How sperm meets egg: a journey from production to fertilization
Many wonder what the sperm ´s journey is like from ejaculation to fertilization. The ultimate goal of a sperm is to fertilize the egg cell.
However, the journey of the sperm to get to the egg is not an easy one. To reach the egg cell, the sperm has to go through a long and difficult journey that can take from thirty minutes to several hours .
For this reason, fertilization needs a large number of motile spermatozoa for at least one of them to be able to overcome all barriers. Firstly for the sperm to get to the egg, and then to fertilize the egg.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1. How the sperm meets the egg
- 2. Route from the testicle to the urethra
- 2.1. Changes in the sperm
- 3. The journey through the female reproductive system
- 3.1. What barriers do spermatozoa have to cross?
- 3.2. The sperm´s arrival at the Fallopian tubes.
- 3.3. Final stage of the spermatozoon: acrosome reaction
- 4. FAQs from users
- 4.1. How long does it take from sperm production to ejaculation?
- 4.2. How can ovulation be calculated so that the sperm and egg meet?
- 4.3. How long can a sperm live in the female reproductive tract?
- 4.4. How many sperm make it to the egg?
- 4.5. How long does it take sperm to reach the egg?
- 4.6. After sperm meets egg, how long until implantation?
- 4.7. Where do the sperm cells pass through on their way to the egg?
- 4.8. Where does the sperm need to get to, to be able to fertilize the egg?
- 5. Recommended reading
- 6. References
- 7. Authors and contributors

How the sperm meets the egg
Colloquially,the path to fertilization we understand as a race in which only the best sperm will be able to reach the finish line and win the prize. Effectively, it is something like this: many spermatozoa start the race, but only one will fertilize the egg.
The route of the sperm to the egg can be divided into two major stages:
- Male reproductive system: the journey of sperm in the male body is from the testicles to the outside world.
- Female reproductive system: from the vagina, where semen is deposited, to the Fallopian tubes, where the egg is found.
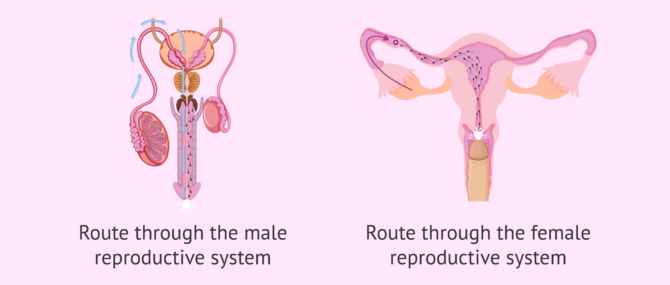
It should not be forgotten that during these two phases of the journey the sperm meet certain obstacles. To follow, we discuss what they are.
Route from the testicle to the urethra
It takes about 90 days for spermatozoa to develop and acquire the necessary maturation before they can be expelled in an ejaculation.The birth of spermatozoa takes place in the seminiferous tubules of the testes. They subsequently pass to the epididymis.
The seminiferous tubules are the internal structures of the testicle where sperm are made. The epididymis is a long structure that connects the testicle and the vas deferens.
At the moment of intercourse, a large quantity of sperm (about 250 million) leave the epididymis and pass through the vas deferens and the urethra. Along the way, the sperm are bathed in fluids released from the seminal vesicles and the prostate. In this way, the semen, the mix of sperm and fluids, is formed.
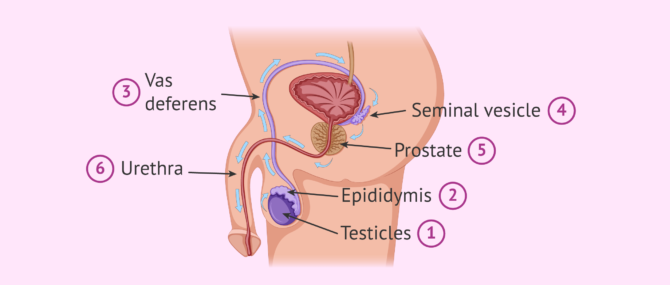
The main function of these seminal fluids is to make is possible for the sperm to enter into the vagina. Sperm will shoot out of the urethra through the penis until they enter the female reproductive tract , specifically the vagina.
Changes in the sperm
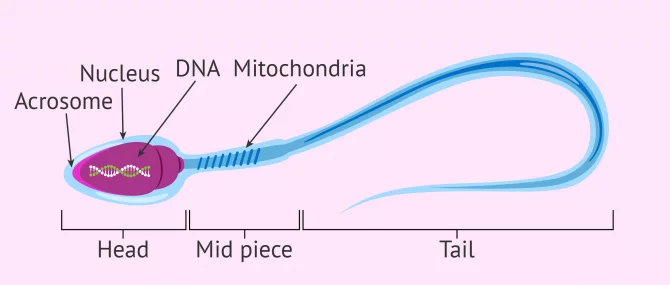
During this journey from the testicle to the outside, the sperm acquire the correct shape and structure to allow fertilization of the egg. The changes that occur at this final stage of sperm maturation are:
- DNA compaction to allow the head (where the DNA is stored) to be as small as possible and therefore move better. This also helps it to pass through the zona pellucida (egg shell).
- The tail acquires the perfect design so the sperm have great speed and resistance.
- The middle piece has a large number of mitochondria for high energy production. This gives the spermatozoon great efficiency in energy usage.
If you wish to continue reading information about what the spermatozoon cell is like, we suggest you visit this article: How are spermatazoa formed
The journey through the female reproductive system
In the process of ejaculation, sperm cells leave the man and enter the vagina. This is where the sperm cells begin the second part of their journey to fertilization.
During this second part of the journey the sperm again encounter an large number of obstacles. These obstacles and barriers can hinder the sperms arrival at the Fallopian tubes, where the egg is waiting.
There is a distance of between 15 and 18 cm and time is of the essence. Sperm cannot afford to delay, since the egg, once it has left the ovary (i.e., after ovulation ), has a half-life of about 24 hours. The survival time of the egg is short compared to that of the sperm. Sperm can live between 2 and 5 days in the female reproductive tract.

After ejaculation, the race of the sperm cells begins. It is a race not only of speed but also of endurance . Defective sperm and/or those with poor motility will fall by the wayside.
What barriers do spermatozoa have to cross?
Some obstacles, or barriers, encountered by sperm are as follows:
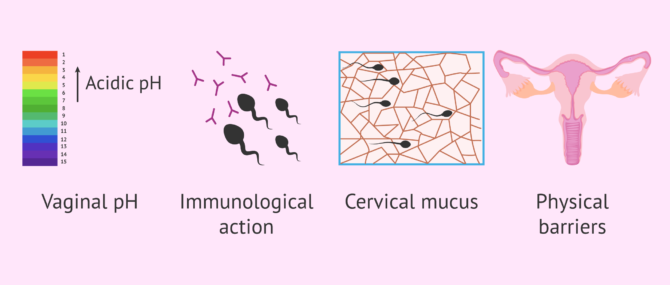
However, it is not all difficulties in the journey of the sperm. The egg tries to pave the way for the sperm by releasing molecules and sending signals. The fallopian tubes and uterus exert a suction force through rhythmic contractions and the cervical mucus becomes less dense allowing the sperm to swim better.
For its part, the seminal fluid that accompanies the sperm neutralizes the pH and provides sugars to the sperm. This fluid also serves as a protective shield against the woman´s white blood cells.
The sperm´s arrival at the Fallopian tubes.
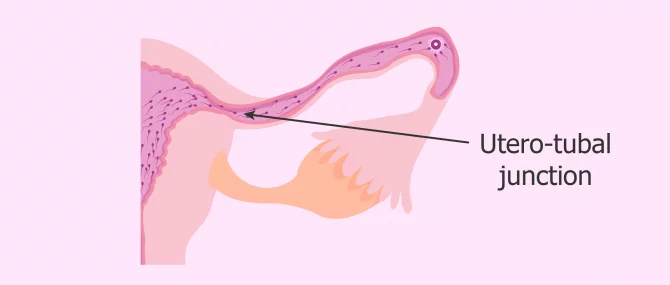
Once the vaginal, cervical and uterine barriers have been overcome, we encounter the narrowest part of the course: the uterotubal junction . Only a few thousand of the average 250 million spermatozoa in freshly ejaculated semen reach this point.
Along the way, the strongest spermatozoa, i.e. those that have been able to overcome the female obstacles, acquire an extraordinary ability: the ability to fertilize . This is known as sperm hyperactivation . From this moment on, its tail moves with much more force and energy, allowing a vigorous movement that helps it arrive at the egg.
Once they reach the fallopian tubes, many sperm remain attached to the tube walls, exhausted and unable to continue their journey.
At this point, few sperm are left in the race, as the vast majority have been lost along the way. Of the few dozen sperm that remain before the egg's watchful eye, only one will make it through the thick doorway to the egg: the zona pellucida.
The chosen sperm, the strongest and most capable one, upon contact with the zona pellucida, initiates the so-called acrosome reaction .
Final stage of the spermatozoon: acrosome reaction
As mentioned above, when the most able sperm has reached the egg, the acrosome reaction takes place. This is the release of the contents of the acrosome, which is composed of a series of enzymes. The purpose of this enzymatic release is to weaken the zona pellucida of the ovum and facilitate penetration.
The acrosome is a structure located in the head of the sperm. It serves as a reservoir for enzymes and other substances that the sperm needs to pass through the zona pellucida.
This reaction "wakes up" the egg, which releases cortical granules , organelles that prevent any other sperm from penetrating. It is as if the ovum plants a flag indicating to the rest of the spermatozoa around it that it has already been conquered by the winning spermatozoa and, therefore, that the doors of its kingdom are closed.
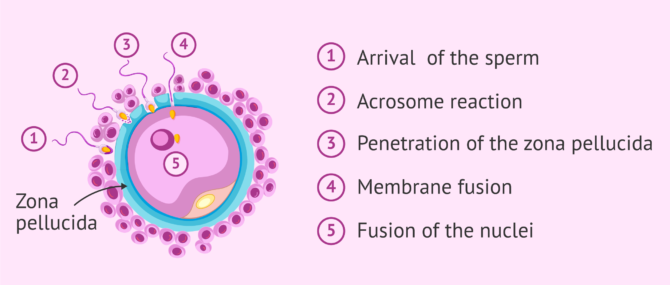
Once the sperm penetrates the oocyte, their two nuclei fuse. This is what we know as fertilization . If you want to know the details about how the sperm enters the egg and how the new being is formed, you can read this article: The steps of fertilization in humans.
We're already 773!
Join our inviTRA community
FAQs from users
How long does it take from sperm production to ejaculation.
Spermatogenesis is the process whereby male reproductive cells are formed, from the immature ones, spermatogonia, until the mature ones, spermatozoa. This complicated process occurs within the seminiferous tubule in the testis and takes about 64-72 days.
Once spermatozoa (sperm cells) have been produced, they leave the testis and travel to the epididymis, where they will acquire the necessary motility in a process that lasts 10 days approximately. Spermatozoa will be stored in the epididymis until they are expelled with ejaculation. When ejaculation starts, sperm travel through the vas deferends and mixes with the seminal fluid that originates in the secretory glands, creating what we all know as semen . Finally, it is expelled through the urethra.
How can ovulation be calculated so that the sperm and egg meet?
It can be calculated by measuring the daily basal temperature and by performing a urine LH test.
How long can a sperm live in the female reproductive tract?
Once ejaculation occurs and the sperm are released into the vagina, they have a half-life of 2 to 5 days. The stronger ones will survive longer. The weaker ones will die on the way. After fertilization, the dead spermatozoa and the live ones that have remained unable to fertilize the egg will be eliminated by phagocytosis (the body's own system of neutralization and elimination of substances).
How many sperm make it to the egg?
To answer this question, we will split the answer into various figures, each one corresponding to a stage in the journey:
- There are approximately 200-250 million sperm in each ejaculation, but only about 2 million make it to the cervix.
- Once there, out of the 2 million sperm entering the cervix, only about 1 million are able to make it to the uterus.
- Out of the 1 million that enter the uterus, only 10,000 are able to travel to the top of this organ.
- Out of the 10,000 that survive at this point, only half of them travel in the right direction, that is, toward the egg cell.
- Out of the approximately 5,000 sperm that enter the utero-tubal junction, about 1,000 get inside the Fallopian tube.
- Finally, out of the 1,000 that enter the tube, it is estimated that only 200 make it to the egg.
However, in the end, only 1 sperm out of the 200 that reach the egg is able to penetrate and fertilize it.
How long does it take sperm to reach the egg?
There is no set time, since the spermatozoa with the best quality, that is, with great ability to overcome obstacles and great strength of movement, will be able to reach the egg in just half an hour. However, there will be others that will need about two days to cross the entire female reproductive tract.
After sperm meets egg, how long until implantation?
Implantation occurs approximately within 3-7 days after fertilization, as the fertilized egg cell has to travel from the point where it was fertilized to the point where it implants. It depends on how high the point where they meet in the Fallopian tube is. For instance, if they meet high in the tube, it will take about 7 days.
Related stories: What Are the First Signs & Symptoms of Embryo Implantation?
Where do the sperm cells pass through on their way to the egg?
As mentioned above, they must first pass through the male reproductive tract and then, after ejaculation, through the female reproductive tract. In the first part of the journey, they leave the testicle and pass through the epididymis, the vas deferens and the urethra. During this part, they are impregnated with secretions from the prostate and seminal vesicle.
In the second part of the course, the spermatozoa pass from the vagina, where they are deposited, to the cervix. Subsequently, they pass through the uterus and reach the fallopian tubes, where the egg is found or where they wait for it to arrive, in case ovulation has not yet occurred.
Where does the sperm need to get to, to be able to fertilize the egg?
The sperm has to reach the fallopian tubes, where the egg is waiting. Once there, it will be able to fuse with it and give rise to the embryo. Subsequently, the embryo will leave the fallopian tubes, reach the uterus and implant in the endometrium of the uterine cavity. This is the beginning of pregnancy.
Recommended reading
The final goal of this whole journey of the sperm is to meet the egg, fuse with it and allow the birth of a new cell. This cell, after about nine months of successive divisions and processes of differentiation and specialization, will give rise to the future baby.
If you want to know more information about what happens after fertilization, we recommend reading this article: Pregnancy stages month by month
If you are interested in knowing more about the hormones responsible for sperm formation, you can visit this link: Male hormone check .
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
Austin CR. Observations on the penetration of the sperm in the mammalian egg. Aust J Sci Res B. 1951;4(4):581–596.
Bennett M. Shapiro. The existential decision of a sperm, Cell 49, no. 3 (May 1987): 293-94, esp. 293.
Chang MC. Fertilizing capacity of spermatozoa deposited into the fallopian tubes. Nature. 1951;168(4277):697–698 ( View )
Choza J. (1991): Antropología de la Sexualidad. Ed. Rialp. Madrid, 1.ª Edición ( View )
J Clin Invest. (2010). Fertilization: a sperm’s journey to and interaction with the oocyte. Research Institute for Microbial Diseases, Osaka University, Osaka, Japan. School of Biological and Biomedical Sciences, Durham University, United Kingdom. 120(4) 984–994 ( View )
Lennart Nilsson, A portrait of the sperm. In: The functional anatomy of the spermatozoan, ed. Bjorn A. Afzelius (New York: Pergamon, 1975), 79-82.
Martin E. The egg and the sperm: how science has constructed a romance-based on stereotypical male-female roles. “Signs”. Vol. 16. No. 3 (Spring, 1991), pp. 485-501. Published by: The University of Chicago Press ( View )
Stein KK, Primakoff P, Myles D. Sperm-egg fusion: events at the plasma membrane. J Cell Sci. 2004; 117(Pt 26):6269–6274 ( View )
Paul M. Wassarman, The biology and chemistry of fertilization, Science 235, No. 4788 (January 30, 1987): 553-60, esp. 554 ( View )
Paul M. Wassarman, Fertilization in mammals, Scientific American 259, no. 6 (December 1988): 78-84, esp. 78, 84
FAQs from users: 'How long does it take from sperm production to ejaculation?' , 'How can ovulation be calculated so that the sperm and egg meet?' , 'How long can a sperm live in the female reproductive tract?' , 'How many sperm make it to the egg?' , 'How long does it take sperm to reach the egg?' , 'After sperm meets egg, how long until implantation?' , 'How does it feel when sperm meets the egg?' , 'How long after IUI does sperm meet egg?' , 'Can sperm meet egg before ovulation?' , 'Where do the sperm cells pass through on their way to the egg?' , 'Where does the sperm go when you have a vasectomy?' , 'Where does the sperm need to get to, to be able to fertilize the egg?' , 'When pregnant, where does sperm go?' , 'When does sperm die outside the body?' , 'When does sperm leave the female body?' and 'How many sperm fertilize an egg for identical twins?' .
Authors and contributors

Find the latest news on assisted reproduction in our channels.
And when do men expel the so-called pre-ejaculatory fluid? I want to know it because then my boyfriend and I will be able to use the pull-out method more accurately. Thnxs!
Hello Katie1,
Firstly, the pull-out method, coitus interruptus , or withdrawal method is not a safe birth control method because it does not prevent you from the transmission of STDs (sexually transmitted diseases) and HIV infection (AIDs). Besides, it is actually an extremely unreliable method.
Apart from that, there are several theories about why pre-ejaculatory fluid exists, none of them proved. While some say the only function of this fluid is providing some lubrication for intercourse, others believe they protect the sperm by acting as a sort of pre-clearing of the urethra, making the environment more conductive for sperm to survive the journey and lowering the acidity. On the other hand, the function of sperm is reproduction.
I hope I have clarified your concerns,
My husband has had a vasectomy and we want to try for a baby. Is there any way we can do this without surgery?
It is possible for a man to become a father after again after a vasectomy. However, this is not possible without some kind of surgical treatment. There are different options available and you can find lots more information in our article: Pregnancy after vasectomy
I hope this helps and good luck.
Interesting article, thanks. It is very interesting that so many sperm are needed to fertilize just one egg and reading this makes me realize why!
Leave a Reply
Privacy Overview
Request A Callback
Sperm, Meet Egg: The Process of Fertilisation

Turbo-charged sperm speed through a dimly lit canal, coursing feverishly through vast landscapes and titanic cavities. A lone egg desperately awaits her suitor, pledging her life if left unavowed. Then, the swiftest sperm rises from the depths of darkness, breaking through a fortress wall and presenting himself to his prospective partner. A union is formed. The end. This is the stuff of movies and drama. But it’s also the stuff of fertilisation. When sperm are released into the vaginal canal, an intricate performance ensues. With the ovaries serving as arc lights, the stage womb is set.
Understanding Fertilisation
Every month, one amongst a woman’s two ovaries releases a mature egg into the fallopian tube. This egg remains available for fertilisation for about 24 hours, and if met by a sperm, can lead to conception . Sperm can survive for up to 5 days within the uterine cavity, so it is possible that you will get pregnant if you’ve had intercourse in the 5 days leading up to ovulation .
It’s wise to maintain an ovulation calendar to preempt your fertile periods. Conception involves millions of sperm vying to outpace each other in order to reach the available egg. Only one sperm wins, achieving fertilisation after a long and arduous journey. The resultant embryo, still in the fallopian tube, then descends downward until it reaches the uterine cavity, where it implants itself.
The Steps of Fertilisation
Fertilisation is a complex process, with the female body working in mysterious ways to align the egg and the sperm. Detailed below, are the steps that go into it.

- Step 1. Ovulation
Ovulation refers to the emergence of a single mature egg from one of the ovarian follicles. The egg only has a 24-hour window to be fertilised . During this time, vaginal discharge becomes wet and slippery, a telling sign that fertility is at its peak . Other ovulation symptoms include bloating and abdominal pain . If unprotected intercourse is had during this time or in the 5 days prior, there is a good chance that it will result in a pregnancy.

- Step 2. Ejaculation
Semen is a versatile substance, providing both nourishment and protection for sperm . As soon as ejaculation happens, the semen left behind forms a wall across the vagina to save sperm from moving downward. This wall lasts only about half an hour before it starts to trickle out of the vagina. The sperm cells that do make it through after ejaculation begin a long journey up the cervical canal, each holding out hope to make it to the egg first.

Step 3. Journey Through the Cervical Canal
The cervical canal is a warm and conducive environment that allows sperm to thrive and push on in their journey. Generously lined with cervical mucus, the canal is tailored for sperm transportation , especially during the fertile window when mucus is at its maximum. Interestingly, the days before ovulation will herald molecular changes that you may not even be aware of. Microscopic threads of molecules line up along the cervical canal, to allow sperm to latch on as they pace through.
- Step 4. Biochemical Alterations + Accelerated Movement
Sperm that enter the cervical canal must change their structural form in order to survive. Their new environment triggers biochemical changes that allow them to travel at breakneck speeds through the uterus and fallopian tubes.

- Step 5. Branching Off
Once sperm reach the uterus, they have a critical decision to make. Do they go right or left? There’s a fallopian tube on either side and it’s anybody’s guess which tube has released an egg this time. Sperm tend to branch out at this point, some gravitating to the left and others to the right.
Must read - 7 Pregnancy Questions to Ask your Doctor
Sperm that pick the correct tube has a significant chance of reaching the egg in time. Now, with about half the competitors as before, sperm must power to the finish line in time.
- Step 6. Fertilisation
Only the most resilient sperm reach the egg and even the ones that do must cross another hurdle before they can reach their final destination. Every egg is covered with a tough outer layer and hundreds of sperm engage in a race to see who can penetrate first. When one sperm finally does manage to achieve fertilisation, the egg immediately experiences chemical changes that block other sperm from entering. Then, the chromosomes in the egg and sperm combine, giving rise to a zygote.
Must read - How to Handle the 1st Trimester of Pregnancy?

- Step 7. Implantation
The zygote divides repeatedly over the next few hours and days. It gradually rolls down through the fallopian tube, reaching the uterine cavity about a week later as a 100-cell ball. The zygote now implants itself into the uterine lining, going on to develop into a baby.
You can also join our Cloudnine Community to discuss and get more information about - Aspiring Parents , Fertility Treatments .
Want to consult a Doctor? Book Video Consultation Online with the best gynecologist in India.
Watch Video on PCOD affect Fertility
As frenzied as the fertilisation process is, it marks the beginning of a chapter that will unfold page by page over the next nine months. By being in the know of how fertilisation works, you can stay better prepared in planning your family. So that when the arc lights in your womb are turned on, you’re still the director of the show.
Explore Cloudnine Momeaze for all your shopping needs with wide range of products.
Our customers had a few questions regarding this blog, check them out now!
How to track your ovulation date?
Slight spotting while conceiving with PCOS
Have Similar Questions?
Get answers from our experts, browse through hundreds of q&a, attend live sessions, and much more.
Want to consult the best gynecologists in India? Please find the links below.
- Best Gynecologists in Bangalore
- Best Gynecologists in Chennai
- Best Gynecologists in Mumbai
- Best Gynecologists in Pune
- Best Gynecologists in Chandigarh
- Best Gynecologists in Gurgaon
- Best Gynecologists in Noida
Want to consult the best Maternity Packages in India? Please find the links below.
- Best Maternity Packages in Bangalore
- Best Maternity Packages in Chennai
- Best Maternity Packages in Mumbai
- Best Maternity Packages in Pune
- Best Maternity Packages in Chandigarh
- Best Maternity packages in Gurgaon
- Best Maternity Packages in Noida
- [email protected]
- +91 99728 99728
Registered Office
Corporate office.
- Bengaluru Chandigarh Chennai Gurugram Hyderabad Ludhiana Mumbai Noida Panchkula Pune Mohali New Delhi Faridabad
- Specialities
- Parent Corner
- Media & News
- Home Services
- Virtual Tour
- Covid-19 Pregnancy Helpline
- Free Pregnancy Counseling
- Terms & Conditions
- Privacy Policy
- Company Policies
Best Gynecologists in India
- Best Gynecologists in Bengaluru
- Best Gynecologists in Bellandur
- Best Gynecologists in HRBR Layout
- Best Gynecologists in Jayanagar
- Best Gynecologists in Malleswaram
- Best Gynecologists in Old Airport Road
- Best Gynecologists in Whitefield
- Best Gynecologists in Sahakarnagar
- Best Gynecologists in Electronic City
- Best Gynecologists in Kanakapura Road
- Best Gynecologists in Industrial Area Phase II
- Best Gynecologists in T Nagar
- Best Gynecologists in OMR
- Best Gynecologists in Sector 14
- Best Gynecologists in Sector 47
- Best Gynecologists in Golf Course Road
- Best Gynecologists in Hyderabad
- Best Gynecologists in Hitech City
- Best Gynecologists in Banjara Hills
- Best Gynecologists in Gachibowli
- Best Gynecologists in Ludhiana
- Best Gynecologists in Malad
- Best Gynecologists in Vashi
- Best Gynecologists in Sector 51
- Best Gynecologists in Kalyani Nagar
- Best Gynecologists in SB Road
- Best Gynecologists in Pimple Saudagar
- Best Gynecologists in Panchkula
- Best Gynecologists in Sector 5 Swastik Vihar
- Best Gynecologists in New Delhi
- Best Gynecologists in Patparganj
- Best Gynecologists in Punjabi Bagh
- Best Gynecologists in Kailash Colony
- Best Gynecologists in Faridabad
- Best Gynecologists in New Industrial Town
Best Pediatricians in India
- Best Pediatricians in Bengaluru
- Best Pediatricians in Bellandur
- Best Pediatricians in HRBR Layout
- Best Pediatricians in Jayanagar
- Best Pediatricians in Malleswaram
- Best Pediatricians in Old Airport Road
- Best Pediatricians in Whitefield
- Best Pediatricians in Sahakarnagar
- Best Pediatricians in Electronic City
- Best Pediatricians in Kanakapura Road
- Best Pediatricians in Chandigarh
- Best Pediatricians in Industrial Area Phase II
- Best Pediatricians in Chennai
- Best Pediatricians in T Nagar
- Best Pediatricians in OMR
- Best Pediatricians in Faridabad
- Best Pediatricians in New Industrial Township
- Best Pediatricians in Gurugram
- Best Pediatricians in Sector 14
- Best Pediatricians in Sector 47
- Best Pediatricians in Golf Course Road
- Best Pediatricians in Hyderabad
- Best Pediatricians in Hitech City
- Best Pediatricians in Banjara Hills
- Best Pediatricians in Gachibowli
- Best Pediatricians in Ludhiana
- Best Pediatricians in Mumbai
- Best Pediatricians in Malad
- Best Pediatricians in Vashi
- Best Pediatricians in Noida
- Best Pediatricians in Pune
- Best Pediatricians in Kalyani Nagar
- Best Pediatricians in SB Road
- Best Pediatricians in Pimple Saudagar
- Best Pediatricians in Panchkula
- Best Pediatricians in Sector 5 Swastik Vihar
- Best Pediatricians in New Delhi
- Best Pediatricians in Patparganj
- Best Pediatricians in Punjabi Bagh
- Best Pediatricians in Kailash Colony
Best Physiotherapists in India
- Best Physiotherapists in Bengaluru
- Best Physiotherapists in Bellandur
- Best Physiotherapists in HRBR Layout
- Best Physiotherapists in Jayanagar
- Best Physiotherapists in Malleswaram
- Best Physiotherapists in Old Airport Road
- Best Physiotherapists in Whitefield
- Best Physiotherapists in Kanakapura Road
- Best Physiotherapists in Electronic City
- Best Physiotherapists in Sahakarnagar
- Best Physiotherapists in Chandigarh
- Best Physiotherapists in Industrial Area Phase II
- Best Physiotherapists in Chennai
- Best Physiotherapists in T Nagar
- Best Physiotherapists in Old Mahabalipuram Road (OMR)
- Best Physiotherapists in Faridabad
- Best Physiotherapists in New Industrial Township
- Best Physiotherapists in Gurugram
- Best Physiotherapists in Sector 14
- Best Physiotherapists in Sector 47
- Best Physiotherapists in Golf Course Road
- Best Physiotherapists in Hyderabad
- Best Physiotherapists in Hitech City
- Best Physiotherapists in Banjara Hills
- Best Physiotherapists in Gachibowli
- Best Physiotherapists in Ludhiana
- Best Physiotherapists in Mumbai
- Best Physiotherapists in Malad
- Best Physiotherapists in Vashi
- Best Physiotherapists in Noida
- Best Physiotherapists in Sector 51
- Best Physiotherapists in New Delhi
- Best Physiotherapists in Punjabi Bagh
- Best Physiotherapists in Patparganj
- Best Physiotherapists in Kailash Colony
- Best Physiotherapists in Pune
- Best Physiotherapists in Kalyani Nagar
- Best Physiotherapists in SB Road
- Best Physiotherapists in Pimple Saudagar
- Best Physiotherapists in Panchkula
- Best Physiotherapists in Sector 5 Swastik Vihar
Best Radiologist in India
- Best Radiologist in Bengaluru
- Best Radiologist in Bellandur
- Best Radiologist in HRBR Layout
- Best Radiologist in Jayanagar
- Best Radiologist in Malleswaram
- Best Radiologist in Old Airport Road
- Best Radiologist in Whitefield
- Best Radiologist in Kanakapura Road
- Best Radiologist in Electronic City
- Best Radiologist in Sahakarnagar
- Best Radiologist in Chandigarh
- Best Radiologist in Industrial Area Phase II
- Best Radiologist in Chennai
- Best Radiologist in T Nagar
- Best Radiologist in OMR
- Best Radiologist in Faridabad
- Best Radiologist in Gurugram
- Best Radiologist in Sector 14
- Best Radiologist in Sector 47
- Best Radiologist in Golf Course Road
- Best Radiologist in Hyderabad
- Best Radiologist in Banjara Hills
- Best Radiologist in Hitech City
- Best Radiologist in Gachibowli
- Best Radiologist in Ludhiana
- Best Radiologist in Mumbai
- Best Radiologist in Malad
- Best Radiologist in Vashi
- Best Radiologist in New Delhi
- Best Radiologist in Punjabi Bagh
- Best Radiologist in Kailash Colony
- Best Radiologist in Noida
- Best Radiologist in Sector 51
- Best Radiologist in Pune
- Best Radiologist in Kalyani Nagar
- Best Radiologist in SB Road
- Best Radiologist in Pimple Saudagar
- Best Radiologist in Panchkula
- Best Radiologist in Sector 5 Swastik Vihar
Best Dietitian in India
- Best Dietitian in Bengaluru
- Best Dietitian in Bellandur
- Best Dietitian in HRBR Layout
- Best Dietitian in Jayanagar
- Best Dietitian in Malleswaram
- Best Dietitian in Old Airport Road
- Best Dietitian in Whitefield
- Best Dietitian in Kanakapura Road
- Best Dietitian in Electronic City
- Best Dietitian in Sahakarnagar
- Best Dietitian in Chandigarh
- Best Dietitian in Industrial Area Phase II
- Best Dietitian in Chennai
- Best Dietitian in T Nagar
- Best Dietitian in OMR
- Best Dietitian in Faridabad
- Best Dietitian in New Industrial Township
- Best Dietitian in Gurugram
- Best Dietitian in Sector 14
- Best Dietitian in Sector 47
- Best Dietitian in Golf Course Road
- Best Dietitian in Hyderabad
- Best Dietitian in Banjara Hills
- Best Dietitian in Hitech City
- Best Dietitian in Gachibowli
- Best Dietitian in Ludhiana
- Best Dietitian in Mumbai
- Best Dietitian in Malad
- Best Dietitian in Vashi
- Best Dietitian in New Delhi
- Best Dietitian in Punjabi Bagh
- Best Dietitian in Patparganj
- Best Dietitian in Kailash Colony
- Best Dietitian in Noida
- Best Dietitian in Sector 51
- Best Dietitian in Pune
- Best Dietitian in Kalyani Nagar
- Best Dietitian in SB Road
- Best Dietitian in Pimple Saudagar
- Best Dietitian in Panchkula
- Best Dietitian in Sector 5 Swastik Vihar
Best Maternity Packages in India
- Best Maternity Packages in Bengaluru
- Best Maternity Packages in Faridabad
- Best Maternity Packages in Gurugram
- Best Maternity Packages in Hyderabad
- Best Maternity Packages in Ludhiana
- Best Maternity Packages in New Delhi
- Best Maternity Packages in Panchkula
Public egg and sperm bank: open for donations.
- Ovulation and conception
- Single and lesbian women
- Optimising conception
Every month, the reproductive organs in a healthy woman prepare for pregnancy.
A complex interaction between the pituitary gland in the brain, the ovaries and the uterus work to create the perfect environment for ovulation (the release of an egg) to occur, for the sperm and egg to meet and for the fertilised egg to implant itself in the uterus.
A step-by-step guide to ovulation
- Every month the pituitary gland, which is in your brain, releases a hormone. This hormone tells the ovaries to produce a number of fluid-filled cysts called follicles. As the follicles grow they secrete the hormone oestrogen. Oestrogen works to thicken the wall of your uterus in preparation for pregnancy.
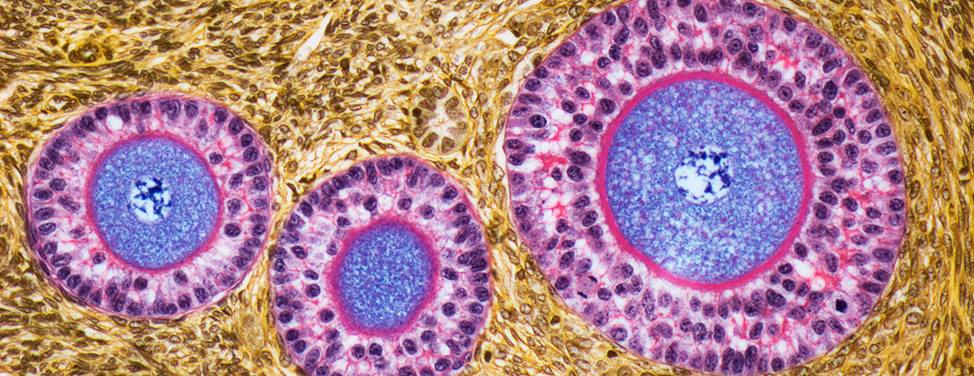
- On day seven of your cycle, the follicles stop growing except for one. This follicle continues to grow and to nourish a maturing egg (oocyte) within.
- On day 12 the maturing follicle releases a burst of oestrogen into the blood stream. The oestrogen travels through your blood. When the oestrogen reaches the pituitary gland in your brain, the pituitary gland responds by releasing the luteinising hormone. This hormone gives the follicle a sudden growth spurt.
- Right before ovulation, the egg inside the follicle detaches itself. The follicle starts to release chemicals that encourage the nearby fallopian tube to move closer and surround the follicle.
- The follicle swells until it bursts open, ejecting the egg and fluid into the abdominal cavity.
- Small finger like protrusions at the end of the fallopian tube, called fimbriae, sweep across the burst follicle and pick up the egg.
- The egg is transported to the entrance of the fallopian tube. Once inside the walls of the fallopian tube, muscle contractions push the egg gently towards the uterus.
- The egg will either meet sperm on its journey through the fallopian tube and fertilisation will happen, or it will arrive in the uterus unfertilised and be absorbed back into the body.

The menstrual cycle
A step-by-step guide to conception
After ovulation the egg lives for 12 to 24 hours and must be fertilised in that time if a woman is to become pregnant.
The burst of oestrogen just before ovulation also works inside the neck of the uterus (the cervix) to make protein-rich clear jelly that covers the top of the vagina during sex. This makes the vagina acidic (which prevents thrush and other infections). This is also a suitable environment for sperm survival. The sperm rapidly swim up and into the cervix, where they can survive in the mucus for up to five days before an egg is released.
When the egg is released at ovulation, it is covered in sticky cells, which help the fallopian tube to catch it. The egg and the sperm meet in the fallopian tube where the sperm start to digest the sticky cells. While it takes only one sperm to make a baby, several need to attach to the outer shell and the membrane of the egg before one can enter and fertilise it.
After fertilisation, the egg and sperm very quickly merge and divide to become an embryo and chemicals are released to stop other sperm from entering.
Over the next four or five days the fertilised egg continues to divide and to travel towards the uterus.
The hormone progesterone, which is secreted into your blood stream by the burst follicle (now called the corpus luteum) prepares the uterus for the egg to implant.
As the pregnancy grows and implants itself into the mother’s uterine lining and blood vessels, it is sending an increasingly strong signal to the ovary to prolong and increase its production of progesterone, which the pregnancy needs to survive.
Getting pregnant
The best time to attempt a pregnancy is in the three to six day leading up to and including ovulation. The most fertile days will vary depending on your cycle length.
If you are using contraception you will need to stop using it if you plan to get pregnant. There are no clear guidelines about when to stop using the Pill (oral contraception) if you are planning to get pregnant. Some health professionals suggest you have three normal menstrual periods, after stopping the Pill, to allow your metabolic function to return to normal. The length of time that it takes for fertility to return will differ for each woman. It is possible, although rare, for a woman to fall pregnant while on the Pill. There is no evidence that this causes problems for the baby.
Related information
- See also: Preparing for pregnancy for things to consider before you get pregnant
- Provide feedback about the content on this page
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Looks like you’re visiting UCSF Health on Internet Explorer. For the best experience, try Chrome or Firefox .

Stopping Seizures Before They Start
Find Conditions
Find Treatments
Clinical Trials
Patient Education
Medical Tests

Find a Doctor
Doctor Stories
- Get a Second Opinion

Find a Clinic
Locations & Directions
Partners & Affiliates
UCSF Benioff Children's Hospitals

Your Hospital Stay
For Visitors
International Services
For Caregivers
Support, Services & Groups
Billing & Insurance
Pricing Transparency
340B Drug Pricing Program
Medical Records
Patient Relations

Our Mission
Quality of Patient Care
Patient Stories
Embracing Diversity
Our Leadership
- Refer a Patient
- Request Appointment
- Call us: (888) 689-8273
Conception: How It Works
To become pregnant , the following steps must occur:
- Sperm transport . The sperm must be deposited and transported to the site of fertilization.
- Egg transport . Ovulation must occur and the egg must be "picked up" by the tube.
- Fertilization and embryo development . Union between the sperm and egg must result.
- Implantation . The embryo must implant and begin to grow in the uterus.
These steps are described below.

Sperm transport
The transport of sperm depends on several factors:
- The sperm must be capable of propelling themselves through the environment of the female vagina and cervix.
- This environment, which is under cyclic hormonal control, must be favorable to admit the sperm without destroying them.
- The sperm must possess the capability of converting to a form that can penetrate the cell membrane of the egg (capacitation).
Following ejaculation, the semen forms a gel that protects it from the acidic environment of the vagina. The gel is liquefied within 20 to 30 minutes by enzymes from the prostate gland. This liquefaction is important for freeing the sperm so transportation may occur. The seminal plasma is left in the vagina.
The protected sperm with the greatest motility travel through the layers of cervical mucus that guard the entrance to the uterus. During ovulation, this barrier becomes thinner and changes its acidity, creating a friendlier environment for the sperm. The cervical mucus acts as a reservoir for extended sperm survival.
Once the sperm have entered the uterus, contractions propel the sperm upward into the fallopian tubes. The first sperm enter the tubes minutes after ejaculation. The first sperm, however, are likely not the fertilizing sperm. Motile sperm can survive in the female reproductive tract for up to five days.
Egg transport
Egg transport begins at ovulation and ends once the egg reaches the uterus. Following ovulation, the fimbriated, or finger-like, end of the fallopian tube sweeps over the ovary. Adhesive sites on the cilia, which are located on the surface of the fimbriae, are responsible for egg pickup and movement into the tube. The cilia within the tube, and muscular contractions resulting from the movement of the egg, create a forward motion. Transport through the tube takes about 30 hours.
Conditions such as pelvic infections and endometriosis can permanently impair the function of the fallopian tubes, due to scarring or damage to the fimbriae.
Fertilization and embryo development
Following ovulation, the egg is capable of fertilization for only 12 to 24 hours. Contact between the egg and sperm is random.
Once the egg arrives at a specific portion of the tube, called the ampullar-isthmic junction, it rests for another 30 hours. Fertilization — sperm union with the egg — occurs in this portion of the tube. The fertilized egg then begins a rapid descent to the uterus. The period of rest in the tube appears to be necessary for full development of the fertilized egg and for the uterus to prepare to receive the egg.
Defects in the fallopian tube may impair transport and increase the risk of a tubal pregnancy, also called ectopic pregnancy.
A membrane surrounding the egg, called the zona pellucida, has two major functions in fertilization. First, the zona pellucida contains sperm receptors that are specific for human sperm. Second, once penetrated by the sperm, the membrane becomes impermeable to penetration by other sperm.
Following penetration, a series of events set the stage for the first cell division. The single-cell embryo is called a zygote. Over the course of the next seven days, the human embryo undergoes multiple cell divisions in a process called mitosis. At the end of this transition period, the embryo becomes a mass of very organized cells, called a blastocyst. It's now believed that as women get older, this process of early embryo development is increasingly impaired due to diminishing egg quality.
Implantation
Once the embryo reaches the blastocyst stage, approximately five to six days after fertilization, it hatches out of its zona pellucida and begins the process of implantation in the uterus.
In nature, 50 percent of all fertilized eggs are lost before a woman's missed menses. In the in vitro fertilization (IVF) process as well, an embryo may begin to develop but not make it to the blastocyst stage — the first stage at which those cells destined to become the fetus separate from those that will become the placenta. The blastocyst may implant but not grow, or the blastocyst may grow but stop developing before the two week time at which a pregnancy can be detected. The receptivity of the uterus and the health of the embryo are important for the implantation process.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Recommended reading

Eating Right Before and During Pregnancy
It is important to get the nutrients you need both before getting pregnant and during your pregnancy. Find more nutrition information including macros here.
FAQ: Fertility Services at UCSF
Find frequently asked questions regarding fertility services at UCSF including, when should you consider fertility services, success rates and more.

Infertility Risk Factors
Maternal age is probably the most significant factor related to a woman's ability to conceive. Learn about other infertility risk factors here.
Ovulation Induction
Ovulation induction uses hormonal therapy to stimulate egg development and release, or ovulation, the goal being to produce a single, healthy egg. Learn more.

Reducing Your Risk of Infertility
Your overall health is a reflection of your reproductive health. Give yourself a long and healthy life. Consider these tips to stay healthy.

Reproductive Surgery in Women
Some women have difficulty conceiving because of problems in their reproductive system such as a congenital malformation and require surgery. Learn more here.

The Menstrual Cycle
Hormones secreted by the hypothalamus, the pituitary and the ovary are the messengers that regulate the menstrual cycle. Learn more here.
Conditions we treat
High-risk pregnancy
Infertility in men
Infertility in women
Key treatments
Cryopreservation
Donor Sperm Insemination
In Vitro Fertilization (IVF)
Intrauterine Insemination (IUI)
Pre-Implantation Genetic Diagnosis
Related clinics

Center for Reproductive Health at Mission Bay
499 Illinois St., Sixth Floor San Francisco, CA 94158

Center for Reproductive Health at Mount Zion
2356 Sutter St., Seventh Floor San Francisco, CA 94115
Fertility Preservation Program
- Share on Facebook
- Share on Twitter
28.1 Fertilization
Learning objectives.
By the end of this section, you will be able to:
- Describe the obstacles that sperm must overcome to reach an oocyte
- Explain capacitation and its importance in fertilization
- Summarize the events that occur as a sperm fertilizes an oocyte
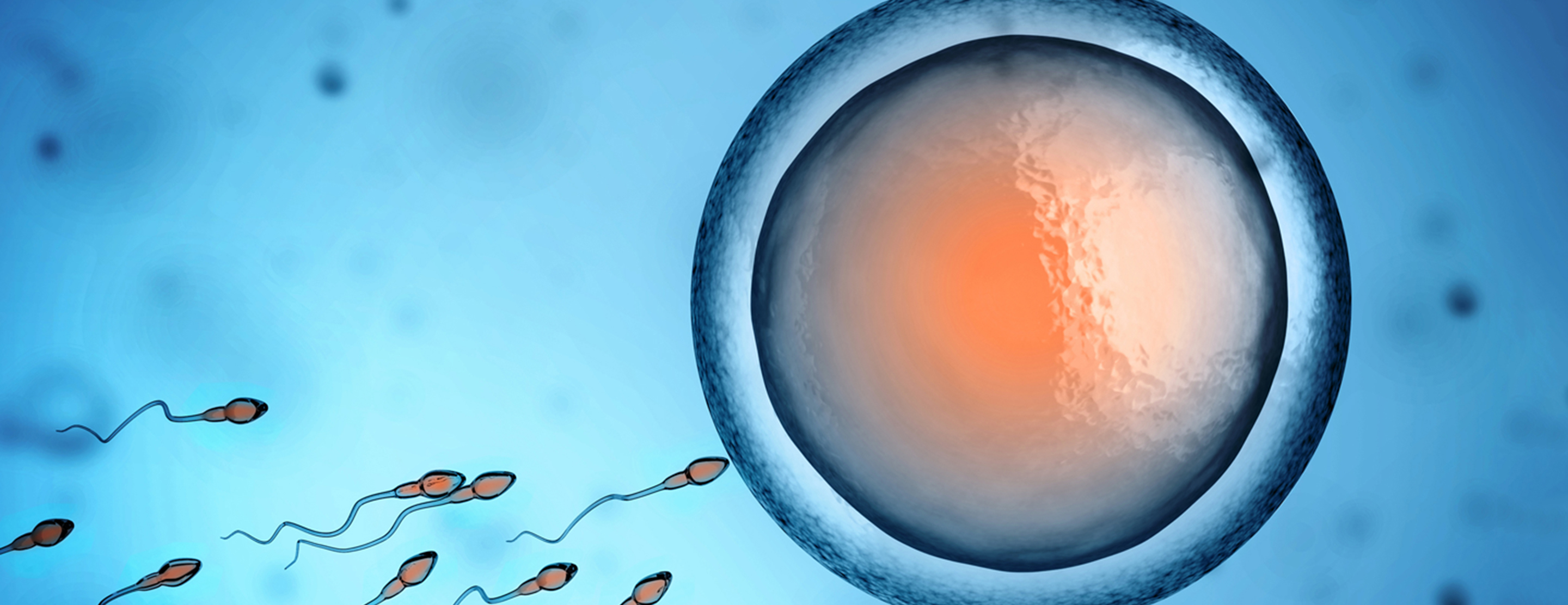
Fertilization occurs when a sperm and an oocyte (egg) combine and their nuclei fuse. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell, called a zygote , contains all of the genetic material needed to form a human—half from each biological parent.
Transit of Sperm
Fertilization is a numbers game. During ejaculation, hundreds of millions of sperm (spermatozoa) are released into the vagina. Almost immediately, millions of these sperm are overcome by the acidity of the vagina (approximately pH 3.8), and millions more may be blocked from entering the uterus by thick cervical mucus. Of those that do enter, thousands are destroyed by phagocytic uterine leukocytes. Thus, the race into the uterine tubes, which is the most typical site for sperm to encounter the oocyte, is reduced to a few thousand contenders. Their journey—thought to be facilitated by uterine contractions—usually takes from 30 minutes to 2 hours. If the sperm do not encounter an oocyte immediately, they can survive in the uterine tubes for another 3–5 days. Thus, fertilization can still occur if intercourse takes place a few days before ovulation. In comparison, an oocyte can survive independently for only approximately 24 hours following ovulation. Intercourse more than a day after ovulation will therefore usually not result in fertilization.
During the journey, fluids in the female reproductive tract prepare the sperm for fertilization through a process called capacitation , or priming. The fluids improve the motility of the spermatozoa. They also deplete cholesterol molecules embedded in the membrane of the head of the sperm, thinning the membrane in such a way that will help facilitate the release of the lysosomal (digestive) enzymes needed for the sperm to penetrate the oocyte’s exterior once contact is made. Sperm must undergo the process of capacitation in order to have the “capacity” to fertilize an oocyte. If they reach the oocyte before capacitation is complete, they will be unable to penetrate the oocyte’s thick outer layer of cells.
Contact Between Sperm and Oocyte
Upon ovulation, the oocyte released by the ovary is swept into—and along—the uterine tube. Fertilization must occur in the distal uterine tube because an unfertilized oocyte cannot survive the 72-hour journey to the uterus. As you will recall from your study of the oogenesis, this oocyte (specifically a secondary oocyte) is surrounded by two protective layers. The corona radiata is an outer layer of follicular (granulosa) cells that form around a developing oocyte in the ovary and remain with it upon ovulation. The underlying zona pellucida (pellucid = “transparent”) is a transparent, but thick, glycoprotein membrane that surrounds the cell’s plasma membrane.
As it is swept along the distal uterine tube, the oocyte encounters the surviving capacitated sperm, which stream toward it in response to chemical attractants released by the cells of the corona radiata. To reach the oocyte itself, the sperm must penetrate the two protective layers. The sperm first burrow through the cells of the corona radiata. Then, upon contact with the zona pellucida, the sperm bind to receptors in the zona pellucida. This initiates a process called the acrosomal reaction in which the enzyme-filled “cap” of the sperm, called the acrosome , releases its stored digestive enzymes. These enzymes clear a path through the zona pellucida that allows sperm to reach the oocyte. Finally, a single sperm makes contact with sperm-binding receptors on the oocyte’s plasma membrane ( Figure 28.2 ). The plasma membrane of that sperm then fuses with the oocyte’s plasma membrane, and the head and mid-piece of the “winning” sperm enter the oocyte interior.
How do sperm penetrate the corona radiata? Some sperm undergo a spontaneous acrosomal reaction, which is an acrosomal reaction not triggered by contact with the zona pellucida. The digestive enzymes released by this reaction digest the extracellular matrix of the corona radiata. As you can see, the first sperm to reach the oocyte is never the one to fertilize it. Rather, hundreds of sperm cells must undergo the acrosomal reaction, each helping to degrade the corona radiata and zona pellucida until a path is created to allow one sperm to contact and fuse with the plasma membrane of the oocyte. If you consider the loss of millions of sperm between entry into the vagina and degradation of the zona pellucida, you can understand why a low sperm count can cause male infertility.
When the first sperm fuses with the oocyte, the oocyte deploys two mechanisms to prevent polyspermy , which is penetration by more than one sperm. This is critical because if more than one sperm were to fertilize the oocyte, the resulting zygote would be a triploid organism with three sets of chromosomes. This is incompatible with life.
The first mechanism is the fast block, which involves a near instantaneous change in sodium ion permeability upon binding of the first sperm, depolarizing the oocyte plasma membrane and preventing the fusion of additional sperm cells. The fast block sets in almost immediately and lasts for about a minute, during which time an influx of calcium ions following sperm penetration triggers the second mechanism, the slow block. In this process, referred to as the cortical reaction , cortical granules sitting immediately below the oocyte plasma membrane fuse with the membrane and release zonal inhibiting proteins and mucopolysaccharides into the space between the plasma membrane and the zona pellucida. Zonal inhibiting proteins cause the release of any other attached sperm and destroy the oocyte’s sperm receptors, thus preventing any more sperm from binding. The mucopolysaccharides then coat the nascent zygote in an impenetrable barrier that, together with hardened zona pellucida, is called a fertilization membrane .
Recall that at the point of fertilization, the oocyte has not yet completed meiosis; all secondary oocytes remain arrested in metaphase of meiosis II until fertilization. Only upon fertilization does the oocyte complete meiosis. The unneeded complement of genetic material that results is stored in a second polar body that is eventually ejected. At this moment, the oocyte has become an ovum, the female haploid gamete. The two haploid nuclei derived from the sperm and oocyte and contained within the egg are referred to as pronuclei. They decondense, expand, and replicate their DNA in preparation for mitosis. The pronuclei then migrate toward each other, their nuclear envelopes disintegrate, and the male- and female-derived genetic material intermingles. This step completes the process of fertilization and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human.
Most of the time, a person releases a single egg during an ovulation cycle. However, in approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times.
Much less commonly, a zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins. Although the zygote can split as early as the two-cell stage, splitting occurs most commonly during the early blastocyst stage, with roughly 70–100 cells present. These two scenarios are distinct from each other, in that the twin embryos that separated at the two-cell stage will have individual placentas, whereas twin embryos that form from separation at the blastocyst stage will share a placenta and a chorionic cavity.
Everyday Connection
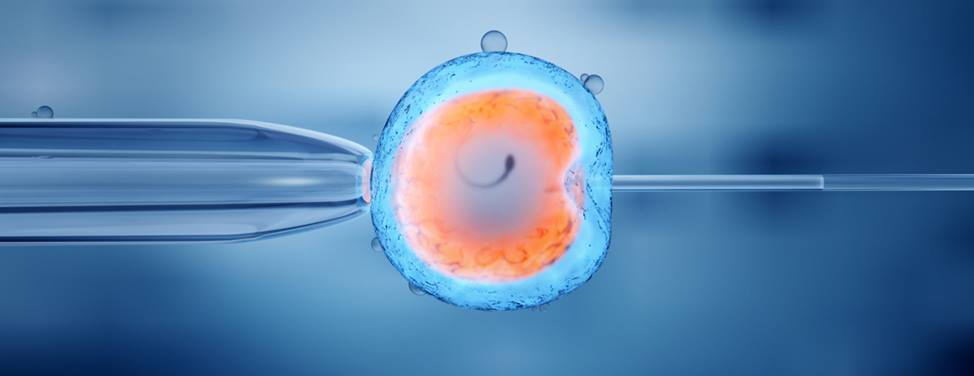
In vitro fertilization.
IVF, which stands for in vitro fertilization, is an assisted reproductive technology. In vitro, which in Latin translates to “in glass,” refers to a procedure that takes place outside of the body. There are many different indications for IVF. The procedure is used frequently in supporting LGBTQ people, people using surrogates/gestational carriers, and also people who have difficulties reproducing. For example, a person may produce healthy eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A person may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg.
A typical IVF procedure begins with egg collection. A normal ovulation cycle produces only one oocyte, but the number can be boosted significantly (to 10–20 oocytes) by administering a short course of gonadotropins. The course begins with follicle-stimulating hormone (FSH) analogs, which support the development of multiple follicles, and ends with a luteinizing hormone (LH) analog that triggers ovulation. Right before the ova would be released from the ovary, they are harvested using ultrasound-guided oocyte retrieval. In this procedure, ultrasound allows a physician to visualize mature follicles. The ova are aspirated (sucked out) using a syringe.
In parallel, sperm are obtained from the male partner or from a sperm bank. The sperm are prepared by washing to remove seminal fluid because seminal fluid contains a peptide, FPP (or, fertilization promoting peptide), that—in high concentrations—prevents capacitation of the sperm. The sperm sample is also concentrated, to increase the sperm count per milliliter.
Next, the eggs and sperm are mixed in a petri dish. The ideal ratio is 75,000 sperm to one egg. If there are severe problems with the sperm—for example, the count is exceedingly low, or the sperm are completely nonmotile, or incapable of binding to or penetrating the zona pellucida—a sperm can be injected into an egg. This is called intracytoplasmic sperm injection (ICSI).
The embryos are then incubated until they either reach the eight-cell stage or the blastocyst stage. In the United States, fertilized eggs are typically cultured to the blastocyst stage because this results in a higher pregnancy rate. Finally, the embryos are transferred to a woman’s uterus using a plastic catheter (tube). Figure 28.3 illustrates the steps involved in IVF.
IVF is a relatively new and still evolving technology, and until recently it was necessary to transfer multiple embryos to achieve a good chance of a pregnancy. Today, however, transferred embryos are much more likely to implant successfully, so countries that regulate the IVF industry cap the number of embryos that can be transferred per cycle at two. This reduces the risk of multiple-birth pregnancies.
The rate of success for IVF is correlated with the age of the gestational carrier (which may be the child's mother or a surrogate). More than 40 percent of females under 35 succeed in giving birth following IVF, but the rate drops to a little over 10 percent in females over 40.
Interactive Link
Go to this site to view resources covering various aspects of fertilization, including movies and animations showing sperm structure and motility, ovulation, and fertilization.
As an Amazon Associate we earn from qualifying purchases.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction
- Authors: J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix
- Publisher/website: OpenStax
- Book title: Anatomy and Physiology 2e
- Publication date: Apr 20, 2022
- Location: Houston, Texas
- Book URL: https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction
- Section URL: https://openstax.org/books/anatomy-and-physiology-2e/pages/28-1-fertilization
© Dec 19, 2023 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.

A Journey of Sperm
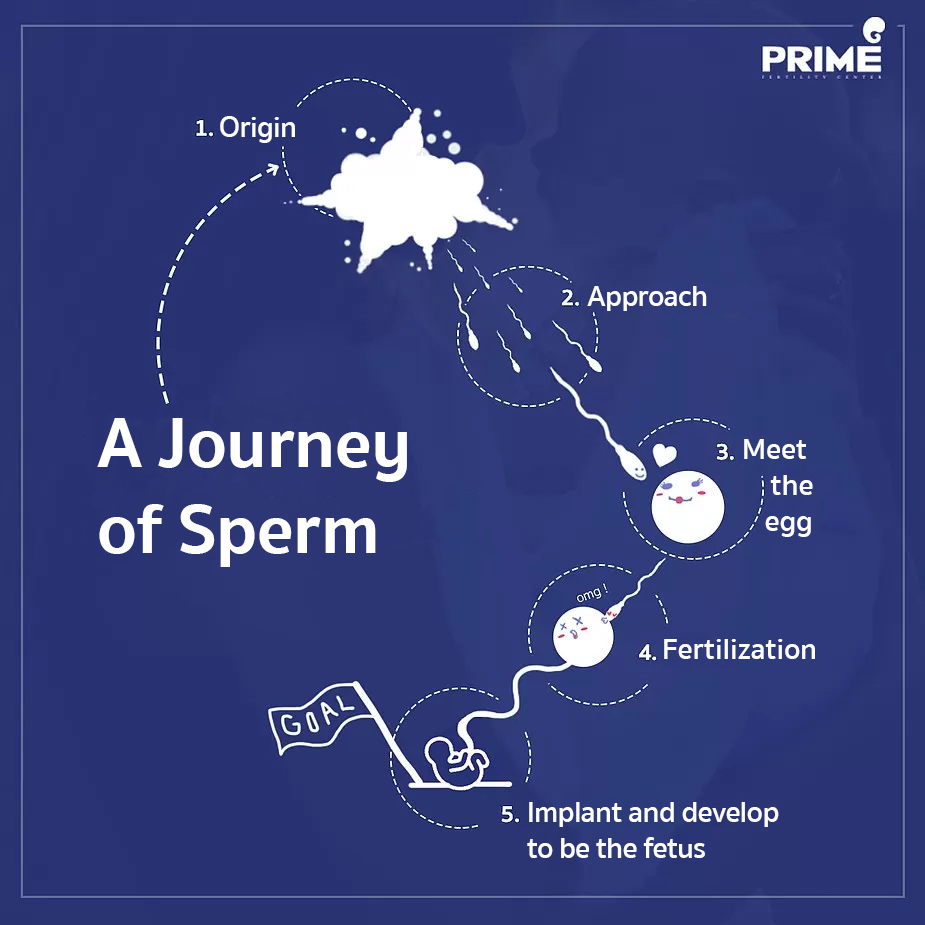
Sperm cells are produced from both testis of male. From germ cell and develop to become fully mature. This process takes around 70-80 days to complete.
After ejaculation, millions of sperm cells are moving to female’s vagina. A lot of sperm cells will be diving through vaginal mucus then aiming to cervix and uterine cavity. In this step, plenty of sperms die during approaching to the target.
Meet the egg
Once sperms (that still survive) reach the fallopian tubes, they will meet 1 fully matured egg which has passed the ovulation then moved to wait for sperm at the fallopian tubes. Each sperm will be approaching to this egg consequently.
Fertilization
Although the egg is surrounded by a lot of sperms, there will be only 1 strongest sperm can penetrate into the egg. After that sperm will throw off its tail and release 23 pairs of chromosomes to match with egg’s chromosomes. Combining to be 1 cell. The egg which has been fertilized already will transform itself in order to reject the approaching of any others sperm cells.
Implant and develop to be the fetus
After fertilization, the cell will be dividing very quickly. Then transfer from fallopian tubes to the uterine cavity in order to implant and grow up to be the fetus later on.
—–
Question about Infertility Treatment: Click Here Review Clip from Our Patients: Click Here
#ICSI #IUI #IVF #eggfreezing #EmbryoFreezing #SpermFreezing #SemenAnalysis #Hysteroscopy #FET #PGT #PGD #NGS #PESA #TESA #primefertilityclinic #primefertiltycenter #fertilityclinic #bangkokfertilityclinic #thailandfertilityclinic
Reference: Prime Fertility Center Co., Ltd. https://www.primefertilitycenter.com/en/a-journey-of-sperm/
Related Posts

Why don’t you have children yet? Check now if you are considered infertile or not.
Why don’t you have children yet? Check now if you are considered infertile or not. […]

ICSI, a technology that helps infertile people achieve pregnancy!
ICSI, a technology that helps infertile people achieve pregnancy! […]
©2019 Prime Fertility Center. All rights reserved.
เว็บไซต์นี้ใช้คุกกี้เพื่อวัตถุประสงค์ในการปรับปรุงประสบการณ์ของผู้ใช้ให้ดียิ่งขึ้น Read More
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Embryology, fertilization.
Rebecca Oliver ; Hajira Basit .
Affiliations
Last Update: April 17, 2023 .
- Introduction
Fertilization is a complex multi-step process that is complete in 24 hours. The sperm from a male meets an ovum from a female and forms a zygote; this is the point in which pregnancy begins and leads to a 280-day journey for a female. There are two ways to track this process, and they differ by the day counting begins. There are the post-ovulation age and the gestational age, calculated by adding two weeks to the last menstrual period. There are many steps that both the egg and sperm must go through for this process to be successful. Furthermore, the fertilized egg itself goes through drastic changes. This article will detail the process in the following sections.
- Development
In the first weeks after fertilization, the zygote makes many changes and develops rapidly. The first eight weeks of development is known as the organogenic period and is the embryonic stage of development. This period is a crucial phase of development for the embryo’s organs. During the first three weeks, teratogens have an all or nothing effect on the embryo. During the third through eighth-week growth and function are affected. Weeks nine to thirty-seven are known as the fetal period. This period is important for extensive growth in size and continuous differentiation of organ systems. The respiratory system completes development just prior to birth. An important part of embryology that does not complete during the embryonic or fetal phase is gametogenesis. In both males and females, these processes begin during the fetal period and continue into puberty. This process is a mitotic and meiotic process that results in the production of an ovum and sperm. [1] Before turning into gametogonia, the embryonic development of gametes is the same in males and females, and at week ten they can be differentiated. Primordial germ cells migrate from the dorsal endoderm of the yolk sac to the hindgut of the gonadal ridge where they go through mitotic divisions and become the gametogonia.
Once fertilization takes place, there are quick changes at the cellular level of the zygote. The zygote is a single cell, and it undergoes mitosis to create many cells. Once the zygote has reached the thirty-two cell stage, it becomes morula. Day four begins blastulation and cavities begin to form by first forming a hollow ball. Some studies suggest that the timing of this process may affect implantation. [2] There are now two different cell types, an inner and outer. The inner cells are called the inner cell mass, and the exterior is known as the trophoblast, which later helps form the placenta, and the inner cell mass becomes the embryo. The inner cell mass will further differentiate into the epiblast and the hypoblast. The hypoblast will become the primitive yolk sac, and the epiblast will become the amniotic sac. During this phase, the entity is a blastula, and the zona pellucida is now gone, allowing for growth and differentiation. During week three, tubes will form, and this is known as the gastrulation phase. Movements during gastrulation are dependent on differential cell adhesion, chemotaxis, chemokinesis, and planar polarity. [3] During this time, there are three layers of cells that will make up different organ systems. These are known as the endoderm, mesoderm, and ectoderm. The ectoderm forms the epidermis, nails, hair, peripheral nervous system, brain, and spinal cord. The mesoderm forms the muscle, bone, connective tissue, notochord, kidney, gonads, and circulatory system. The endoderm forms the epithelial lining of the digestive tract, stomach, colon, liver, bladder, and pancreas. At sixteen weeks the primitive streak forms. The primitive streak establishes the midline of the body. The next stage in development is neurulation. At this time the notochord induces the ectoderm to form the neural plate which eventually forms the neural tube. The neural tube will become the brain and spinal cord. The mesoderm divides into the axial, paraxial, intermediate, and lateral plate mesoderm, which give rise to different body parts — the paraxial mesoderm forms somites, which differentiate into cartilage, muscle, bone, and dermis. The intermediate mesoderm becomes the urogenital system, and the lateral plate mesoderm becomes the heart and vessels. The endoderm becomes the gastrointestinal tract, and the ectoderm will meet the endoderm forming the mouth and the anus. An important gene regulatory mechanism is Dkk1; the deletion of Dkk1 is known to cause an imperforate anus with a rectourinary fistula. [4]
- Biochemical
There are significant changes that the egg and sperm must undergo for the fertilization process to occur; this starts as soon as sperm gets deposited in the vagina. Sperm undergoes capacitation to have increased motility and metabolism to help it make the journey to the fallopian tube. Capacitation occurs due to the acidic environment of the vagina. It activates ATP enzymes in the cytosol of the sperm. The process of capacitation is important because it makes changes in the plasma membrane by altering the lipid and glycoprotein composition, which is one of two changes the sperm undergoes during this process. [5] The second change helps penetrate the matrix. The egg’s extracellular matrix is difficult to penetrate. The acrosome on the sperm contains important lysosomal enzymes. These enzymes are considered to be released by exocytosis and required for the penetration of the egg. [6] Hyaluronidase from the acrosome digests the cells embedded in hyaluronic acid surrounding the oocyte. This process exposes acrosin, which is in the inner membrane of the sperm. Acrosin is necessary to digest the zona pellucida. Once the acrosome reaction takes place, no other sperm may penetrate the zona pellucida; this is imperative so that the appropriate number of chromosomes is available and that there is not a trisomy zygote. The fusion of the acrosome of the sperm to the zona pellucida induces a rise in calcium. This rise in calcium stimulates secretory vesicles known as cortical granules to expel contents, which modifies the extracellular matrix. The cortical granules release enzymes that make it impenetrable to sperm entry by digesting sperm receptor glycoproteins ZP2 and ZP3 so that they can no longer bind spermatozoon. [7]
- Molecular Level
We have discussed in previous sections changes occurring at the biochemical and cellular levels. Here we will discuss the molecular changes taking place during the fertilization process. Before the actual fertilization process occurs, the sperm travels to the fallopian tubes where it will penetrate the egg. The spermatozoa in ejaculate vary, and the make-up of each spermatozoon contributes to its ability to get to the egg and fertilize it. [8] Spermatozoa have differences in DNA fragmentation status, motility, morphology, and sensitivity to signaling molecules. Diving even deeper into this topic, research has shown that spermatozoa with stable chromatin reach the fertilization site with greater ease and can bind well. [9] The sperm and egg are two haploid nuclei that join to form a diploid nucleus. Once the sperm and egg have joined their membranes and fused, the zygote undergoes mitotic divisions. As mentioned before, the changes the egg undergoes once one acrosome has penetrated its membrane to keep other sperm out to prevent triploidy is crucial from a molecular standpoint. The sperm has a vital role in providing a centriole, which helps organize and assemble the mitotic spindle. [10]
The function of fertilization is to create a diploid(2N) zygote. Fertilization by a sperm activates the ovum, which takes place in the distal third of the fallopian tube. Once the sperm has entered the ovum, immediate changes take place not to allow further penetration of the ovum. These exact changes are in the biochemical section of this article. Once the sperm has penetrated the ovum, the sex of the embryo will be determined based on the presence or absence of a Y chromosome, which contains the SRY gene known as the testis-determining factor and also known as sex-determining region Y.
A follicle must mature from an oocyte to a Graafian follicle to be ready for fertilization. During ovulation, the follicle will be released and swept into the fallopian tube. If the sperm were deposited in the last ten hours, the spermatozoa would have made their way to this location, and fertilization can occur. Fertilization must take place within twenty-four hours of ovulation; otherwise, the ovum will not be available to be fertilized and will end in menses. The follicle has two layers that the sperm must penetrate, both the corona radiate and zona pellucida. The first step is the penetration of the corona radiata. The acrosome of the spermatozoa then releases enzymes, which aid in the digestion of this layer and allows for access to the secondary oocyte.
Infertility is a common problem encountered in the medical community. If a female patient cannot become pregnant after one year of unprotected intercourse performed regularly, an evaluation is in order. An important consideration is the patient’s body mass index. If a patient is overweight, weight loss may improve her chances of becoming pregnant. [11] It is essential to consider labs in patients who are unable to become pregnant because abnormalities of the thyroid gland or androgen excess may indicate an endocrinopathy. A commonly encountered endocrinopathy that causes issues with fertility is polycystic ovarian syndrome. In PCOS, testosterone increases, which interferes with egg maturation. [12] A physical exam is also useful in evaluating infertility. Masses or tenderness in the adnexae or the pouch of Douglas is consistent with endometriosis or chronic pelvic inflammatory disease. Furthermore, structural abnormalities may suggest an infection, leiomyoma, malignancy, or Mullerian anomaly. In women who are not suspected to be ovulating, it is crucial to do a thorough hormone analysis to investigate if ovulation is occurring. A mid-luteal progesterone level should be tested one week before expected menstruation. To show proof of ovulation, a progesterone level greater than 3 ng/mL is the expectation. Another useful hormone to evaluate female fertility is the anti-Mullerian hormone. [13] This hormone is in the TGF-beta family and expresses itself by small early antral follicles. These levels reflect the size of the primordial follicle pool and are a good indicator of ovarian function.
- Clinical Significance
There are numerous clinical scenarios in which fertilization comes into play. Fertilization and the development that follows is a delicate and complex process that can result in defects. Hormones are important for preparing the female body to implant a fertilized egg and to grow and nourish it. FSH, which causes the release of estrogen from the ovaries, aids the cervical mucus in being more hospitable to sperm movement through the vaginal canal and cervix. An LH surge is necessary for the release of an egg from the ovary out of the follicle and into the fallopian tube where it can undergo fertilization. Progesterone produced by the corpus luteum and later by the placenta creates and maintains a thickened endometrium to allow a nourishing environment for implantation and growth. Pregnancy tests detect fertilization by measuring beta-human chorionic gonadotrophin released by the growing placenta after implantation. Another important clinical significance is neural tube defects, which are birth defects of the central nervous system that occurs when the neural tube fails to close completely. [14] Folic acid supplementation during pregnancy has been shown to help prevent neural tube defects, thus is a commonly recommended prenatal supplement. Another important clinical consideration is a group of genes known as Hox genes, which play a significant role in body plan and development along the cephalic to the caudal axis. If there are mutations in these genes, then body parts may develop in the incorrect location. [15]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Rebecca Oliver declares no relevant financial relationships with ineligible companies.
Disclosure: Hajira Basit declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Oliver R, Basit H. Embryology, Fertilization. [Updated 2023 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Volume changes during the preimplantation stages of mouse egg development. [Yonsei Med J. 1973] Volume changes during the preimplantation stages of mouse egg development. Chung SO. Yonsei Med J. 1973; 14:63-90.
- A study of hetero-specific sperm-egg interactions in the rat, mouse, and deer mouse using in vitro fertilization and sperm injection. [J Exp Zool. 1980] A study of hetero-specific sperm-egg interactions in the rat, mouse, and deer mouse using in vitro fertilization and sperm injection. Thadani VM. J Exp Zool. 1980 Jun; 212(3):435-53.
- Intracellular sperm/egg interactions in Drosophila: a three-dimensional structural analysis of a paternal product in the developing egg. [Mech Dev. 1991] Intracellular sperm/egg interactions in Drosophila: a three-dimensional structural analysis of a paternal product in the developing egg. Karr TL. Mech Dev. 1991 Jun; 34(2-3):101-11.
- Review The mode of action of IUDs. [Contraception. 1987] Review The mode of action of IUDs. Ortiz ME, Croxatto HB. Contraception. 1987 Jul; 36(1):37-53.
- Review Intracellular calcium signaling in the fertilized eggs of Annelida. [Biochem Biophys Res Commun. 2014] Review Intracellular calcium signaling in the fertilized eggs of Annelida. Nakano T, Deguchi R, Kyozuka K. Biochem Biophys Res Commun. 2014 Aug 1; 450(3):1188-94. Epub 2014 Jun 19.
Recent Activity
- Embryology, Fertilization - StatPearls Embryology, Fertilization - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Getting Pregnant
- Log a Period
The Journey of Sperm [Like Never Seen Before]

By Professor Allan Pacey BSc, PhD, FRCOG - University of Sheffield
For successful conception, sperm need to make the most remarkable journey through the bodies of men and women. It is a journey that scientists have only recently been able to understand in any detail, with new discoveries being made all the time. This article outlines our current knowledge and explains what makes for a winning sperm, but also why the majority of sperm never make it at all.
The journey of sperm begins inside the testicles. Males begin to produce sperm at the start of puberty at around 12 or 13 years old. It is a process that requires a slightly cooler temperature, which is why testicles hang outside men's bodies. Nor is it a quick process: the production of sperm takes about 70 days. Exactly how many sperm come off the production line is also critical to how fertile each man is.
In simple terms, the larger a man's testicles the greater the number of sperm produced per unit time. This is because inside bigger testicles there are more of the sperm pre-cursor cells (called spermatogonia) that divide and multiply and go on to make new sperm. Also, there are more of the intricate labyrinths of tubes and nurse cells that are critical for the production of sperm. Quite simply, the bigger the factory the bigger the quantity of sperm produced.
about 1,000 sperm roll off the production line with every heartbeat
In a typical fertile male, about 1,000 sperm roll off the production line with every heartbeat. However, before they are finally ready for release, sperm first spend another week or so passing through a long winding tube called the epididymis. Here finishing touches are added to them, including modifications to the molecules on their surface that ultimately will help when they reach the egg. In addition, there are also some 'tweaks' to the machinery of the tail that will help them swim better when the time comes.
Once sperm leave the epididymis, they can remain alive, healthy and motionless for several weeks in the man's body without being released. Men have the capacity to store many billions of sperm, but if sperm are stored for too long, then they can start to degenerate and die. This is a natural process designed to dispose of old sperm. However, if ejaculation does not happen often, then older degenerating sperm can damage newer sperm leaving the epididymis. Therefore, scientists recommend that men ejaculate every two or three days to keep the reservoir of sperm in optimal condition.
When ejaculation finally happens, about 250 million of the sperm being stored are propelled by muscular contractions through a tube called the vas deferens and then into the tube passing down the penis (the urethra) that eventually leads to the outside world. It is the muscular contractions that contribute to the feeling of orgasm that men experience during intercourse. Typically, there are several spurts of fluid from the end of the penis at orgasm. The majority of sperm are in the first spurt, with the second and third containing fluid from the prostate gland and other structures called the seminal vesicles. It is now that the sperm begin swimming for the first time.
Once inside the vagina, sperm must escape quickly if they are to survive. Perhaps surprisingly, the environment of the vagina is quite acidic. This is an important defense mechanism to protect women's bodies from attack by bacteria and viruses in everyday life. However, following sexual intercourse, these acids would also quickly kill sperm if the fluids from the prostate and seminal vesicles did not give them some protection.
Therefore, in those few minutes immediately after ejaculation it is the fastest, healthiest or just plain luckiest sperm that have enough time to swim out of the vagina and into the relative safety of the cervix. Slow, deformed or unlucky sperm are left behind in the vagina and quickly die. A woman's cervix acts as an amazing filter and it's easy to see how men who produce too few 'mucus penetrating sperm' may find it difficult to get their partner pregnant and therefore may suffer infertility as a consequence.
only about 1 in 100 of the sperm ejaculated into the vagina will ever make it into the relative safety of the cervix
As a general rule of thumb, scientists think that only about 1 in 100 of the sperm ejaculated into the vagina will ever make it into the relative safety of the cervix. However, to make matters more complicated, this will also depend on the hormone profile of the woman and how close she is to releasing an egg from her ovaries. It is only in those few days immediately before ovulation that a woman's cervical mucus allows sperm inside. Outside this fertile window, even the strongest and fastest sperm will find it impossible to get inside.
Learn when your fertile window is with Ovulation Calculator.
Entering the cervix is, however, only the very start of a sperm's journey through a woman's body. The next step is how to get through the womb and into one of the Fallopian tubes. Although it is a journey of only about 10 or 12 centimeters, there are a number of hazards along the way.
The first hurdle for sperm that successfully enter the womb is whether to go left or right. This is because women have two Fallopian tubes (one at either side) but since only one of her ovaries will release an egg in any given month, sperm must swim into the right one. To make their way down a Fallopian tube toward an ovary that isn't going to release an egg would be a wasted journey! Thankfully, to increase the odds of sperm getting it right, the woman's body comes to the rescue.
Briefly, as the egg gets closer to being released from the ovary, some of the hormones that are produced to help the egg grow also enter the woman's bloodstream. These trigger muscles in the wall of the womb closest to it start rhythmically contracting upward, slowly moving sperm gently toward the entrance of the Fallopian tube on the same side. Because the muscles on the other side (which isn't growing an egg) receive fewer hormones, they don't contract as much meaning sperm generally don't go in that direction.
However, getting to the opening of one of the woman's Fallopian tubes, on the side of her body where the egg is about to appear from, is only part of the journey. Here the woman's body has another trick up her sleeve. Although the entrance to the Fallopian tube is a tiny opening only a few sperm heads wide, it acts as a valve only letting certain sperm inside. This again means that the woman's body is selecting sperm to make sure that only the best ones get close to the egg.
Scientists think that sperm are selected to enter the Fallopian tubes in two ways. First, some experiments have shown that if sperm swim too erratically then they are unable to get inside. Sperm that swim like this are nearing the end of their life and so perhaps they are being excluded because they won't live long enough to find an egg. Second, there is some evidence that sperm with certain molecules on their surface can't get into the Fallopian tube either. Quite how this works is unclear, but again it shows that not just any sperm can complete the journey. Of the many millions of sperm that were ejaculated into the vagina, only perhaps a hundred get this far!
Once inside the Fallopian tubes, sperm are in a relatively safe place in comparison to the rest of their journey so far. Here the female body helps them survive and remain in a healthy condition until the egg is ready to be released. For example, several research studies now suggest that inside the Fallopian tubes, sperm tend to stick to the inner walls by the tip of their head. Studies have shown that sperm that stick tend to live longer and have better quality DNA in their heads than sperm that don't.
Some scientists believe that when sperm attach and stick to the sidewalls of the Fallopian tube, this gives the woman's body a signal to say sperm have finally arrived. Others have suggested that once sperm are stuck, new molecules are produced by the cells which line the inside of the Fallopian tube which may ultimately help in fertilization or embryo development. Whilst it is hard to know for sure, one thing is clear: if sperm are to fertilzse an egg they must free themselves from the sidewalls as soon as it appears.
Quite how long sperm can remain stuck to the sidewalls of the Fallopian tube is unclear. But to pull themselves away, they increase the beat of their tail to give them extra thrust. This type of swimming is called hyperactivation and it's very important in these final stages of a sperm's journey.
Once free from the sidewalls, then sperm need to make their way down the Fallopian tube in the direction of the ovary in order to find an egg that will be shortly coming in the other direction. Quite how they do this is not completely clear, but probably involves one or both of the following mechanisms:
First, inside the Fallopian tube there is probably a subtle change of temperature that occurs once the egg is released from the ovary. Experiments in the laboratory suggest that sperm are 'positively thermotaxic' which means they preferentially swim to a warmer place. It has been suggested that after ovulation has occurred it is one or two degrees Celsius warmer in the middle of the Fallopian tube (where the egg will eventually arrive) so sperm will naturally make their way there.
Second, it has also been suggested that sperm are able to detect subtle chemical signals, either given off by the egg once it is released from the ovary or that are released from the ovary at the same time as the egg (perhaps in the fluid that bathes the growing egg). The response of sperm to these signals is called chemotaxis and if true, it will be a powerful attractant to guide the sperm to the egg.
probably only half a dozen sperm ever get this far!
Either way, one or both of these mechanisms will serve to make sure that there are a few sperm present in the middle of the Fallopian tube in time for the egg to appear. This is important because, in comparison to sperm, the egg only has a limited life and once released from the ovary will need to be fertilized within a few hours if conception is to occur. Therefore it is critical that sperm get to the right place in the Fallopian tube before the egg arrives. However, probably only half a dozen sperm ever get this far!
In comparison to sperm, the egg is quite a large cell - the largest in the human body. In addition, it is released from the ovary surrounded by a cloud of cells called the cumulus through which the sperm must first penetrate before they can reach and make contact with the egg surface. To assist sperm to get through the cumulus, the sperm must again use the erratic and frenetic swimming style (hyperactivation) that they used to pull away from the sidewalls of the Fallopian tube.
At this point in the sperm's journey there are perhaps only one or two sperm close to the egg and with any chance of fertilizing it. However, for the successful sperm, there is one more hurdle left: how to get inside the egg once it reaches the egg surface. To some extent, the hyperactivated tail beat that helped the sperm get free of the Fallopian tube side walls and through the cloud of cumulus cells will also assist here. But for additional help there is a bag of enzymes on the very top of the sperm head that bursts once the winning sperm makes contact with the outer surface of the egg.
The enzymes help dissolve the outer membrane of the egg and in combination with the powerful tail thrusts, assist the sperm in penetrating the egg and getting inside. Once this is achieved, then there is an immediate chemical reaction inside the egg that suddenly hardens the egg membrane and stops other sperm from following it. If two sperm were to fertilize the egg, the egg would then contain too many chromosomes and in the resulting confusion embryo development would fail to occur.
Over the following few hours the sperm tail is detached (this stays outside) and the chromosomes inside the sperm head separate and line up with those from the egg to start the process of forming a new individual. At this point the sperm's journey has ended, but the journey of the embryo has only just begun.
See how the race of the winning sperm unfolds in our infographic
Click the image below to see a larger view
Embed the The Journey of Sperm infographic on your site (copy the code below):
<div style="clear:both"><a href="https://www.ovulationcalculator.com/journey-of-sperm-infographic/"><img src="https://www.ovulationcalculator.comhttps://www.ovulationcalculator.com/img/uploads/2015/08/sperm_infographic.jpg" title="The Journey of the Winning Sperm" alt="The Journey of the Winning Sperm" border="0" /></a></div><div>Courtesy of: <a href="https://www.ovulationcalculator.com/journey-of-sperm-infographic/">Ovulation Calculator</a></div>
Take the fertility quiz
Take our fertility quiz to test your fertility knowledge! Fertility Knowledge Quiz
Join the Discussion!
Add your own comment
Remove the guess work and get the timing right!
1 Tell us your cycle 2 Tell us about you 3 Get accurate predictions
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
What to know about intrauterine insemination (IUI)

Intrauterine insemination (IUI) can increase their likelihood of becoming pregnant. The procedure involves collecting sperm and inserting it into the uterus.
The success rate of IUI depends on the age of both partners, their fertility, and whether or not they use fertility drugs. If a couple undergoes the procedure every month, the success rate may be up to 20% per cycle.
However, the risks of IUI include infections and multiple births.
Read on to learn how IUI works, how much it costs, its risks, and more.
How does it work?

To understand how IUI works, it helps to know what happens during a typical conception.
Following ejaculation, sperm moves up the vagina and into the cervix, which is the opening to the uterus. After navigating through the cervix, the sperm move into the uterine cavity and then the fallopian tubes. These are a pair of tubes that capture the egg after it releases from the ovary.
If sperm are in the fallopian tube when the egg arrives, the egg and sperm can meet. The egg can undergo fertilization and become an embryo. The embryo then travels back through the fallopian tube and into the uterus, where it implants to become a pregnancy.
The cervix is a natural barrier to sperm movement. This means that after ejaculation, only a small percentage of sperm can move past the cervix and into the uterus.
An IUI procedure sidesteps this issue by inserting the sperm past the cervix and into the uterus. This shortens the distance the sperm travels to reach the fallopian tubes, increasing the likelihood that one sperm will meet and fertilize the egg.
IUI procedure step by step
The IUI procedure consists of the following steps :
- masturbating into a sterile container
- retrieving into a special condom during sex
- extracting from a urine sample in a lab
- collecting while undergoing vibratory stimulation
- Sperm sample washing: This involves the removal of the seminal fluid from the sample because it can cause severe cramping in the female. This part can take 1–2 hours.
- Sperm insertion: The individual will lie down as a healthcare professional inserts a thin, flexible catheter through the cervix into the uterus. They then slowly inject the sperm sample. This takes a few minutes.
Cost, access, and insurance
Although IUI can help people fall pregnant, it can be relatively expensive. This limits access, as insurance does not always cover the procedure. A 2018 study reports that for most people, insurance companies do not cover infertility treatments as they do for other medical conditions.
However, it is important to note that IUI is a minimally invasive strategy that is typically less expensive than other assistive fertility methods, specifically in-vitro fertilization (IVF).
Just 15 states have laws that mandate that insurance companies cover a portion of infertility costs. This means in many cases, individuals have to pay out of pocket. Cycles generally range from one to several thousand dollars.
Success rate
The success of an IUI procedure depends upon several factors, including:
- the reason for infertility
- the age of both partners
- the use of fertility drugs
If a couple undergoes the procedure every month, the success rate may be as high as 20% per cycle. However, older research from 2010 that evaluated 366 people found that IUI resulted in a pregnancy rate of around 8.7% and a live birth rate of around 5.8%.
Because the success rates vary greatly from person to person, individuals considering IUI can discuss the likelihood of pregnancy with a healthcare professional.
If a female takes fertility medications while undergoing IUI, the likelihood of becoming pregnant with twins, triplets, or multiple births is higher. Twins or higher-order multiple pregnancies — pregnancies involving three or more fetuses —carry significantly higher risks to the pregnant individual and their fetuses, including premature birth .
Additionally, the risks of IUI involve a small chance of infection.
IUI is less effective in people with severe sperm abnormalities or who produce few sperm. It also does not help individuals with:
- moderate to severe endometriosis
- fallopian tube blockage or damage
- uterine abnormalities
When to contact a doctor
Following an IUI procedure, an individual should contact a doctor if they experience severe abdominal pain or other side effects.
Two weeks after an IUI, a person may wish to take a home pregnancy test . However, a blood test is a more accurate means of determining if fertilization has occurred, so someone should ask their doctor if they recommend this.
If the IUI does not lead to a pregnancy, a doctor can advise whether to repeat the procedure or try a different type of fertility treatment, such as IVF.
Learn more about IVF.
IUI increases the likelihood of fertilization because it results in more sperm reaching the area where one can meet an egg and unite. Even though the cost is less than the cost of IVF, it can still be a barrier for some as it often does not have insurance coverage.
The success rate depends on factors such as the condition underlying infertility. A person should be aware that taking fertility medications while undergoing IUI can increase the risk of multiple births.
Last medically reviewed on December 22, 2022
- Pregnancy / Obstetrics
- Getting Pregnant
How we reviewed this article:
- Allahbadia, G. N. (2017). Intrauterine insemination: Fundamentals revisited. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5676579/
- Dupree, J. M. (2018). Insurance coverage of male infertility: What should the standard be? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6087851/
- Intrauterine Insemination: IUI. (n.d.). https://americanpregnancy.org/getting-pregnant/intrauterine-insemination/
- Intrauterine Insemination (IUI) [Fact sheet]. (2016). https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/intrauterine-insemination-iui/
- Kamath, M. S., et al . (2010). Predictive factors for pregnancy after intrauterine insemination: A prospective study of factors affecting outcome. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3017328/
Share this article
Latest news
Related coverage.
Artificial insemination, or intrauterine insemination (IUI) is used to treat infertility. It involves direct insertion of semen into a woman's womb…
Females are most fertile within two days ovulation. However, it is also possible to get pregnant in the the days around ovulation. Learn more here.
Modern Fertility offers a way monitor and track reproductive hormones. Learn about the reliability of the tests, how they work, and more.
A female fetus has around 6-7 million eggs. But this number drops as a person ages to around 1,000 at menopause. Learn more here.
All about sperm
Pathway of Sperm from Testes to Urethra: Understanding the Male Reproductive System
Short answer pathway of sperm from testes to urethra: Sperm travel through the epididymis and vas deferens to reach the ejaculatory ducts, where they mix with seminal fluid. The mixture then passes through the prostate gland and into the urethra before being expelled during ejaculation.
Understanding the Pathway of Sperm from Testes to Urethra: An Overview
The step-by-step guide to the pathway of sperm from testes to urethra, common faqs about the pathway of sperm from testes to urethra answered, troubleshooting problems that can impact the pathway of sperm from testes to urethra, examining the role of ejaculation in facilitating the movement of sperm along the pathway.
Table of Contents
As we all learned in our high school biology class, the process of procreation involves the fusion of a male sperm and female egg to create a new life. But have you ever wondered about the journey that these tiny little swimmers undertake before reaching their final destination? It may seem like a simple concept, but understanding the pathway of sperm from testes to urethra is a crucial aspect of human anatomy and reproductive health.
So, let’s get down to business. The journey of a million sperms begins in the testes- two egg-shaped glands located within the scrotum. These organs are responsible for producing both sperm and testosterone hormone required by males.
From there, matured Sperm cells move on to Epididymis where they undergo maturation .The epididymis is a tightly coiled tube attached to each testicle, and it is here that sperm enters after its production in the testes. The epididymis acts as an incubator, nourishing and bathing them with fluids that help them mature over several weeks until they are ready for ejaculation out into semen.
Next stop – Vas Deferens!. Once fully developed inside epididymis sperm travel through vas deferens tubes.It’s not just one & like 20 muscular watery tubes connect to another duct called Ejaculatory Duct forming thick tube travelling towards ejaculatory process.
Just before entering into prostate gland ejaculatory ducts fuse together creating space for Seminal Vesicles which secrete primarily carbs on which sperms feed.In accordance with this,the next pitstop would be Prostate Gland, secreting watery substance making up almost 30% of semen volume along with seminal vesicle fluid providing additional nutrient-rich material serving as fuel source during their voyage towards goal
Last but not least-Urethra: The moment we’ve all been waiting for – when it finally enters into Urethra.The last leg of their journey is less than an inch long covered by Glans Penis aka the Tip!. And voila! The last push of semen from the urethra results in ejaculation, which marks the end of a sperm’s incredible voyage.
In conclusion, understanding the pathway of sperm from testes to urethra may seem like a trivial matter – but when it comes to reproductive health and fertility, knowledge is power. Knowing how different parts work together can help both men and women protect themselves from sexually transmitted diseases (STDs), infertility issues and other problems related to reproduction. So next time you are on your biology lesson or having a conversation about fertility – remember to appreciate just how amazing this intricate process truly is!
The journey of sperm from the testes to the urethra is an incredibly complex and fascinating process. In this step-by-step guide, we’ll take a closer look at what happens along the pathway and how everything works together to enable reproduction.
Step 1: Production in the Testes
Sperm production starts in the testes – two small, oval-shaped glands located within the scrotum. Testicles are packed with tiny coiled tubes called seminiferous tubules that are responsible for sperm production.
Here, immature sperm cells start to develop into fully matured, fertilization-ready gametes. The process of spermatogenesis takes approximately three months, and newly produced sperm is continuously released into the male reproductive system.
Step 2: Maturation in Epididymis
After leaving the seminiferous tubules, immature sperm cells travel through a network of ducts and then enter a storage area known as the Epididymis; a coiled tube around 20 feet in length that lies on top of each testicle.
In this organ, they undergo maturation and become mobile as they grow tails or flagella to swim towards the female egg. It is also where they develop their capacity for fertilization via interaction with prostatic secretions later during ejaculation
Step 3: Transport Via Vas Deferens
Once maturation is complete, long thin tubes known as Vas deferens begin transporting these matured sperms from both testicles toward prostate gland which lies just beneath urinary bladder
The vas deferens can be described as muscular ducts capable of propelling waves of peristalsis or contraction down its walls pushing sperms forward by rhythmic muscle contractions.
Through an ejaculatory reflex action coming from spinal cord when an orgasm arrives during intercourse or masturbation activity both vas deference will push semen containing products from prostate past vasectomy site out through urethra surrounded by penis shaft
Step 4: Mixing with Seminal Fluids from Prostate and Seminal Vesicles
As sperms travel through vas deferens towards the urethra, they mix with seminal fluids produced by prostate gland and seminal vesicles. These fluids provide a nutrient-rich environment for the sperm cells, providing them with energy to propel themselves forward during ejaculation.
The prostatic secretions contain buffers that neutralize vaginal acidity which would otherwise denature sperm in an acidic environment while also acting as a lubricant to ease transport/movement of semen. The various enzymes within it help keep the tubes free from clots or jams allowing fluid movement required leading up to fertilization process.
In contrast, seminal vesicle contains fructose sugar rich in ATP that helps increase mitochondrial activity while at the same time reserves glycogen stores in order to provide long-term survival energy for sperms
Step 5: Ejaculation Via Urethra
Finally, when all these individual pieces come together, ejaculation occurs – forcing the semen out of penis shaft and through the urethra opening located
The journey of sperm from testes to urethra is quite a fascinating one for people who are interested in the anatomy of the human body. However, even though it is such a crucial process, many people have questions that often remain unanswered. In this blog post, we will address some common FAQs about the pathway of sperm from testes to urethra and provide detailed explanations.
1. What is the pathway followed by sperm as it travels from the testes to the urethra?
Sperm’s journey begins in the seminiferous tubules within each testis in which they are produced. Once they are formed, they travel toward and assemble in epididymal ducts that run alongside each testicle. The sperm maturation process occurs throughout these ducts, and after completion of their development process (approximately 2-4 weeks), they enter vas deferens tubes – muscular ducts that extend from each epididymis region toward the pelvic region where they join with seminal vesicles to form ejaculatory ducts leading towards the prostate gland (where fluids are added before ejaculation) and finally out of the body via urethra tube during ejaculation.
2. What is happening in epididymal duct as sperm mature there?
During this time, sperms gain new features like improved motility – moving more efficiently due to an extra flagellum or even mosaics(carrying two different morphologies stuck together). Additionally, sperms increase glandular secretions inside themselves – special proteins serving at various points along their path through both female reproductive tract environments without being destroyed completely by hostile immune cells intended to protect against infections thereby increasing chances of fertilization once inside a compatible egg,
3. Why do sperm move forward in only one direction?
Aided by peristaltic waves generated inside their vas deferens tissue walls but also needing help crossing areas with opposing directional forces like anti-peristaltic waves (which can result with regurgitation out of urethra tube) or uterine contractions in females. Sperm and their outputs are designed to swim purposefully towards an egg, but also cover a lot of ground faster than potential competitors.
4. Is it possible for sperm to make its way to the egg if they were not ejaculated?
It is highly unlikely, and chances are next to none. Ejaculation delivers millions of sperms into the female reproductive tract at once, stacking the odds in favor of fertilization significantly. A single man’s semen contains only about 200-300 million healthy forward motile sperm cells per milliliter during ejaculation, while typically a woman releases one egg each month approximately on day 14 of her menstrual cycle within an interval window that lasts for up to 24 hours.
5. Can a man lose his ability to produce sperm?
Men who have undergone cancer treatment can experience damage to testes which severely impacts producing enough amount or quality of spermatogenesis capacity levels concerned with male fertility (e.g.,
Let’s begin by understanding how sperm is produced. The production of sperm begins in the testes and continues through a five-stage process called spermatogenesis. Throughout this process, several chemical messengers or hormones play crucial roles that impact how and where sperm travel before reaching their final destination at the urethra.
The pituitary gland located in the brain secretes two essential hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH promotes spermatogenesis and stimulates cells in the testes called Sertoli cells that are necessary for generating viable sperm. These cells are ultimately responsible for pushing mature sperm towards the ducts in the testis’ epididymis.
Next, LH stimulates testosterone production in cells known as Leydig cells found near seminiferous tubules where spermatogenesis occurs. Testosterone is a key male sex hormone responsible for regulating various processes such as fertility, sexual function, body hair growth, muscle mass development among others.
Now here comes an interesting part: After they leave either side of each testicle via many tiny tubes called tubules, immature but fully formed sperm move into larger tubes known as epididymis where they would mature further during storage until ejaculation occurs during sexual intercourse or masturbation.
During ejaculation process, smooth muscles surrounding vas deferens – a tube connecting epididymis with urethra – will contract due to messages from sympathetic neurons closely associated with ejaculatory center located within spinal cord. This results in movement of fluid carrying millions of live sperms into prostatic urethra while dispatching secretions from three different glands namely prostate gland bulbourethral gland, and seminal vesicles. Finally those fluids mix together with sperms and travel to distal urethra.
In conclusion, for sperm to reach their final destination at the urethra, a complex series of events must occur continuously as they travel from the testes through epididymis to vas deferens before joining secretions from accessory glands near their entry point into urethra. The delicate hormonal balance involving FSH, LH along with testosterone levels is what ensures that the pathway stays clear through various anatomical structures so that mature viable sperms can be released during ejaculation.
As we all know, sperm is an essential component of a man’s reproductive system. Without it, fertilization cannot occur, and the dream of starting a family remains out of reach for many couples. Unfortunately, there are several problems that can impact the pathway of sperm from testes to urethra. In this blog post, we will be discussing some common issues associated with this complex process and how they can be addressed for increased male fertility.
One problem that affects sperm transportation is blockage or obstruction in the epididymis, one of the collecting ducts within the testicles where sperm mature and are stored before ejaculation. Blockages may result from infections like sexually transmitted diseases (STDs) or scar tissue formation due to previous surgeries such as vasectomy or hernia repair. When such a blockage occurs, it prevents semen containing the sperm from being ejaculated out through the urethra during orgasm.
Varicocele is another condition that can adversely impact male fertility by restricting blood flow to the testicles’ veins which further results in reducing sperm production as well as motility leading to poor quality sperms.. These swollen veins cause an increase in testicular temperature significant enough to impair normal sperm development .
Other factors including hormonal imbalances affecting spermatogenesis could negatively influence fertility likewise certain treatments like chemotherapy may also cause damage to healthy sperms leading tot loss or reduction in quality/quantity . Similarly prolonged use/addiction of drugs/substances such as tobacco/alcohol supplements would forbid optimal results when seeking conception.
To address these issues and enhance your chances of starting a family, men facing infertility should consider consulting with their healthcare provider regarding potential medical interventions available for their conditions. For instance surgical corrections may help unclog blocked ducts this could include vasectomy reversal surgery , artificial insemination ,medications/drugs ,or even natural remedies /therapies better nutritional supplements like Zinc,Magnesium,selenium have been linked to healthy sperm production.
In conclusion, the pathway of sperm from testes to urethra is prone to several glitches that can significantly impact male fertility. However, by identifying and treating these issues promptly upon diagnosis or decline of fertility, men can enhance their chances for conception and ultimately build the family they have always desired.
The process of impregnation is a fascinating one, and one that involves many intricate biological processes including the movement of sperm along the pathway towards the egg. One important factor in this journey is ejaculation. It has been long touted that ejaculation plays a major role in assisting the movement of sperm towards fertilization, but how exactly does it do this? Let’s examine the role of ejaculation in facilitating the movement of sperm along the pathway.
Firstly, it’s important to understand what ejaculation actually is. Ejaculation is the forceful expulsion of semen from the male reproductive system during sexual activity. Semen consists of various components including spermatozoa (sperm), seminal fluid, and prostatic fluid which all play different roles in facilitating successful impregnation.
So how does ejaculation assist in getting sperm to their final destination? During ejaculation, semen is propelled outwards through contractions of various muscles surrounding the male reproductive organs. This forceful release can provide initial momentum for sperm to begin their journey along the female reproductive tract towards fertilization.
Furthermore, semen contains substances such as fructose (a type of sugar) which provides energy for sperm to move forward. The viscosity (thickness) and pH level (acidity) also help create an environment conducive to sperm survival and motility.
In addition to these physical factors, there are also psychological factors at play during ejaculation that can impact fertility rates. Orgasm and arousal cause a release of hormones such as oxytocin which contribute to feelings of bonding between partners and improve chances for conception through increased sexual frequency.
It’s clear that ejaculation plays a significant role in facilitating the movement of sperm along the pathway towards fertilization. From providing initial propulsion force to nourishing sustenance necessary for survival while traveling through unfamiliar terrain, this process offers crucial support from start-to-finish in order for successfully conception to occur. So next time you go about your intimate activities with your partner(s), you’ll appreciate the powerful role of ejaculation during reproduction, perhaps in ways that you never imagined before.


IMAGES
VIDEO
COMMENTS
Out of the approximately 5,000 sperm that enter the utero-tubal junction, about 1,000 get inside the Fallopian tube. Finally, out of the 1,000 that enter the tube, it is estimated that only 200 make it to the egg. However, in the end, only 1 sperm out of the 200 that reach the egg is able to penetrate and fertilize it.
During this journey through your fallopian tubes, an egg can be fertilized by sperm. Sperm production begins in the testicles of men or people assigned male at birth (AMAB). During ejaculation, millions of sperm cells are set free with the sole purpose of finding an egg to fertilize. ... Conception is the first step, where an egg and sperm join ...
So how does this process work? Let's dive into the intricate pathway of sperm step-by-step. Step 1: Production ... Amongst humans, one of the essential components for reproduction is sperm, responsible for fertilizing an egg. The journey that sperm takes from creation to fertilization is known as the pathway of sperm. It's truly miraculous ...
"The Journey of Sperm and Egg: The Fertilization Process" | Pregnancy | Embryo FormationFertilization is the biological process by which a sperm cell from a ...
Step 3. Journey Through the Cervical Canal The cervical canal is a warm and conducive environment that allows sperm to thrive and push on in their journey. Generously lined with cervical mucus, the canal is tailored for sperm transportation, especially during the fertile window when mucus is at its maximum.Interestingly, the days before ovulation will herald molecular changes that you may ...
Once inside the walls of the fallopian tube, muscle contractions push the egg gently towards the uterus. The egg will either meet sperm on its journey through the fallopian tube and fertilisation will happen, or it will arrive in the uterus unfertilised and be absorbed back into the body. The menstrual cycle. A step-by-step guide to conception
Hundreds of millions of sperm vie for a single egg cell. The sperm cells are streamlined in design for this purpose: a long tail to help them move, lots of mitochondria to power that movement, genetic information to pass on, and enzymatic proteins to get into the egg cell. The proteins are stored in a cap at the front of the sperm known as an acrosome - this is the part that first contacts the ...
Following ovulation, the egg is capable of fertilization for only 12 to 24 hours. Contact between the egg and sperm is random. Once the egg arrives at a specific portion of the tube, called the ampullar-isthmic junction, it rests for another 30 hours. Fertilization — sperm union with the egg — occurs in this portion of the tube.
Surgical removal of the isthmus in the pig leads to increased numbers of sperm entering the ampulla and polyspermy in about one-third of eggs , suggesting that the isthmic portion of the female reproductive tract regulates the number of fertilization-competent sperm that reach the egg in vivo. This control step is bypassed by IVF, which usually ...
The first step in this journey begins when sperm cells are released from the testes. They enter into a part of the male reproductive system known as the epididymis where they mature over several weeks before being released during ejaculation. ... It represents the merging of two cells, the sperm and the egg, which leads to a new life. This ...
Step-by-Step Guide: Unraveling the Pathway of Sperm . Welcome to our comprehensive step-by-step guide, where we unravel the intricate and fascinating pathway of sperm. Prepare yourself for a journey through the world of reproductive biology, as we delve deep into the intricacies of this tiny yet incredibly crucial component of human life.
During the journey, ... This step completes the process of fertilization and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human. ... Next, the eggs and sperm are mixed in a petri dish. The ideal ratio is 75,000 sperm to one egg. If there are severe problems with the sperm—for example ...
In this step, plenty of sperms die during approaching to the target. Meet the egg. Once sperms (that still survive) reach the fallopian tubes, they will meet 1 fully matured egg which has passed the ovulation then moved to wait for sperm at the fallopian tubes. Each sperm will be approaching to this egg consequently. Fertilization
Fertilization is a complex multi-step process that is complete in 24 hours. The sperm from a male meets an ovum from a female and forms a zygote; this is the point in which pregnancy begins and leads to a 280-day journey for a female. There are two ways to track this process, and they differ by the day counting begins. There are the post-ovulation age and the gestational age, calculated by ...
The journey of sperm is an incredible tale of resilience, strategy, and determination. ... just one exceptional sperm can penetrate and fuse with the egg's protective outer layer through specific receptors on its head. This extraordinary event marks fertilization—a profound union of genetic material from both parents. ... Step 6: Sperm ...
Unite sperm and eggs. Now comes the part of IVF that everyone's the most familiar with — combining the best sperm with your best eggs. This stage is called insemination. It usually takes a few hours for a sperm to fertilize an egg. Your doctor may also inject the sperm directly into the egg instead, a process known as intracytoplasmic sperm ...
The journey of sperm begins inside the testicles. Males begin to produce sperm at the start of puberty at around 12 or 13 years old. It is a process that requires a slightly cooler temperature, which is why testicles hang outside men's bodies. Nor is it a quick process: the production of sperm takes about 70 days.
This shortens the distance the sperm travels to reach the fallopian tubes, increasing the likelihood that one sperm will meet and fertilize the egg. IUI procedure step by step The IUI procedure ...
Step 1: Production. Sperm production starts at the testicles, where millions of them are produced every day. It takes about 74 days for the male body to produce fully mature and functional sperm. Step 2: Maturation. After being produced in the testicles, immature sperm travel through a tube called the epididymis.
donatemyeggsMarch 21, 2024 on : "Your egg donation journey, step by step. ️ Swipe to learn more! #EggDonationBenefits #GrowFamilies #eggdonation #eggdonor #eggdono..." Your egg donation journey, step by step. 🛣️ Swipe to learn more!
Step 2: Maturation. After production, the sperm cells begin their journey through various ducts within the male reproductive system where they mature and gain mobility. It takes about 10-14 days for the average sperm to fully mature into a swimming machine. Step 3: Storage.
The Step-by-Step Guide to the Pathway of Sperm from Testes to Urethra . The journey of sperm from the testes to the urethra is an incredibly complex and fascinating process. In this step-by-step guide, we'll take a closer look at what happens along the pathway and how everything works together to enable reproduction.