of Transportation Pete Buttigieg. The secretary was due to arrive in Baltimore to visit the crash site and receive updates on the investigation.

Maryland Gov. Wes Moore, left, speaks during a news conference as Sen. Chris Van Hollen (D-Md.) looks on near the scene where a container ship collided with a support on the Francis Scott Key Bridge. Steve Ruark/AP hide caption
Maryland Gov. Wes Moore, left, speaks during a news conference as Sen. Chris Van Hollen (D-Md.) looks on near the scene where a container ship collided with a support on the Francis Scott Key Bridge.
The National Transportation Safety Board said it will investigate what happened, announcing on X (formerly Twitter) that it was launching a "go team" to Baltimore.
Prior to the crash, the ship had completed 27 inspections, according to a database by the maritime safety site Equasis. In one inspection at a port in Chile last year, the ship was determined to have a deficiency related to "propulsion and auxiliary machinery," according to Equasis.
In 2016, an inspection found "hull damage impairing sea worthiness" after the ship hit a dock on its way out of the port of Antwerp. Video of the incident shows the stern of the ship scraping against the quay as it attempted to exit the North Sea container terminal.
The bridge is an important travel route with a deep history

Members of the National Transportation Safety Board listen to NTSB Chair Jennifer Homendy speak during a news conference near the scene where a container ship collided with a support on the Francis Scott Key Bridge, in Dundalk, Md., Tuesday, March 26, 2024. Matt Rourke/AP hide caption
Members of the National Transportation Safety Board listen to NTSB Chair Jennifer Homendy speak during a news conference near the scene where a container ship collided with a support on the Francis Scott Key Bridge, in Dundalk, Md., Tuesday, March 26, 2024.
The bridge's collapse leaves Baltimore and travelers along the East Coast without a vital transit corridor for the foreseeable future. The four-lane, 1.6-mile-long bridge carries some 11.3 million vehicles each year, according to state data, and is one of three ways to get through Baltimore on the interstate.
Reconstructing the bridge will be a "long-term build," Moore told reporters.
Speaking from the White House, President Biden said he intends for the federal government to "pay for the entire cost of reconstructing that bridge."
"We're gonna get it up and running again as soon as possible," Biden said. "Fifteen thousand jobs depend on that port, and we're gonna do everything we can to protect those jobs and help those workers."
The bridge isn't just a vital transportation route. It also has a special historical significance.
It opened to the public in March 1977, but its history goes much deeper than that. Scholars believe it stood within 100 yards of the site where its namesake, Francis Scott Key, witnessed the failed British bombardment of Fort McHenry in September 1814.
Key, an American lawyer, watched the battle from the British warship he had boarded to negotiate the release of a detained American civilian. The awe he felt at seeing the flag rise the next morning inspired him to write "Defense of Fort McHenry," which was later renamed "The Star-Spangled Banner" and became the U.S. national anthem in 1931.
Shippers are scrambling to re-route their cargo
Roughly $80 billion worth of cargo passes through the Port of Baltimore each year. But with the port's shipping channels now closed indefinitely due to the accident, shippers have been left scrambling to find alternate routes to transport their goods to and from the East Coast.
Some vessels have already been diverted to Norfolk, Va., Margie Shapiro, who runs a freight handling business in Baltimore, told NPR . Other traffic could be re-routed through New York or Philadelphia.
The Dali was being chartered by Maersk and carrying cargo for Maersk customers, the shipping giant said in a statement . The company said it would be omitting Baltimore from its services "until it is deemed safe for passage through this area."
Cargo already at the Port of Baltimore will have to travel overland, but truck traffic will also be snarled by the loss of the bridge.
"The whole ecosystem is going to be a little bit off," Shapiro said. "When the ecosystem gets messy, things get messy. Freight rates go up. The world gets a little bit chaotic."
NPR's Dave Mistich and Scott Horsley contributed to this report.
- francis scott key bridge
- Francis Scott Key Bridge
- Baltimore bridge collapse
- francis scott key
- International edition
- Australia edition
- Europe edition

Travel agent won’t cancel my sick mother’s holiday
She suffered a stroke just three weeks before the cruise and can’t speak
Ten months ago, my parents paid £4,000 for a holiday with Princess Cruises through the travel agent cruise118.com. Last month, three weeks before departure, my mum suffered a stroke. She’s now in intensive care, unable to speak and or move. I tried to cancel the holiday and claim the 25% refund due under the booking terms and conditions. BA immediately agreed to refund the flights, but cruise118.com informed me that, due to data protection rules (GDPR), only my mother, as the lead passenger, could cancel. My parents had annual travel insurance but it did not cover the region they were going to. My mother applied to upgrade it the day before her stroke, but by the time the quote arrived it was too late. LHV, York
This is terribly sad. Your mother is only in her 60s and was active and healthy. Cruise118.com’s stance strikes me as utterly unreasonable. You had sent a letter from the hospital confirming her condition and offered to put your father, as a named passenger, on the phone.
I asked it how its interpretation of GDPR worked if a customer could not speak for themselves. Whereupon it acknowledged a “misunderstanding”. “We have an established process that allows cancellation to be processed on a lead passenger’s behalf, by providing appropriate medical documentation,” it said.
Because the window for the 25% refund had closed, it agreed to refund you and Princess Cruises, on discovering the circumstances, magnanimously returned the rest of the holiday cost as a goodwill gesture. My advice to travellers is take out travel insurance as soon as you book so you are covered from the outset. Email [email protected] . Include an address and phone number. Submission and publication are subject to our terms and conditions
- Consumer affairs
- Your problems, with Anna Tims
- Consumer rights
Comments (…)
Most viewed.
Southwest’s first red-eye flights are coming. Here’s where and when.
The airline expects to launch overnight flights from las vegas and hawaii.
Southwest Airlines is preparing to launch overnight flights for the first time in its history.
After hinting at the change last year , the Dallas-based carrier plans to add overnight flights from Las Vegas and Hawaii, Chief Commercial Officer Ryan Green said at an air travel conference Wednesday. The airline still has a few technical and labor details to work out before the flights can begin, but it hopes to get them in the air in about two years, Green said.
Green added that he sees an opportunity for about 50 red-eye flights a day at Southwest.
Red eyes, so called for the appearance of travelers’ eyes after missing a night of sleep, are ubiquitous at most major airlines. Travelers book them for what are often cheaper fares than daytime flights. For travelers from the West Coast, they also offer the advantage of leaving after work and arriving on the East Coast the next day in time for a breakfast meeting.
And airlines like overnight flights because they can generate more revenue from an airplane that would otherwise sit idle at an airport until the next morning.
Las Vegas’s Harry Reid International Airport boasted no fewer than 26 overnight flights departing after 9 p.m. on almost every U.S. airline on a random Thursday in March, data from aviation analytics firm Cirium Diio shows. These flights, which are typically over four hours, connect Sin City to cities such as Atlanta, Boston, New York and D.C.
Southwest plays catch up on red eyes
Southwest is beloved by travelers for its quirkiness, all-economy seating with no seat assignments and free checked bags. What it is not known for is being on the forefront of travel technology. Remember the plastic boarding cards you picked up at the gate well into the 2000s ? Or the Great Meltdown of 2022 ?
For most of its 50-plus years flying, Southwest could not offer anything more than daytime flights in the U.S. due to limits with its reservations system. That changed in 2014 when it began implementing a new, modern booking system from airline IT provider Amadeus to launch international flights. Overnight flights became possible in 2017 when the platform was fully adopted.
It took another six years before Southwest began selling tickets with overnight connections last July.
Southwest CEO Robert Jordan in November described the possibility of overnight flights at the airline as the latest “ evolution ” of its business model.
Cheap, easy growth
Southwest, like most airlines, is in a bind. Aviation supply chain issues mean many of the new planes it has ordered from Boeing are years behind schedule. Costs are also up thanks to inflation and new post-pandemic labor agreements.
Boeing’s issues have forced Southwest to cut its growth plans this year. Instead of 79 new 737 Max planes, it will only take around 46.
“We have to be maniacally focused on being efficient,” Green said, adding that the airline wants to grow but without “adding to the cost structure.”
Enter overnight flights.
Savanthi Syth, an airline analyst at investment bank Raymond James, said in an email that adding red-eye flights would allow Southwest to grow at less cost than buying new planes.
“In the Hawaii-mainland U.S. market, red-eye flight capabilities should enable more connections or just a better schedule than Southwest can offer today,” she added.
That’s good news for the many loyal Southwest fliers in, say, Dallas or Kansas City, Mo., whose only flight option home from Hawaii is to lose an entire day to travel.
Similarly, more flights from Las Vegas could help slow fare increases. The average U.S. domestic airfare from the city, not including added fees such as checked bags or seat assignments, was up 12 percent to $264.38 in the third quarter of last year compared with 2019, according to Bureau of Transportation Statistics data . Airfares were down 6 percent when adjusted for inflation.
“Southwest’s significant volume of red-eye flights will bring additional capacity to an already crowded Las Vegas market,” said Seth Miller, an airline analyst and editor of the PaxEx.Aero website. “Passengers should benefit as destination options expand and fares remain competitive.”
More on air travel
Leave flying to the pros: Think you could land a plane in an emergency? Experts say you’re wrong . Here’s what you should actually do if something goes awry during a flight .
Pet peeves: Why do “gate lice” line up early for a flight ? Psychologists explained for us. Another move that annoys airline workers: abusing the flight attendant call button . For more on how to behave on a flight, check out our 52 definitive rules of flying .
Plane mess: Stories about extremely disgusting airplanes have been grossing out travelers. The question of plane cleanups became the subject of a recent debate after a flight attendant allegedly told a pregnant passenger to pick up the popcorn spilled by her toddler.
Frequent flying: Airline status isn’t what it used to be, but at least there are some good movies and TV shows to watch in the air. And somewhere out there, experts are trying to make airline food taste good.

Help | Advanced Search
Quantitative Biology > Cell Behavior
Title: a data-informed mathematical model of microglial cell dynamics during ischemic stroke in the middle cerebral artery.
Abstract: Neuroinflammation immediately follows the onset of ischemic stroke in the middle cerebral artery. During this process, microglial cells are activated in and recruited to the penumbra. Microglial cells can be activated into two different phenotypes: M1, which can worsen brain injury; or M2, which can aid in long-term recovery. In this study, we contribute a summary of experimental data on microglial cell counts in the penumbra following ischemic stroke induced by middle cerebral artery occlusion (MCAO) in mice and compile available data sets into a single set suitable for time series analysis. Further, we formulate a mathematical model of microglial cells in the penumbra during ischemic stroke due to MCAO. Through use of global sensitivity analysis and Markov Chain Monte Carlo (MCMC)-based parameter estimation, we analyze the effects of the model parameters on the number of M1 and M2 cells in the penumbra and fit identifiable parameters to the compiled experimental data set. We utilize results from MCMC parameter estimation to ascertain uncertainty bounds and forward predictions for the number of M1 and M2 microglial cells over time. Results demonstrate the significance of parameters related to M1 and M2 activation on the number of M1 and M2 microglial cells. Simulations further suggest that potential outliers in the observed data may be omitted and forecast predictions suggest a lingering inflammatory response.
Submission history
Access paper:.
- HTML (experimental)
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .
Where is the Francis Scott Key Bridge? What to know about collapsed Baltimore bridge
The collapse of the Francis Scott Key Bridge , a major transportation link in the Baltimore area, sparked a massive search and rescue effort early Tuesday morning.
The bridge has been a critical transportation passageway along the East Coast for decades. Video captured the collapse , after Singapore-flagged container ship, the Dali, collided with one of the bridge's pillars.
The ship had caught fire, and several vehicles fell into the river below.
Here's what to know about the Francis Scott Key Bridge.
Follow here for live updates → Baltimore's Key Bridge collapses after ship collision; rescue effort underway
Where is the Francis Scott Key Bridge located?
The bridge crosses over the Patapsco River on I-695 and is the final link on the Baltimore Beltway, according to the Maryland Transportation Authority .
It is the outermost of the three tollways that cross Baltimore's Harbor.
How long is the Francis Scott Key Bridge?
The 4-lane bridge structure alone is 1.6 miles long. The facility also includes the Curtis Creek Drawbridge. Including approach roadways, the entire stretch is around 10.9 miles long, MDTA said.
Why did a ship hit the Francis Scott Key Bridge?
The ship, a container vessel chartered by Maersk, apparently lost power a few minutes before striking the bridge, a senior U.S. official told USA TODAY .
No Maersk crew or personnel were onboard the vessel when it struck the bridge, according to a statement from the company. It was operated by a charter company, Synergy Group, and owned by Grace Ocean Pte., based in Singapore, and ultimately bound for Sri Lanka.
Accidents like this, called Marine casualties, are not uncommon, the official told USA TODAY, with an allision (an immobile object being struck by a ship) occurring about every 10 years or so. Investigators will likely look into the cause of the power outage and whether there was a mechanical failure on the ship.
How old is the Key Bridge in Baltimore?
The Francis Scott Key Bridge opened in March 1977, according to the Maryland Transportation Authority .
What type of bridge is the Francis Scott Key?
The steel-arched bridge was the second-longest continuous-truss bridge span in the world when it was built and remains the second longest in the United States and third in the world, according to the American Civil Engineering Society .
When was the Francis Scott Key Bridge built?
Construction of the Francis Scott Key Bridge began in 1972.
Francis Scott Key Bridge has a deep history
According to the MDTA, the bridge crosses over the Patapsco River, near where Francis Scott Key, the bridge's namesake, was inspired to write the lyrics of the Star Spangled Banner.
Key is believed to have witnessed the bombardment of Fort McHenry on the night of Sept. 12, 1814, within 100 yards of the modern-day bridge. That battle is what inspired him to the national anthem.
How vital is the Francis Scott Key Bridge?
The bridge is critical to East Coast shipping. The port’s private and public terminals handled 847,158 autos and light trucks in 2023, the most of any U.S. port. The port also handles farm and construction machinery, sugar, gypsum and coal, according to a Maryland government website.
National Geographic content straight to your inbox—sign up for our popular newsletters here

The story behind Chicago deep dish pizza
This thick, cheese-laden take on the Italian original has become a culinary icon — but who exactly invented it?
Deep dish pizza is synonymous with Chicago. A thick, bread-like base topped with layers of mozzarella and chunky tomato sauce is the perfect fortification, some might argue, against the notoriously long and cold Chicago winters.
Not everyone appreciates it, however. “Chicago pizza is not only not better than New York pizza, it’s not pizza. It’s a fucking casserole ,” comedian (and New Yorker) Jon Stewart once ranted on his TV programme, The Daily Show . And it’s true that for those used to a thin New York-style slice, or even more delicate Neapolitan pizzas, deep dish can seem a little… excessive. But who can resist the lure of so much melted cheese? Even Stewart saw the error of his ways and publicly repented.
According to the legend perpetuated by Pizzeria Uno , Ike Sewell, the original owner of Uno, invented deep dish pizza back in 1943. But this isn’t quite true, argues pizza historian Peter Regas , who’s been investigating the roots of deep dish for more than a decade. True deep dish was indeed invented at 29 East Ohio Street (the address of Pizzeria Uno’s first restaurant) in the autumn of 1943, says Regas — but not by Sewell. The actual mastermind was apparently Ric Riccardo, who discovered a pizza oven and round cast iron pans in the kitchen when he took over the place.

Riccardo named his restaurant Pizzeria Riccardo — but did he actually make the pizza? Possibly, but he was a businessman and an artist, not a cook. He’d also grown up in northern Italy, and pizza — at that time still a rarity in Chicago — was a southern Italian dish, the thin crust version originating in Naples and rustico, a hand pie stuffed with fillings including mozzarella and tomato, being a popular street food in Salento. Some sources credit Pizzeria Uno’s manager, Rudy Malnati Sr, or his son Lou, a bartender, with the deep dish’s invention, but Regas has found evidence that Malnati didn’t join the restaurant until a few years later. Meanwhile, Sewell, a Texan and a liquor distributor by trade, didn’t partner with Riccardo until early 1944, and his main contribution to the operation was money.
The first deep dish pizza, according to Regas, was about an inch tall — half the height of the modern product — and whoever was in Riccardo’s kitchen used standard pizza dough, made with flour, yeast, salt and water. The current fortified dough appeared in the 1950s courtesy of Alice Mae Redmond, a cook from Mississippi who thought the original wasn’t stretchy enough and incorporated elements from her recipe for Southern-style biscuits — namely oil.
Riccardo died in 1954 and Redmond and the Malnatis moved on to rival pizzerias, Gino’s East and Lou Malnati’s. Sewell, by this point the sole owner, changed the name to Pizzeria Uno. In 1977, he sold up to a Boston conglomerate, which simplified the origin story to give him all the credit. “[The CEO] told me, ‘Ike Sewell is our Colonel Sanders’,” Regas says, referring to the KFC figurehead. “The idea that they are the original is the most important thing.”
How it’s made
Crust recipes, topping selections and sauce seasonings vary from pizzeria to pizzeria, but all deep dish pizzas begin with a cast iron pan lined with a yeasty dough fortified with either olive oil or butter. It’s then filled with heaps of mozzarella cheese, covered with toppings and finished off with a layer of tomato sauce. Although the original Uno’s pizza was just cheese and tomato, one of the most dominant toppings in Chicago today is sausage.
Several variations have appeared over the years. Stuffed pizza, served at Nancy’s and Giordano’s, has a second layer of crust above the cheese. A variant known as pan pizza, invented at Pequod’s, has an extra sprinkling of cheese between the crust and the side of the pan, which caramelises during baking.
Several chains, including Uno’s and Lou Malnati’s, sell frozen pizzas in grocery stores and by mail order. The first recipe for home cooks appeared as early as 1945, according to Chicago Tribune archives, but most Chicagoans still prefer to get theirs from a pizzeria.

Where to try it
1. lou malnati’s.
Founded in 1971, Lou Malnati’s is the largest of the deep dish chains, with around 80 locations across the city, Illinois, Wisconsin, Indiana and Arizona, home to many expat Chicagoans. It’s famous for its flaky, buttery crust and enormous sausage patty topping; gluten-free offerings include a crustless pizza held together with yet more sausage.
2. Pequod’s
Pequod’s caramelised cheese crust, invented by its founder, Burt Katz, has a cult following among Chicago pizza connoisseurs. If you go at the weekend, be prepared to wait for a table, but very few visitors would argue it’s not worth it. The $7.95 (£6) individual pizza lunch special is one of the best deals in town.
3. Milly’s Pizza in the Pan
Newcomer Milly’s began as founder Robert Maleski’s pandemic project. He made just 20 pizzas a night and always sold out: Chicagoans loved his caramelised cheese crust and surprising topping combinations such as cherry tomatoes, jalapeños, bacon and pineapple. In 2021, he moved into a permanent space in the Uptown neighborhood, where his pizzas remain a hot item; it’s best to order in advance. A second location is scheduled to open this year.
( Liked ‘The Bear’? Eat your way around Chicago with these iconic dishes. )
Related Topics
- FOOD TOURISM
- STREET FOODS
- FOOD AND THE ENVIRONMENT
- FOOD CULTURE
- FOOD HISTORY
You May Also Like

How to plan a springtime food weekend in the Cotswolds, UK

Where to eat in Bogotá, the Colombian capital taking on Lima's food crown
Limited time offer.
Get a FREE tote featuring 1 of 7 ICONIC PLACES OF THE WORLD

Why mole is Oaxaca's most famous dish

Liked ‘The Bear’? Eat your way around Chicago with these iconic dishes

A taste of the South of France, from tapenade to ratatouille

Meet Mory Sacko, the chef shaking up Paris's fine-dining scene

Eat your way around the world with these 6 food travel books
- History & Culture
- Photography
- Environment
- Paid Content
History & Culture
- Women's History Month
- History Magazine
- Women of Impact
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Cent Nerv Syst Dis
Recommendations for traveling to altitude with neurological disorders
Marika falla.
1 Institute of Mountain Emergency Medicine, Eurac Research, Bolzano, Italy
2 Center for Mind/Brain Sciences, CIMeC, University of Trento, Rovereto, Italy
Guido Giardini
3 Mountain Medicine and Neurology Centre, Valle D’Aosta Regional Hospital, Aosta, Italy
Corrado Angelini
4 Department Neurosciences, University of Padova, Padova, Italy
Several neurological conditions might worsen with the exposure to high altitude (HA). The aim of this review was to summarize the available knowledge on the neurological HA illnesses and the risk for people with neurological disorders to attend HA locations.
A search of literature was conducted for several neurological disorders in PubMed and other databases since 1970. The neurological conditions searched were migraine, different cerebrovascular disease, intracranial space occupying mass, multiple sclerosis, peripheral neuropathies, neuromuscular disorders, epileptic seizures, delirium, dementia, and Parkinson’s disease (PD).
Attempts were made to classify the risk posed by each condition and to provide recommendations regarding medical evaluation and advice for or against traveling to altitude. Individual cases should be advised after careful examination and risk evaluation performed either in an outpatient mountain medicine service or by a physician with knowledge of HA risks. Preliminary diagnostic methods and anticipation of neurological complications are needed.
Conclusions
Our recommendations suggest absolute contraindications to HA exposure for the following neurological conditions: (1) Unstable conditions–such as recent strokes, (2) Diabetic neuropathy, (3) Transient ischemic attack in the last month, (4) Brain tumors, and 5. Neuromuscular disorders with a decrease of forced vital capacity >60%. We consider the following relative contraindications where decision has to be made case by case: (1) Epilepsy based on recurrence of seizure and stabilization with the therapy, (2) PD (± obstructive sleep apnea syndrome-OSAS), (3) Mild Cognitive Impairment (± OSAS), and (4) Patent foramen ovale and migraine have to be considered risk factors for acute mountain sickness.
Introduction
There is an increasing interest in exploring location situated at high-altitude (HA) for leisure, sports (mountain climbing and alpinism), or work (astronauts, aviation, health care service, and alpine rescue) therefore, is not unusual to encounter people who develops acute symptoms related the HA exposure. The diverse extent of symptoms presentations is mainly due to the altitude reached and the ascending speed. During clinical practice, neurologists may also need to evaluate the risk or to advise people with pre-existing neurological disorders that are willing to going to HA areas.
The aim of this review is to summarize the available knowledge on (i) the neurological high-altitude illnesses (HAI), (ii) the risk of developing neurological symptoms at HA other than HAI, and (iii) the risk for people with neurological disorders to attend HA locations.
Physiological effects of low oxygen
Altitude is classified as low (500–2000 m), moderate (2000–3000 m), high (3000–5500 m), or extreme (>5500 m). 1 The main environmental modification with the altitude increase is the progressive reduction of the barometric pressure, being usually of 760 mmHg at sea level and around 523 mmHg at 3048 m above sea level. According to the barometric pressure decrease, also the atmospheric oxygen partial pressure (PO 2 ) decreases and remains always around 20.93% of the total barometric pressure (159 mmHg at sea level and 67 at 3048 m). Those modifications are termed hypobaric hypoxia (HH). The main human physiological consequence of going high is the reduction of the alveolar oxygen (O 2 ) which differs in acclimatized vs non-acclimatized individuals.
The acute exposure to HH induces alveolar hypoxia that causes the hypoxic pulmonary vasoconstriction to direct blood towards lungs areas better oxygenated. The hypoxemia activates the arterial chemoreceptors (aortic and carotid bodies), whose fibers reach the nucleus tractus solitarius and the dorsal motor nucleus of the vagus nerve, increasing the alveolar ventilation to 1.65 times normal and with prolonged stayed up to 5 times normal. The increased ventilation determines transient hypocapnia and increase pH which in turns inhibit the bulbar (brainstem) respiratory center.
This response fades away in 2 to 5 days due to the metabolic gradual compensation induced by the kidneys with a gradual decrease in bicarbonate (compensatory metabolic acidosis). The bicarbonates are also reduced in the cerebrospinal fluid (CSF) and in the cerebral tissue thus decreasing the pH in the fluid around the chemosensitive neurons of the respiratory centers that are stimulated. 2 Hypoxia and hypocapnia have opposing effects on cerebral blood flow. Hypoxia increases CBF, 3 - 5 while hypocapnia decreases it. 5
The hypoxemia stimulation of the chemoreceptor also induces cardioacceleration through an increased sympathetic activity that leads to an increase of heart rate, cardiac output and blood pressure.
Brain under hypoxia is protected till a critical threshold through different physiological mechanisms including the autoregulation and the increase of oxygen extraction which allows normal energy metabolism to be maintained. Autoregulation consists in vasodilatation (small pial vessels and large intra- and extracranial vessels) and reduction in cerebral vascular resistance during reduced cerebral perfusion to maintain the cerebral blood flow (CBF) constant or to increase CBF when also energy failure and/or a decrease in hemoglobin level are present. 6 However, acute hypoxia may induce functional changes such as an impaired cerebral autoregulation, 7 an increase of cerebral blood flow 8 , and vascular permeability. 9
The prolonged exposure to HA determines a gradual acclimatization mainly due to the increased erythrocytes’ number (red blood cells) and hemoglobin concentration, increased pulmonary ventilation and diffusion capacity, increased angiogenesis in the peripheral tissue and increased cells O 2 utilization/extraction despite the low PO 2 . Hypoxia also induces the production of the hypoxia-inducible factors (HIFs) which activate several genes encoding proteins necessary to ensure O 2 delivery for the tissue energy metabolism (genes related to endothelial growth factors and glycolytic enzyme, erythropoietin and mitochondrial genes, and genes that increase the production of nitric oxide).
The unique alveolar PO 2 measurement at 8400 m was performed by Grocott and colleagues 10 and they found a value of 43.1 mmHg with a barometric pressure of 253 mmHg.
Further maladaptive physiological brain effects have been shown in individuals after sojourns to HA.
Among structural changes there are white matter abnormalities, 11 , 12 reduced grey matter volume 13 and microbleeds due to hemosiderin deposit. 14
Neurological manifestations related to the acute high altitude exposure: high altitude illnesses
Several factors are implicated in the appearance of neurological manifestations.
The rate of ascent, the altitude reached, the individual predisposition, and the physical effort along with others such as the temperature, the dehydration, the wind, and the exposure to solar radiation all may provoke typical neurological symptoms related to the HA exposure and overall defined as high HAI. 15
The HAI include the HA headache (HAH), the acute mountain sickness (AMS), and the high altitude cerebral edema (HACE). The rapid ascent to HA in few people is the major determinant of the HAI. Several drugs are recommended to prevent or treat HAI, 16 and possible interaction of those drugs with preexisting neurological conditions and potential development of new neurological condition during exposure to HH are summarized in Table 1 .
Drugs used for prevention and treatment of high-altitude illnesses and interaction with drugs used in neurological conditions.
AEDs: antiepileptic drugs; AMS: acute mountain sickness; COX-2: cyclooxygenase-2; CBZ: carbamazepine; FANS: HACE: high altitude cerebral oedema; HAPE: high altitude pulmonary oedema; NSAIDs: non-steroidal anti-inflammatory drugs; PHT: phenytoin; PB: phenobarbital; SSRIs: Selective Serotonin Reuptake Inhibitors; VPA: valproic acid.
References: Luks AM, Auerbach PS, Freer L, Grissom CK, Keyes LE, McIntosh SE, Rodway GW, Schoene RB, Zafren K, Hackett PH. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update. Wilderness Environ Med. 2019 Dec;30(4S):S3-S18. doi: 10.1016/j.wem.2019.04.006.
Patsalos PN, Perucca E. Clinically important drug interactions in epilepsy: interactions between antiepileptic drugs and other drugs. Lancet Neurol. 2003 Aug;2(8):473-481. doi: 10.1016/s1474-4422(03)00483-6.
High altitude headache
The International Headache Society stated that >30% of the individuals that goes to high altitude (>2500 m) has HAH that typically develops in temporal relation to the ascent to HA and resolved within 24 hours after descent. 17 About 80% of lowlanders are susceptible to HAH at an altitude above 3000 m and almost 100% above 4500 m. 18 HAH is usually bilateral, of mild to moderate intensity, and it is aggravated by exertion, movement, straining, coughing, and/or bending. Risk factors include a history of migraine, low arterial oxygen saturation, high perceived degree of exertion, restrictions in venous outflow, and low fluid intake (<2 L in 24 hours). HAH usually subsides with analgesic (ibuprofen or paracetamol) hydration and avoiding further ascent, if those measures are not efficacious rapid descent should be advised.
Acute mountain sickness
The AMS can manifest in around 30-50% of the unacclimatized individuals that goes to HA (>2500 m), but in susceptible individuals even at lower altitude. 19 The incidence of AMS is higher for those that had a previous AMS and increases with the altitude, being less frequent below 2500 m (10-25%) and more frequent above 3000 m (up to 75%). Based on the recent consensus update, AMS manifests with nonspecific symptoms such as headache, which is the leading symptom required for the diagnosis, gastrointestinal symptoms (nausea or vomiting), fatigue/weakness, and dizziness/light-headedness whereas the sleep disturbances were removed from the previous score due to a repeatedly reported discordance of sleep from other AMS symptoms. AMS symptoms start to appear usually between 4 to 12 hours after arrival at HA. The presence of AMS is defined as a Lake Louise AMS Score ≥3 from the four rated symptoms. 19 The new LLS also gives the score related to the impact of AMS on overall function at HA (AMS Clinical Functional Score). Slow ascent, preacclimatisation and other pharmacological approaches to prevent, diagnose and treat AMS are discussed elsewhere. 16 , 20
High-altitude cerebral edema
Leading neurological findings are truncal ataxia and altered mental status and in addition the presence of different other focal symptoms or psychiatric changes preceded or not by headache or AMS symptoms. 16 HACE represents a life-threatening form of acute HAI, that can be preceded by AMS or not, 21 and if this condition is not treated promptly it can result in death which can occur rapidly due to brain herniation. 22 Around 1-2% of individuals can develop severe symptoms compatible with the HACE that usually start between 24 to 72 hours after a gain in altitude. Immediate descent, oxygen, and dexamethasone administration are crucial. When rapid descent would not be possible due to the weather conditions, challenging terrain, or the presence of injuries or wounds, a portable hyperbaric chamber could be used if the airway can be protected. An MRI study on 9 individuals with HACE showed, in 7 of them in the acute phase, T2 increased signal in the splenium of the corpus callosum that resolved in subsequent MRI study and all individuals had clinical recovery. 23 In patients survived from HACE, microbleeds were identified on susceptibility weighted images (SWI) in the cerebral white mater tracts. 9 This imaging data are related to vasogenic (extracellular) edema partly due to the breakdown of the blood brain barrier (BBB) and endothelial dysfunction. There are also reports of irreversible consequences of HACE, such as subcortical dementia and neuropsychiatric symptoms 24 and personality changes, 25 due to the hypoxia and the presence of lesions in the globus pallidus on MRI.
Neurological manifestations due to repetitive or chronic exposure to HA
Beyond these acute neurological manifestations, also chronic complications have been reported.
White matter hyperintensities
The white matter hyperintensities (WMHs) are nonspecific findings and commonly seen on MRI in normal aging with an increased prevalence with increasing age (10-20% at 60 years and near 100% above 90 years). WMHs are supposed to represent chronic small vessel cerebrovascular disease 26 and are also seen in association with different neurological conditions (e.g., migraine). 27 The presence of several risk factors may contribute to the progression of the WMHs in terms of volume and number and the progression over time is related to different neurological consequences (e.g., cognitive decline and gait abnormalities).
The presence of WMHs, observed on T2-weighted fluid-attenuated inversion recovery (FLAIR) images along with the diffuse reduction in WM integrity measured by diffusion tensor imaging (DTI), has been documented in extreme mountaineers who climbed over 4800 m, 23 , 28 , 29 in pilots 30 and in altitude chamber operations technicians 31 after repeated acute exposure to an altitude above 7260 m. 31 A retrospective study on 301 Tibetan patients residing at HA showed a high prevalence of WMHs and their presence was correlated with a younger age. 32 They also found an independent association of WMHs with several cardiovascular risk factors (e.g., hypertension, atrial fibrillation, and chronic cerebral infarction) but they failed to demonstrate an association with the hemoglobin level despite the higher levels present in Tibetans.
Chronic mountain sickness
The chronic mountain sickness (CMS) or Monge’s disease 33 can develop in certain individuals that permanently live or are natives at HA (>2500 m). Worldwide there are around 140 million of individuals that live above 2500 m, of them 17 million live above 3500 m and 4 million above 4500 m and 5–10% are at risk to develop CMS. 34 The CMS prevalence depends on the altitude of residence and the population ethnicity since it has been demonstrated a different genetic adaptation to hypoxia in the different highlanders’ populations. In the Andine HA residents, the CMS incidence and the erythrocytosis are increased 33 compared to Tibetan and Ethiopian. CSM is characterized by excessive erythrocytosis and severe hypoxemia which can lead to pulmonary hypertension and eventually congestive heart failure. Respiration is disordered during sleep, with episodic hypopnoea and apnoea. Individuals living at HA experience troublesome burning pain distally in the limbs. 35 The diagnosis is based on the presence of different symptoms such as headache; dizziness; breathlessness; and/or palpitations; sleep disturbances; fatigue; localized cyanosis; dysesthesia in the hands, palm, and foot soles; and reduced concentration and cognitive performance. CMS gradually disappeared with descent to lower altitudes. 36
Test to predict acute mountain sickness susceptibility
A recent work describes the possible use of a hypoxia-test to detect subjects susceptible to severe HAI. With a decision algorithm based on a clinicophysiological score the physician with experience in high altitude medicine can advise on progressive acclimatization and prescription of drugs, such as acetazolamide, people who plan travel to altitude. 37 With the aid of this hypoxia submaximal exercise test the occurrence of severe HAI was reduced from 27% to 12% with correct recommendations. Other tests are present in literature with similar indications like a rest test both on the field or in simulate environment. 38
Other neurological manifestations at HA and risks of exposure at HA for those with preexisting neurological conditions
Several neurological symptoms, in particular cerebrovascular accidents and seizures have been reported with high frequency at HA but their relationship with the HA exposure is not yet completely understood. The role of hypoxia is considered to be prominent.
In this section and the following paragraphs, we are going to discuss (i) different neurological conditions documented at HA that could present with or without any signs or symptoms of HAI and (ii) the possible worsening of the underlying disease in patients with preexisting neurological disorders when travelling to HA. Previous revision was done by Baumgartner et al 39 and Basnyat et al. 40 Therefore, we are going to update the current evidence and attempts are made to classify the risk posed by each condition and to provide recommendations regarding medical evaluation, advice for or against travelling to altitude, and effective prophylactic measures. 41 Unstable neurological disorders [e.g., brain tumor, recent transient ischemic attack (TIA), or stroke] are a contraindication for travel to HA due to a possible worsening and a recovery impairment. In case of stable neurological conditions, the possible effect of exertion in addition to the hypoxia effect should be considered. Detailed anamnesis, neurological examination, and the presence of comorbidities should be carefully considered and case by case individually discuss to provide correct advice (e.g.,, passive or active ascent) in an outpatient mountain medicine service or by a physician with knowledge of travelling and HA risks. Development in diagnostic methods and treatment of neurological conditions are also mentioned. Based on the risk due to the pre-existence of neurological disorders, attempts will be made to provide recommendations to correctly advise for or against travelling to HA.
Literature and research methods
A search of the literature was conducted for several neurological disorders in PubMed and other databases. The studies were selected according to the following eligibility criteria: articles published before March 2021 and currently published journal articles. PubMed was used as the primary information source, but other databases were included in the search such as EMBASE, Web of Science, Cochrane Library to identify publication on HA exposure in patients with neurological disorders, with emphasis on clinical neurological series or individual cases reported at HA, from the early ‘70 to March 2021, without language restrictions. The following MeSH terms and/or keywords were used: high altitude, mountain travelling, hypoxia, neurological conditions searched were migraine and other types of headaches, transient ischemia of the brain, occlusive cerebral artery diseases, intracranial hemorrhage and vascular malformations, intracranial space occupying mass, multiple sclerosis, peripheral neuropathies, neuromuscular disorders, epileptic seizures, dementia and Parkinson’s disease.
Cerebrovascular diseases
Stroke, hemorrhagic or ischemic, is defined as a relatively sudden occurrence of a focal neurological deficit.
Ischemic stroke
Ischemic stroke is usually due to the occlusion of a cerebral blood vessel that cause cerebral infarction. The occlusion could be due to atherosclerosis with superimposed thrombosis affecting large cerebral vessels, cerebral embolism, and occlusion of the small vessels. Hemodynamic stroke is a type of ischemic stroke that is caused by hypoperfusion. In other situation the ischemic damage is associated with other pathophysiological mechanisms: arterial dissection, inflammation (i.e., vasculitis), cerebral veins or dural sinuses thrombosis, hypercoagulable conditions, vasospasm and emboli of various origin (i.e., fat, cholesterol, and tumor). Ischemic stroke at HA have been reported and may be related with polycythemia, reduce plasma volume, dehydration, prothrombotic state, or impaired cerebral vascular autoregulation. Ischemic stroke could be also a complication of HACE. 42 The hematocrit and hemoglobin levels increase with the altitude resulting in polycythemia which represents an independent risk factor for stroke. 43 , 44 Dehydration together with polycythemia contributes with consequent “inspissation sanguinis.” Hypoxia may also determine endothelial dysfunction, coagulation abnormalities and platelet aggregation 45 , and cardiac arrhythmias. 46
Contradictory results have been reported in the literature on the relationship between chronic HA exposure and stroke possibly related to the heterogeneous ethnicity and different prevalence of specific cardiovascular risk factors, exposure to HA (transiently or since birth), and ethnic lifestyle habits (e.g., diet). The first report is from Sharma et al 47 in a small study of 13 stroke patients occurred after long stay (3 to 18 months at > 3000 m) and they observe in young patients an increased level of platelet adhesiveness. A higher prevalence of acute ischemic stroke (>anterior circulation) was reported in younger Tibetan (Tibet 3650 m) compared to Chinese lowlanders (Beijing 40 m) and the authors suggested that erythrocytosis and hyperhomocysteinemia possibly contribute to these differences. 48 Another retrospective study reported that the first-ever acute ischemic stroke in Tibetan plateau residents were more severe and showed a larger infarct volume and less artherosclerotic factors, suggesting a prevailing risk related to the hypercoagulable state due to polycythemia (reduced blood flow and increase peripheral resistance) and an increased hypoxia-inflammatory response at HA. 44 First ever ischemic stroke due to polycythemia induced by chronic HH (>4000 m) exposure have been reported in Indian soldiers more frequently at high compared to low altitude (13.7 vs 1.05/1000). 49 A study found an increased frequency of thrombotic stroke at HA in Saudi Arabia (Al Baha >2000 m vs Riyadh 620 m) probably due to increased hematocrit in conjunction with other factors (e.g.,, hypertension). 50 Another study suggests a higher incidence of stroke in Pakistani highlanders (>4500 m) compared to lowlanders (600 m). 51 Recently was published a case of stroke occurred in a 44-year-old experienced Sherpas climber who resides at HA (3800 m). 52 On the contrary, few epidemiological surveys conducted at different altitude suggested that cerebrovascular disease may be less frequent than at sea level. Razdan et al 53 performed the survey in the Kashmir region of South India (1530 m) among rural population. Cruz et al 54 performed a survey in Quiroga (Ecuador at 2300 m). Bancaleri et al 55 suggested a low stroke prevalence in Cerro de Pasco (Perù 4300 m). Kuller et al 56 reported a lower stroke rate at different HA locations compared to sea level in the United States. A lower incidence of stroke was found in a hospital in the Sub-Himalayan region India (Himachal Pradesh at 2200 m). 57 These discrepancies between studies may be due to other factors (e.g., others environmental stressor such as pollution in urban areas) and could be related to individual comorbidities in certain population. Furthermore, it has been suggested that HIF determines resistance against ischemia and improved cardiac function after ischemia. 44
Several authors have reported ischemic stroke cases with the acute HA exposure in healthy subjects without any known risk factors (>4500 and 3600 m, respectively). 58 , 59 In the presence of deep vein thrombosis, a cryptogenic stroke due to a paradoxical embolism should be considered as a consequence of the increased pulmonary vascular resistance and arterial pressure due to the hypoxic vasoconstriction at HA which increased the likelihood of right to left shunting in those with a patent foramen ovale (30% healthy population). Indeed, embolic etiology was suspected in cases reported in the literature due to the presence of a large patent foramen ovale (3840 m). 60 , 61 Cases of deep venous thrombosis and associated pulmonary and cerebral embolism have been also reported, probably due to the increased prothrombotic state (4270 to 5790 m). 62 , 63
Since dehydration, immobility or strenuous exercise may predispose to thrombosis it is recommended adequate hydration and exercise maintaining during altitude sojourn. Acclimatization is also essential to avoid HAI which may contribute to the reduced CBF. Recent data found that the risk of a second stroke or TIA after a minor stroke or TIA is 2.1% at 7 days, 2.8 at 30 days, 3.7% at 90 days, and 5.1% within 1 year. 64 A patient with previous TIA should be informed that the best treatment in case of recurrence is thrombolysis (when possible) and dedicated treatment in a stroke unit that may be difficult to be available in HA location or in adverse environment.
Cerebral venous thrombosis
The occlusion of cerebral venous sinuses and/or the tributaries cortical veins produces a venous ischemic stroke. Cerebral venous thrombosis (CVT) also cause raised intracranial pressure through decreased cerebrospinal fluid (CSF) absorption. The clinical presentation ranges from minor to life threatening depending on the site of venous occlusion (e.g., veins or sinus) and consequently the extent of brain parenchyma involvement and the effect of ICP. The clinical course is slower compared to the ischemic stroke, it is usually accompanied by headache and focal neurological deficit and complicated with seizures and hemorrhages and on neuroimaging are often visible multiple cerebral lesions not in arterial territories. Commonly affected sites are superior sagittal sinus (62%), transverse sinus (45%), sigmoid sinus (rare in isolation), and deep veins (internal cerebral veins, basal vein of Rosenthal, vein of Galen, and straight sinus). At HA all these sites involvement have been reported. 65 , 66
Main risk factors at sea level are the hypercoagulable conditions (congenital or acquired thrombophilias) with thrombocytosis and hyperfibrinogenemia, head injury with direct venous trauma, estrogen-containing oral contraceptives, pregnancy and puerperium, infections, malignancy, and inflammatory disease. At HA other mechanisms include dehydration, hypoxia-induced hemostatic changes such as an increased platelet activity, volume depletion and secondary polycythemia, reduced mobility, inflammatory changes secondary to endothelial injury that accelerates the thrombotic process, hyperhomocysteinemia, exercise, and coagulation pattern triggered by hypothermia. 67 These hemostatic changes do not appear during gradual ascent up to 45000 m, 68 therefore other mechanism may play a prevalent role such as the effect of the increased cerebral volume on CBF. 69
CVT was reported in a necropsy of seven trekkers who died after HACE and/or HAPE while trekking in Himalayas. 22 The seven cases reported occurred after few days to few weeks of staying at an altitude range between 3440 and 6300 m asl. Cheng et al 70 reported a case of CVT with a poor neurological outcome occurred after 4 days at 4000 m without any known risk factors. Khattar et al 71 described 21 cases (2 died) of CVT; however, it is not specified the altitude and the length of stay at altitude; they observed a higher incidence of alcoholism (76%) in their retrospective cohort while a lower incidence of other comorbidities such as oral contraceptives (14%) and trauma (10%). Paliwal et al 65 described 4 cases (1 died) occurred at an altitude ranging from above 3000 to 3800 m asl without specifying the length of stay.
Other authors reported CVT cases occurred after several weeks of stay at HA. Song and colleagues 69 analyzed cerebral thrombosis at HA in their case and cases reported in the literature and they confirmed that all were mountaineers exposed for more than 3 weeks at HA (>5000 m) and all had cerebral thrombi of venous origin likely related to volume depletion and polycythemia. 69 Hassan et al 72 analyzed 28 cases of CVST occurred at an altitude >3000 feet but mostly (85.7%) > 8000 feet where they reside for >1 week; 27 had a good outcome and found overall a high level of hemoglobin and D-dimer and suggest that smoking and dehydration were the possible reversible risk factors in their cohort. Khan et al 73 reported a case of CVT due to deep cerebral vein thrombosis occurred in an otherwise healthy young man (20-year-old) after two weeks of stay at 4000 m asl.
Several authors reported CVT at extreme HA [>7200 towards Cho Oyu (8201 m), >5000 m towards Gasherbrum I (8068 m), Mount Everest at 8848 m and at 8511 m] with a length of stay ranging from 20 to 45 days. 66 , 74 - 76 Interestingly, while Khanal et al 66 reported the involvement of the right transverse and sigmoid sinus in a subject with low protein S plasma activity, all the other authors reported the involvement of the superior sagittal sinus in subjects without any known risk factors. 74 - 76 Familial thrombophilia (protein S or C deficiency, heterozygous Factor V Leiden mutation) was identified as the cause of few CVT case reports occurred between 3000 and 8848 m asl. 66 , 77 - 79
A case of CVT in a young woman working in a high-altitude chamber as instructor have been reported and mostly related to the oral contraceptive assumption. 80
CVT is a challenging condition due to its wide range of clinical presentations. The persistence of headache and focal neurological symptoms after descent suggests to always evaluates the possibility of CVT, especially in those predispose (e.g., due to thrombophilia), including a magnetic resonance venography to the neuroimaging stroke workup. The presence of multiple hemorrhagic infarctions in one hemisphere without atherothrombosis or embolism source suggest a cortical vein origin. Careful history and medical screening should be performed individually before going to altitude. There are no evidence-based guidelines to make firm recommendations; however, it should be considered to advise all travelers to HA to drink adequately (2-3 L of water/day) to avoid dehydration and hyperviscosity, avoid strenuous activity at high summit and those with known predisposing factors to thrombosis to avoid altitude sickness (e.g., HACE and the increased ICP which further compromise the CBF) considering all the measures that are helpful (e.g., acclimatization and specific treatment). In addition, women on oral contraceptives should consider the risk of being exposed to HA.
Reversible cerebral vasoconstriction syndrome
Reversible cerebral vasoconstriction syndrome (RCVS) is characterized clinically by severe headache (hyperacute and excruciating) with or without fluctuating neurological symptoms (TIA-like episodes) or seizures associated with reversible vasoconstriction of the medium and large cerebral vessels. 81 Known risk factors are eclampsia, peripartum period, the use of vasoactive substances (including triptans and selective serotonin reuptake inhibitors), and strenuous exercise but also an idiopathic variety exist. The suggested mechanism is a transient disturbance in the control of cerebral sympathetic vascular tone. 81 Recently two cases were reported of RCVS developed acutely at HA suggesting that also altitude may provoke it (1200 and 3650 m). 82 , 83 Therefore, this condition should be considered in the differential diagnosis, given its reversibility when the main cause is revealed and adequately treated. Although the pathophysiology is still poorly understood it may be useful to recommend avoiding at HA adjunctive possible risk factors such as all vasoactive substances (e.g., nasal decongestants, selective serotonin reuptake inhibitors, or SSRI).
Posterior reversible encephalopathy syndrome
There is an acute increased perfusion and blood pressure (BP) increase after few hours at altitude which remains higher during HA sojourn and further increased with the increased altitude as demonstrated in the HIGHCARE-Himalaya study. 84 Due to the elevated hypoxic peripheral and central chemoreflex sensitivity, 85 , 86 hypertensive individuals may be more susceptible to HA deleterious effects.
Hypertensive encephalopathy can develop in such individuals presenting with headache, seizures or focal neurological signs and edema in the subcortical white matter which is usually reversible although hemorrhage or infarction may occur.
Posterior reversible encephalopathy syndrome (PRES) presents with severe headache, nausea, or vomiting, with or without neurological symptoms mainly referable to the parietal and occipital lobes (e.g., visual field deficits, hallucinations, confusion sometimes leading to seizure and coma) due to severe hypertension (diastolic pressure >125 mmHg). 87 The clinical presentations are variable depending on the underline etiology. A multifocal vasoconstriction of the cerebral arteries is implied and typically resolves in 1 to 3 months. The hypertension leads to cerebral autoregulatory failure and vasodilation with interstitial fluid extravasation and vasogenic edema 88 with a predilection for the posterior circulation thought to be related to the lack of sympathetic activity. 89 When promptly recognized and treated, the symptoms and radiological abnormalities can be completely reversed, otherwise the symptoms progress to ischemia with large infarction and death. Given its reversible nature when promptly recognized, it is of a paramount importance to consider it in the differential diagnosis including a magnetic resonance angiography in the neuroimaging workup.
Hemorrhagic stroke
The hemorrhage occurs within the brain parenchyma (i.e., intracerebral hemorrhage) or within the subarachnoid space and ventricular system (also termed subarachnoid hemorrhage). The main cause of intracranial hemorrhage is considered the arterial hypertension that may worsen at HA due to cardiovascular response to HA 90 but in patients with amyloid angiopathy there is the risk of high recurrence of lobar hemorrhage even at sea level and therefore these patients should not be recommended to ascent to HA. In case of recent acute neurological events patients should not ascend to HA. In case of previous hemorrhages, the situations need to be carefully evaluated considering comorbidities and stable conditions.
There are few data on the frequency of cerebral intracranial hemorrhage at HA. Intracranial hemorrhage is the most frequent stroke subtype reported on the Tibetan plateau in China (74.1%). 91 A prospective hospital-based study investigated the main cause of intracranial hemorrhage (ICH) and outcomes in Tibetans and found that most of the cases are caused by hypertension and that those patients are at greater risk of disability or disability/death on follow-up compared with patients from the area of Chengdu located at low altitude. 92 A nontraumatic subdural hematoma case has been reported following acute HA exposure. 93
Subarachnoid hemorrhage
At HA there is an increasing blood flow and augmented capillary permeability related to the brain adaptation to HA. The adjunctive role of the decreased barometric pressure may increase the aneurysm or arteriovenous malformations rupture event.
Subarachnoid hemorrhage (SAH) is usually related to an aneurysm rupture due to increased pressure which force the blood into the subarachnoid space. Aneurysm of 10 mm or more of diameter are more susceptible to rupture being the likelihood of rupture those smaller than 10 mm between .05% and .7% per year. 94 , 95 Risk factors includes hypertension, physical activity (e.g., sexual activity), straining at stool or during natural delivery, sometimes even due to coughing or sneezing. The leading symptoms is the headache usually refers by the patients as the “worse ever had” and various degree of altered mental status which make the differentiation with HACE difficult. SAH were reported in a necropsy of seven trekkers died after HACE and/or HAPE while trekking in Himalayas. 22 The bleeding risk of aneurysm, arteriovenous malformations and cavernous hemangiomas at HA is not yet determined. A case report of bleeding from a middle cerebral artery aneurysm has been reported in an acclimatized man who develops suddenly severe occipital headache and after 1 hour loss of consciousness upon descent (from 4700 to 4200 m) and subsequent gradual (over days) progression of neurological symptoms. 96 Two cases were reported of SAH due to a small (4 mm diameter) aneurysm rupture, one developed in a man during air travel landing 97 and the other developed both before and after landing. 98
Recommendations for patients with history of recent/past ischemic and hemorrhagic stroke or transient ischemic attacks
For patients with a recent stroke (less than 90 days) data are lacking regarding the safety of trekking to HA therefore it is not recommended to go to mountain. For patients with previous stroke several aspects are worth considering: (i) the definite diagnosis based on clinical history and neuroimaging, (ii) a stable control of risks factors (arterial hypertension, hypercolestherolemia, hyperglycemia, metabolic syndrome, anticoagulants for atrial fibrillation, smoking habits).
Further, (iii) in those with atherothrombotic stroke it is recommended a carotid ultrasound within the previous 6 months, to prevent the risk of HA complications in a plaque or a severe stenosis, (iv) for those with cardioembolic stroke a cardiological evaluation with echocardiography it is recommended and novel oral anticoagulants in those with non-valvular atrial fibrillation are preferable to warfarin in a remote environment, (v) in those with a cryptogenic stroke further evaluations including coagulation abnormalities study or patent foramen ovale exclusion are needed.
TIA is often a clinical diagnosis which suggests that such patients should not trek or climb at HA alone. It is important to consider that loss of consciousness, dizziness, falls, amnesic or confusional episodes as isolated symptoms are not necessarily TIA.
Arterial hypertension is the main cause of hemorrhagic stroke and HA increases blood pressure leading to adverse effects on cerebral aneurisms and arterial venous malformations. Patients with amyloid angiopathy are at risk of lobar hemorrhage, therefore patients with such conditions are advised to avoid altitude. A moderate or severe disability post-stroke measured with the Rankin scale (>2) is a contraindication to visit a wild environment. It is advisable to encourage patients with previous stroke (but this applies to most neurological patients) to avoid trekking alone.
The occasional occurrence of syncope is reported over 3000 m in non-acclimatized persons, this is in relation to vasovagal stimulation, and we will only mention that some cases might be susceptible to drug treatment. Nicholas et al 99 reported 94 cases seen in healthy young adults in an emergency room over 12-month in Colorado (3293 m) that mainly occurred in the first 24 hours of HA reached and they named it high-altitude syncope (HAS) . HAS is usually benign and differently from a seizure the patient usually shows a rapid recovery with no prolonged confusion or disorientation. Freitas et al 100 reported a case of a young women with repeated syncope while climbing at HA (>2000 m) confirmed to be of neuro-cardiogenic origin (positive 70° head-up tilt test) and successfully treated with beta blockers (atenolol 50 mg).
Acute hypoxia exposure induced increased sympathetic activity that increased cardiac output to maintain arterial oxygen content. The sympathetic vascular tone control and baroreceptors responsiveness are suggested mechanisms underlying neurogenic syncope. Indeed, an increased sympathetic activity prior to syncope has been shown using microneurography and heart rate variability studies and this activity ceased at syncope onset. 101 Moreover, vascular resistance is reduced prior to syncope which is thought to be due to the initial adrenergic discharge that at high levels cause vasodilatation in intramuscular blood vessels. Prolonged sympathetic activation induces downregulation of beta-adrenergic receptors as shown during exercise in chronic hypoxia. 102
Transient global amnesia
Transient global amnesia (TGA) is a syndrome characterized by memory loss (e.g., anterograde memory) and confusion/disorientation lasting from 30 minutes up to 24 hours. 103 Four TGA cases related to HA have been described in the literature (altitude range between 2000 and 5500 m; length of stay at altitude range between 1 to 10 days), enough to deserve the definition of HA global amnesia. 103 - 105 TGA is often triggered by the effort and sometimes associated with emotional factors. Hypoxia could play an adjunctive etiological role, predominantly affecting memory circuits (Papez circuit), and further aggravate by the hypocapnia resulting from the hypoxic ventilatory response (HVR) that induces cerebral vasoconstriction. 105 TGA occurs frequently on the first or the second day of vacation and it has been found to be associated with high blood pressure levels. Those patients can be examined in hospitals located near ski resorts or mountain huts. In the differential diagnosis, an untested head injury or an acute cerebrovascular event should be considered if the memory deficit does not regress and focal signs are present. Prognosis is benign as in cases occurring at low altitudes and relapses are rare. An association with patent foramen ovale has been described. A previous and unique TGA is not a contraindication for altitude travel or flying. In case of recurrence a specific advice is needed by an expert physician.
In the general population, migraine is a widespread disease, with a prevalence of about 12%, which can reach 22-25% in women of childbearing age. HH is certainly a trigger for migraine attacks. 106 Some epidemiological data suggest an increased prevalence of migraine in HA populations 107 but also a worsening of both frequency and intensity of migraine episodes in low altitude residents during trekking or long flights. 108 There seems to be no difference between migraine without (M) or with aura (MA). M does not present an increased risk of developing cerebrovascular events, while in MA this risk is significantly increased even in young people with associated risk factors, such as smoking and oral contraceptive therapy.
During a mountain medicine consultation, it is common to evaluate people with migraine who ask advice for traveling at HA or who have already experienced a worsening of their headache. It is not easy to distinguish between HAH also associated with AMS and migraine crises, 109 therefore a neurologist with specific experience is needed. The presence of additional symptoms in AMS may help since the Lake Louise score define AMS as the presence of headache plus one or more adjunctive symptoms (anorexia, nausea/vomiting, fatigue, dizziness/vertigo) in an unacclimatized person who rapidly ascend >2500 m. Headache is usually bilateral and described as stabbing or dull pain whereas migraine typically is unilateral and describes as throbbing or pulsing pain. Since migraine can worsen at HA, patients with an increase and high frequency of migraine attacks particularly those with MA should be referred to a specialist before planning to visit HA locations. When migraine patients plan to do a trekking, expedition or even a long HA trip, they must have an adequate amount of symptomatic and prophylactic drugs in the bag. The use of triptans seems to be safe. 110 One study suggested some usefulness of triptans in AMS prevention. 111 However, a recent Cochrane review degraded the evidence of the latter study due to low quality and imprecision. 112 Acetazolamide can also be effective in migraine prevention. Patients with MA should adequately check and control vascular risk factors (e.g., thrombophilic state) and stop smoking. Estrogen is an absolute contraindication, even at low altitudes. In patients with migraine and atypical aura (multiple aura symptoms: visual, sensory, speech and/or language, motor, or autonomic) prolonged over several hours to 3 days) especially if it is the first attack and after age 40 and predominantly negative symptoms (e.g., hemianopia), a brain MRI with DWI study should be performed before travel to disclose recent embolic subclinical strokes. In addition, a transcranial Doppler to disclose a patent foramen ovale (PFO) or the presence of a right to left shunt should be also preventively performed even though there are no data on the efficacy of the closure of PFO in the prevention of stroke at high altitudes in those patients. A small study suggests that PFO is a possible risk factor for HAPE. 113
Delirium and high altitude psychosis
Delirium is an acute modification of cerebral function in response to stressors (e.g., acute illnesses, drug, or alcohol intoxication) and develops over a short time (hours to days). Delirium manifests with confusion and reduced concentration, insomnia, overactivity, tremor, vivid hallucinations, and sometimes excessive sympathetic activity (flushed face, dilated pupils, injected conjunctivae, rapid pulse and blood pressure rise, increased sweating). Delirium can be induced by hypoxia 114 but other causes related to HA have been suggested to be implicated, the hypocapnia-induced vasoconstriction and alkalosis. 115
Delirium in mountain climbers may appear as described in several cases reported in the literature (altitude >7000 m). 116
Hallucinations and other psychotic symptoms may appear at HA with or without other symptoms of delirium or HACE. 117 Isolated HA psychosis in climbers have been reported (e.g., the “third man” phenomenon) at an average altitude 7280 m and to disappear upon descent, but it is associated with an increased risk of accidents. 117 If rapid descent is not possible antipsychotic should be given or cognitive strategies (e.g.,, reality testing) can be adopted by the affected climbers or by a partner. 118 Organic causes need to be rapidly excluded.
Depression, anxiety, and insomnia
The presence of depression is either pre-existent or caused by HA exposure and according to Hüfner et al 119 physical activity at HA might be beneficial. In expedition, travelling, and HA exposure, there should be a strategy to avoid mood disorders, that might be due to altered neurochemical status, including neuro-encephalins, or altered blood-brain barrier.
Depressed individuals going to HA with a pre-existing psychiatric condition should be in a state of stable disease with no recent change in medication. There are, however, cases in which a latent depression might be revealed by isolation and HA. Such cases should have psychotherapy and encouraged to descend, especially because drug treatment at HA is poor, since most benzodiazepine are contraindicated at HA, similarly to alcohol use. The only tolerated hypnotic is Zolpidem 10 mg.
Another important notion is that there is an interaction between altitude and drug use. For instance, about one third of people with stroke have occult depression and several are on antidepressants, but a relative serotonin depletion due to hypoxia could be associated with resistance to standard antidepressants. Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressants, and this should be considered in post-stroke depressed patients.
Boos et al 120 in a Nepal trekking investigated the relationship between anxiety and AMS, this study involved 80 participants over 10 consecutive altitudes up to 5140 m during a trek. The majority of previous studies tended to be smaller and assessed only 1 or 2 altitudes. Furthermore, the subjects in this study 120 underwent an identical ascent protocol, staggered by 2 days. They included much higher altitudes than most studies done, which strengthened the relationship between anxiety and AMS given by the Lake Louise Score. HA anxiety symptoms may be difficult to be distinguished from AMS symptoms thus as suggested travelers should be advised about the symptom’s similarity between the two conditions. 119
Sleep alteration and its relationship with periodic breathing are altitude-related, the discussed hypocapnia suppresses ventilatory drive to the point of apnea. Carbon dioxide levels increase, stimulating respiration, which (with hypoxia) produces hyperventilation, and the cycle repeats, producing periodic breathing. Respiratory control involves both central and peripheral mechanisms.
Sleep architecture becomes progressively more disturbed and periodic breathing more frequent, while REM sleep is preserved. Both dreams and nightmares might, however, contribute to psychic homeostasis and be useful in stressing environments. Johnson et al 121 in a Nepal trekking observed increasing episodes of apnea/hypopnea (AHI) and higher arousal index (AI) from Kathmandu (1500 m) to Lobuche (5000 m).
Although not specifically studied in patients with obstructive sleep apnoea syndrome (OSAS) at HA, the addition of low flow (1-2 L/min) nocturnal oxygen is helpful in climbers and may be advantageous in patients with OSAS to reduce both periodic breathing and central apneas. Given the high prevalence of psychiatric condition in general population is not uncommon that such pre-morbidities may be present in climbers or travelers to HA. 119 We recommend maintaining current medication, avoid drugs interaction, alcohol, and hypnotic drugs assumption.
Cranial nerve palsies
Several cranial nerves palsy have been reported at HA due to different causes such as hypoxia induced brain swelling and increased intracranial pressure, barometric pressure changes, dehydration and possibly vasospasm or a hypercoagulable state, cold or infections. Beyond the well-recognized sixth cranial nerve palsies due to cerebral swelling at HA, in most of the reported cases due to other etiology a complete recovery has been reported after several weeks or months. Unusual cases of acute unilateral optic neuropathy secondary to barotrauma following a medial orbital wall fracture has been reported 122 as well as an anterior ischemic optic neuropathy in pilots 123 and secondary to decompression sickness. 124 , 125 Oculomotor nerve palsy (III cranial nerve) has been reported (3600 m). 126 Abducens nerve palsy was found at HA both isolated and correlated with HACE (in less than 1%) 21 , 22 and possible mechanism are HA increased intracranial pressure, brain edema, vascular lesions, or stress induce latent amblyopia. 40 , 127 , 128 Facial baroparesis (VII cranial nerve palsy), typically due to the increased pressure compressing the nerve in the middle ear cavity, has been reported in 11 published case report due to HA air travel or mountain trekking (4300 m reached in 6 days). 129 , 130 Hypoglossal nerve palsy probably due to increased pressure in the hypoglossal foramen has been reported (3500 m reached from 2500 in 3 days). 129
Neurodegenerative disorders
Multiple sclerosis.
Multiple sclerosis (MS) is an autoimmune disease and repetitive proinflammatory cascades could also act at the endothelial level causing decreased vasodilatory capacity reducing the neurovascular coupling during task execution. This cerebral vasoreactivity (CVR) impairment together with the hypoxia related damage occurring in acute inflammatory lesions, 131 suggests that patients with MS must be advised to avoid altitude to prevent a possible new relapse, even when symptoms are mild. The possible involvement of the autonomic nervous system in patients with MS may also be related with the lack of compensatory mechanism with the exposure to altitude. An exacerbation of a relapsing remitting MS was recently reported with acute exposure to HA (Mt. Fuji at 12388 feet/3776 m). 132 A high AMS occurrence (after 48 hours at altitude and symptoms lasting 2 days) has been reported in MS athletes at HA during the National Veterans Winter Sports Clinic in Snowmass, Colorado (2470-3813 m). 133 Another study has found that athletes with neurological impairments (including MS) with a prior history of AMS and headache at HA have a higher Lake Louise Score (LLS). 134 Nine MS patients participated to a 5-day expedition to Machu Picchu and most of them experienced altitude sickness >3600 m or more and were treated with analgesic if needed, they also reported transient sensory complaints and increased equilibrium disturbances but without evidence for any relapses. 135
Beyond hypobaric hypoxia (HH), other environmental stressors such as temperature (T) may affect negatively MS patients. MS patients may develop new neurological signs and symptoms if they present an infection or if exposed to cold (e.g., central pain exacerbations due to cold hypersensitivity). 136 A high prevalence and mortality rate of MS patients have been reported in US high-altitude states with average low temperatures (CO, WY, and MT). 137 The detrimental effect of elevated environmental heat has also been reported since long time. Indeed, in the past the diagnosis of MS was performed using a hot bath test which induce temporary symptoms (e.g., visual impairment, fatigue, motor disability or tingling) the so called “Uthoff’s phenomenon.” Therefore, MS patients are particularly sensitive to high outdoor temperatures and humidity which can raise the core T, and exercises-induced hyperthermia even after short-term exposures. However, the possible long-term adaption may improve thermoregulation of MS patients in the high-temperature and low-latitude region and explain the higher prevalence and mortality rate in colder and higher states reported. 137 Furthermore, a decreased risk of MS has been reported after exposure to ultraviolet radiation. 138
In conclusion, the exposure either acute or chronic to HA does not seem advisable and a personalized evaluation should be performed before the clinicians can advise properly patients with MS to whether or not they could go to HA.
Mild cognitive impairment and dementia
Mild cognitive impairment (MCI) is a condition in which individuals demonstrate minimal cognitive impairment of instrumental activities of daily living and it is considered to be an intermediate state between normal cognitive aging and early dementia. 139 However, the progression toward dementia may reverse as it has been showed in approximately 24% of the individuals in different longitudinal studies. 140 Several factors (e.g., lifestyle) have been implicated in MCI reversion. The possible contribution of hypoxia in the progression of the MCI into dementia is not yet established. Hypoxemia is a crucial factor for cognitive impairment in patients with pulmonary (e.g., COPD) 141 , 142 and cardiopulmonary disorders, 143 , 144 and the degree of cognitive impairments is closely related to the degree of hypoxia. In patients with cardiac arrest have been found that hypoxia increase β-amyloid (Aβ) level. 145 In an animal model has been found that chronic HA exposure induces learning and memory deficits and the reduced expression of several synaptic proteins and astroglial cell markers in different brain areas. 146 Recent studies suggest a potential beneficial role of limited exposure to hypoxia. Experimental intermittent hypoxia (IH)-hyperoxia training has demonstrated improvement in cognitive functions and decreased Alzheimer’s disease (AD) biomarker in MCI patients. 147
Well‐adapted elderly Andean HA dwellers compared to lowlanders showed a slightly impaired cognitive function. 148 - 150 Higher MCI prevalence was found in 1000 lowlanders staying at HA (>4300 m) for >12 months in India compared to 1000 lowlanders staying at sea level. 151 On the contrary, a cognitive screen performed in 481 HA (2100 m-4000 m asl) residents in developing regions (aged >60 years), 1.37% were classified as MCI whereas the 98.8% of the subjects scored within normal range. 152 The contradictory results may depend in the latter case on specific population characteristics (e.g., illiterate), but could also be related with the reduced environmental and cardiovascular risk factors in rural population. 152 Several studies have investigated the acute and chronic effect of HA exposure on cognition in healthy subjects, and it is still not clear whether there is a selective or a general impairment of tasks investigating both central executive (working memory set-shifting, updating, monitoring, inhibition, and planning) and non-executive (perception, attention, and short term memory) functions. 153 - 155 Two cases of secondary subcortical dementia with neuropsychiatric symptoms, due to lesion in the globus pallidus bilaterally, following HACE at HA (3500 m) have been reported. 24 Due to the potential deleterious effect exerts by hypoxia on cognitive functions it is not advisable to allow patients with any type of dementia to go to altitude and this could be applied also to MCI patients. Moreover, the use of dexamethasone in case of HAI can reduce the effect of anticholinergic and cholinesterase inhibitors drugs therefore worsening the cognitive symptomology.
Parkinson’s disease
PD is related to the neurodegeneration of the nigrostriatal dopamine system that lead to a decrease dopaminergic transmission in the basal ganglia (BG). BG are particularly susceptible to hypoxia-ischemia due to their high metabolic activity. 156 There is evidence that OSAS due to chronic intermittent hypoxia contributes to the pathogenesis of PD increasing the alfa-synuclein levels. 157 Severe and prolonged hypoxia contributes to brain damage, but moderate hypoxia exerts a neuroprotective effect through HIF-1alfa activation in PD model 158 while low level of HIF-1alfa is associated with neuronal dopaminergic cell loss in the substantia nigra pars compacta (SNpc) and contributes to PD pathogenesis. 159 HIF1alfa pathway is proposed as a therapeutic target for PD. 160
The possible involvement of the autonomic nervous system in patients with PD may lead to the lack of compensatory mechanism with the exposure to altitude. In PD patients has been reported an impaired chemosensitivity to hypoxia and perception of dyspnoea. 161 Dyspnea is frequently reported by 40% of PD patients, 162 enough to deserve to be included in the clinical evaluation screening thorough the nonmotor symptoms scale (NMS) and in the evaluation of their impact on daily life part I of the Movement Disorder Society—Unified PD Rating Scale (MDS-UPDRS) as it has been suggested. 163 One case of Parkinsonism after acute HH exposure (up to 16000 ft-4876.8 m) resulting in damage of the basal ganglia has been reported. 164 However, there are no published data in the literature regarding patients with idiopathic PD traveling to altitude. Few studies were performed to evaluate the effects of mountain exercise in PD’s patients and demonstrate improvement in motor performance and social cognition; however, it is not specified at which altitude they stayed. 165 , 166
Screening for OSAS or dyspnea should be included in the evaluation of PD patients willing to travel to HA location and if positive they should travel with non-invasive ventilatory support. Due to the fluctuation of nonmotor symptoms (e.g., dyspnea) and motor symptoms in advanced PD patients, mainly related to the response to the dopaminergic medications, every patient should have specific oral antiparkinsonian drugs promptly available, should always visit the mountain accompanied and maintain adequate hydration. In conclusion, a careful personalized evaluation should be made by a neurologist expert in the field considering other risk factors such as prior history of any HAI.
Neurological symptoms presenting at HA may be related to HAI and usually ameliorate or resolve to a certain extent upon descent, whereas the persistence of them suggests the presence of intracranial lesions.
Three cases were reported of brain tumors both malignant and benign which suddenly become symptomatic when people are exposed to HA (range between 3000 and 4000 m). 167 , 168 A similar problem is presented by arachnoidal cysts and pinealomas. 167 This might be due to edema, an increase in cerebral blood flow, or increased cerebrospinal fluid pressure. Patients with brain tumor (e.g., colloid cyst) may have obstructive hydrocephalus which can worsen with the pressure changes due to HA. These events are usually well-tolerated in healthy individuals but may lead to severe consequences in patients with brain lesions, given the lack of brain reserve. Following craniotomy have been documented residual trapped air that expand at HA 169 and cause raised ICP leading to severe neurological symptoms depending on the underlying cause. 170 Patients with known intracranial lesions are unstable and should not travel to HA.
Brain trauma and other lesions
HA exposure slow the brain repair resulting from a concussion. 171 Management of brain trauma aimed to prevent a further or secondary brain insult minimizing the occurrence of hypotension and hypoxia. 172 In addition, hypobaria exerts a negative effect on intracranial pressure and cerebral perfusion pressure. There are evidence suggesting an increased blood-brain barrier permeability enhancing action of free radicals is also possible. In highlanders, residents mortality and nerve function recovery after a traumatic brain injury and decompressive craniotomy were affected by the elevated hemoglobin concentration due the chronic HA exposure. 173
For a patient with a traumatic or metabolic brain injury, such as CO poisoning, severe previous COVID-19 infection, previous brain hypoxia or after a cardiovascular operation 84 it does not seem advisable to go at high altitude.
Peripheral nerve disorders and neuromuscular disease
Diabetic neuropathy is frequent while other condition affecting peripheral nerves or neuromuscular disorders are unfrequent. Inherited or acquired sensory motor peripheral neuropathies reduce the sensibility of the foot, during walking or climbing causing risks. Beside hyperglycemic episodes in diabetic neuropathy there are in addition microvascular abnormality, segmental demyelination and remyelination. This angiopathy is further aggravated by the exposure to hypoxia, therefore microtraumatic events and/or cold exposure could aggravate these angiopathy and induce nerve demyelination or axonal atrophy. Neuropathic patients should be advised to wear comfortable shoes, accounting for the individuals’ feet shape and possible deformities, but also for the feet sizes’ variability due to prolonged standing position, to avoid further reduced blood flow to the extremities.
The present recommendations are that hydration should be maintained, immobility should be avoided or flight socks when flying encouraged to prevent deep venous thrombosis and wearing warm comfortable stockings during mountaineering activities. There is no evidence that previous peripheral damage can progress at altitude. Paulson et al 174 found that Charcot Marie Tooth patients were at risk of developing dysarthria, incoordination and difficulty walking after returning from skiing at 8000 ft in the Colorado mountains.
Neuromuscular disorders such as muscular dystrophies, myotonic dystrophy, and amyotrophic lateral sclerosis, can facilitate alveolar hypoventilation provoking hypoxemia and sleep disturbances, including sleep apnea, with nocturnal hypoxemia to an oxygen saturations level as low as 75% at sea level. At altitude these patients can have higher desaturations risks. Therefore, patients with neuromuscular disorders should be screened for the presence of sleep apnea prior to travel to HA and, if sleep disturbance is detected, they should travel with non-invasive ventilatory support. 175 Patients with neuromuscular disorders with a decrease of forced vital capacity (FVC) of >60% should not travel at medium/high altitude.
Further research and insight for muscle mass loss and the understanding of the muscle protein pathways could further provide recovery for HH effect. Ruggiero et al 176 showed that acute exposure to severe hypoxia exacerbates peripheral fatigue and muscle slowing compared with sea level, that only appropriate acclimatization to HA reversed the effects of acute hypoxia, at least in those not on medication.
Cramps might be a sign of muscle fatigue but also a sign of occult or known peripheral neuropathy.
Myoglobinuria might be due to poor hydration or electrolyte unbalance.
Rhabdomyolysis is a definite risk for travelers due to unaccustomed physical exercise, other factors contributing to the risk of myoglobinuria are beside inadequate preventive hydration, high ambient temperatures, supplement use (e.g., creatinine and herbal weight loss supplements), or certain medications (e.g., statins, selective serotonin reuptake inhibitors), illicit drug or alcohol use, or recent viral illnesses. The first step when encountering rhabdomyolysis after strenuous exercise is to determine whether the rhabdomyolysis is clinically significant, requiring descent or intravenous fluid administration. Since corticosteroids might transitory increase glycemia and cause hypokalemia caution should be paid in treating acute HA illnesses (e.g., HACE, HAPE) to avoid in diabetic travelers the ketoacidosis. Since also acetazolamide can induce ketoacidosis, it should never be used in diabetic patients. Caution should be exert with the use of both corticosteroids and calcio-antagonists due to their metabolic and vasoactive effect. GABAergic medication used for neuropathic pain should be reduced to avoid drugs interaction in case of emergency drug treatments.
Epilepsy/seizure at high-altitude
Seizures at HA may occur in the setting of AMS or HACE, 177 but can be also elicited by the HA exposure in persons with previous history of fits without current therapy 178 or in those in treatment with antiepileptic drugs. 179 Two case were reported in male trekkers in Nepal that had a single generalized grand mal seizure without any structural (CT) or functional (EEG) abnormalities, ruled out in Kathmandu. 180 Similarly, Hennis et al 181 reported a case of a young male with a family history of seizures, who experienced an isolated tonic-clonic seizure whilst hypoxemic at 4250 m. Since in all these three cases the mountaineers were acclimatized it is unlikely that the seizures could be related to AMS or HACE. Neuronal excitability could be increased by several physiological events such as shortage of sleep, exhaustion, dehydration, electrolyte disturbances such as hypocalcemia or hyponatremia. In addition, acute severe hypoxia and respiratory alkalosis at HA may provoke epileptic seizure. De novo seizures in people at altitude are anecdotal but may be fatal. 178 Observation on seizures at altitude are: 1. they tend to be first time fits; 2. they occur in the first 2-3 days after arrival; 3. there is an under representation of alcohol abuse; 4. fits seem to be more thalamic than cortical in origin. 41 For a single seizure occurring at altitude if any possible underlying neurological condition is ruled out there is no contraindication for future mountaineering, trekking or climbing with specific precautions as suggested by the UIAA Medical Commission and other authors. 182 For known epileptics it is advisable to continue previous antiepileptic therapy at altitude, 179 and if they discarded therapy, one should consider resuming medicines. Moreover, it is advisable avoid sleep deprivation and alcohol use/abuse, and also epileptogenic drugs.
Conclusive remarks
Mountain climbers may develop specific illnesses that largely depend on the altitude reached and the rate of ascent. The popularity of travel to HA destinations, extreme tourist activities and mountain climbing is reflected by the fact that neurologists at low altitude are increasingly likely to encounter neurological problems and disorders in people exposed to HA. Additionally, neurologists may have to advise patients with pre-existing neurological conditions on the risks of ascent to altitude. This review focuses on neurological-related HAI: AMS and HACE, as well as other neurological disorders occurring at HA and the risks posed by HA for patients with neurological disorders.
The present study examines the problems posed by HA traveling with several neurological conditions, and whether the underlying disease will worsen in the mountains (see also Table 2 ). The neurological conditions that allow to practice mountaineering include migraine, except with atypical aura, and other common headaches, epileptic seizures under good pharmacological control and Parkinson’s disease without OSAS with precautions. All neurological patients need to attend altitude locations always accompanied. Contraindications are unstable neurological conditions (e.g., recent stroke), diabetic neuropathy, neuromuscular disorders with a decrease FVC of >60%, Parkinson disease with OSAS, MCI and dementia, cerebral thrombosis, intracranial hemorrhage and vascular malformations, and intracranial space occupying mass.
Adaptive and maladaptive altitude responses and neurological consequences.
CBF: cerebral blood flow; MS: multiple sclerosis; PD: Parkinson’s disease; PFO: patent foramen ovale; PNS: peripheral nervous system; PRES: Posterior reversible encephalopathy syndrome; RCVS: Reversible cerebral vasoconstriction syndrome; TGA: Transient global amnesia.
We try to estimate the risk found by previous transient ischemia of the brain, emboli from patent foramen ovale, occlusive cerebral artery diseases, multiple sclerosis, peripheral neuropathies, neuromuscular disorders, as well as psychiatric and sleep disorders.
We provide recommendations regarding evaluation, advice for or against travelling in mountains and effective prophylactic measures since individual cases should be advised after careful examination and risk evaluation either in an outpatient mountain medicine service or by a physician with knowledge of risk involved in travelling in the mountains ( Table 3 ).
Recommendations for HA exposure for neurological patients.
a personalized decision has to be made after careful evaluation by a neurologist expert in the field.
AMS: acute mountain sickness; FVC: forced vital capacity; OSAS: obstructive sleep apnea syndrome; PFO: patent foramen ovale; TIA: transient ischemic attack.
This area has not been fully investigated and the data are in many instances either anecdotal or based on personal experience therefore further experience is needed. The main purpose of these recommendations is to avoid occurrence of acute mountain sickness or cerebral edema and recurrence of a neurological condition in a remote area where the rescue might be difficult.
Author Contributions: All the authors contributed to this review article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Marika Falla https://orcid.org/0000-0001-7477-3020
Corrado Angelini https://orcid.org/0000-0002-9554-8794
Advertisement
The Dali was just starting a 27-day voyage.
The ship had spent two days in Baltimore’s port before setting off.
- Share full article

By Claire Moses and Jenny Gross
- Published March 26, 2024 Updated March 27, 2024, 9:07 a.m. ET
The Dali was less than 30 minutes into its planned 27-day journey when the ship ran into the Francis Scott Key Bridge on Tuesday.
The ship, which was sailing under the Singaporean flag, was on its way to Sri Lanka and was supposed to arrive there on April 22, according to VesselFinder, a ship tracking website.
The Dali, which is nearly 1,000 feet long, left the Baltimore port around 1 a.m. Eastern on Tuesday. The ship had two pilots onboard, according to a statement by its owners, Grace Ocean Investment. There were 22 crew members on board, the Maritime & Port Authority of Singapore said in a statement. There were no reports of any injuries, Grace Ocean said.
Before heading off on its voyage, the Dali had returned to the United States from Panama on March 19, harboring in New York. It then arrived on Saturday in Baltimore, where it spent two days in the port.
Maersk, the shipping giant, said in a statement on Tuesday that it had chartered the vessel, which was carrying Maersk cargo. No Maersk crew and personnel were onboard, the statement said, adding that the company was monitoring the investigations being carried out by the authorities and by Synergy Group, the company that was operating the vessel.
“We are horrified by what has happened in Baltimore, and our thoughts are with all of those affected,” the Maersk statement said.
The Dali was built in 2015 by the South Korea-based Hyundai Heavy Industries. The following year, the ship was involved in a minor incident when it hit a stone wall at the port of Antwerp . The Dali sustained damage at the time, but no one was injured.
Claire Moses is a reporter for the Express desk in London. More about Claire Moses
Jenny Gross is a reporter for The Times in London covering breaking news and other topics. More about Jenny Gross

IMAGES
VIDEO
COMMENTS
The current observational study is the first to investigate prospectively a possible association between travel history and stroke in a large series of patients. For the association between travel history and stroke, the term "economy class stroke syndrome" has been introduced in the literature. Until now, 14 single cases of ECSS have been ...
As it turns out, a history of stroke does not pose danger to the brain during an airline flight, and therefore, a past stroke is not a contraindication to flying on an airplane as a passenger. A transient ischemic attack (TIA) is a mini-stroke that resolves without permanent brain damage. A TIA is very similar to a stroke and it is a warning of ...
Risks of flying after a stroke. Flying may increase the risk of a blood clot in the arm or leg if people are immobile for long periods, such as during long-distance flights, which are usually ...
There is no shortage of books, chapters and papers on the history of stroke focusing predominantly on the last 150 years and enumerating endless "milestones". Instead of adding another article to this body of knowledge, this essay aims at ensuring awareness for the "big picture", the "grandes routes", and the "striking breakes" without overloading the reader with too much detail.
The Stroke Association recommends that it is "probably best to avoid flying for the first two weeks. This is the time when your problems are likely to be most severe and other conditions related to your stroke may come up.". In the most severe stroke cases, patients may want to wait as long as three months. However, with a TIA, many people ...
This helps to give you a bit more room. Use a carry-on. Use a shoulder bag or back pack. Pack it with basic toiletries, medications, and travel information. Wear shoes that are easy to take on and off. This makes security checks easier. Travel with someone. It helps to travel with someone who can help you.
If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a large vein may also increase your risk of blood clots. Getting up and walking around when possible is recommended for long flights, just be sure the seatbelt light is not on when you do so.
Travel precautions help people with heart disease. Traveling to a faraway place doesn't need to be off limits because you have heart disease or are a caretaker of someone who has had a cardiac event like heart attack or stroke. A few simple precautions can help make your trip smooth. Here are some travel tips:
Ideas for the Airport (2:19-5:05) Being prepared before you are inside the airport can help reduce stress and save time. Checking luggage, using an easy to carry bag, and having a direct flight are some helpful tips. Airports have resources and services if you have mobility impairments.
Stroke research in the future. With increased collaboration, identification of the need for rigorous experimental design and closer interactions between clinical and preclinical researchers, there is a fresh wave of optimism in the stroke field that new and improved treatments will be found to benefit patients.
Timing. First off, it is crucial to avoid flying within the first couple weeks of having a stroke. This span can reveal some of the strongest signs of mental and physical impairment, so giving a survivor time to adjust is important. In any situation, make sure to consult with a doctor before making travel plans.
Or they can be caused by blood clots or other debris that travel through the bloodstream, most often from the heart. An ischemic stroke occurs when fatty deposits, blood clots or other debris become lodged in the blood vessels in the brain. ... Personal or family history of stroke, heart attack or transient ischemic attack. COVID-19 infection ...
5. Make Frequent Pit Stops. When traveling by car during high traffic times, such as Thanksgiving or Christmas week, take a route with rest stops, such as a major highway, and plan for breaks at ...
According to the Stroke Association, it is best to wait at least two weeks to fly following a stroke. This is because a person is at an increased risk of a second stroke after suffering a TIA (transient ischemic attack) or stroke. In the event of a second stroke, it is advisable to be close to emergency medical interventions that can reverse ...
Introduction. Stroke accounts for 2% of all medical emergencies during commercial flights with an estimated incidence of 1 stroke every 163 420 flights. 1 On-board stroke has been reported in several scientific studies, although most were retrospective case series focusing on economy class stroke syndrome (ECSS). 2, 3 This subtype of stroke ...
Comparison with non-passenger controls was used to identify clinical features of stroke in passengers against a group who had no history of air travel during the previous 2 years (1st of Jan 2018-1st of March 2020). A comparison of stroke risk factors, severity of stroke, discharge status and clinical outcomes in the two groups was performed.
The mostly unwritten history of stroke in the twentieth century should not only include the medical, but also the patient's and the societal perspective. ... But it may also be linked to the high rate of post-stroke disabilities hindering victims to travel to a place of pilgrimage. On the other hand, there was definitely a lack of commercial ...
Stroke affects a wide variety of patients but particularly older people. It can be very challenging to get a coherent history. By definition stroke is sudden onset—one moment a person is well and the next they are not, and so acute stroke patients are often frightened. Patients may be drowsy, disorientated, frightened, dysphasic or even ...
Healthy Travel. Whether you're traveling on vacation or for work, it's important to stay healthy and active. When you're away from home and your regular routine, it takes a bit of planning. Traveling can be tough on healthy habits. Unfortunately, there's no quick recovery from a week of lounging by the pool or having drinks out with ...
The bridge is an important travel route with a deep history. Enlarge this image. ... Cargo already at the Port of Baltimore will have to travel overland, but truck traffic will also be snarled by ...
Ten months ago, my parents paid £4,000 for a holiday with Princess Cruises through the travel agent cruise118.com. Last month, three weeks before departure, my mum suffered a stroke.
Long-term depressive status may be established by 5-years post-onset. Early- and late-onset depression presented similar natural history, while severe depression had a longer duration and quicker recurrence than mild depression. These estimates were limited to alive patients completing the depression assessment, who tended to have less severe stroke than excluded patients, so may be ...
Southwest Airlines is preparing to launch overnight flights for the first time in its history. After hinting at the change last year, the Dallas-based carrier plans to add overnight flights from ...
The history is an important part of the code stroke assessment. Based on the history gathered, you will have a low or high pretest probability for a stroke prior to the CT scan. Remember the six important questions to ask, specifically the time last seen normal, as it starts the clock on potential acute stroke therapy.
Neuroinflammation immediately follows the onset of ischemic stroke in the middle cerebral artery. During this process, microglial cells are activated in and recruited to the penumbra. Microglial cells can be activated into two different phenotypes: M1, which can worsen brain injury; or M2, which can aid in long-term recovery. In this study, we contribute a summary of experimental data on ...
Francis Scott Key Bridge has a deep history According to the MDTA, the bridge crosses over the Patapsco River, near where Francis Scott Key, the bridge's namesake, was inspired to write the lyrics ...
Francis Scott Key was believed to be near the site when he observed a British bombardment during the War of 1812. By Jin Yu Young The Francis Scott Key Bridge, which collapsed after being struck ...
Riccardo died in 1954 and Redmond and the Malnatis moved on to rival pizzerias, Gino's East and Lou Malnati's. Sewell, by this point the sole owner, changed the name to Pizzeria Uno.
Conclusions. Our recommendations suggest absolute contraindications to HA exposure for the following neurological conditions: (1) Unstable conditions-such as recent strokes, (2) Diabetic neuropathy, (3) Transient ischemic attack in the last month, (4) Brain tumors, and 5. Neuromuscular disorders with a decrease of forced vital capacity >60%.
The ship had spent two days in Baltimore's port before setting off. By Claire Moses and Jenny Gross The Dali was less than 30 minutes into its planned 27-day journey when the ship ran into the ...