#PrepYourHealth: Tips for Holiday Travel

Holiday travel often includes visiting loved ones or taking a vacation. Whether you’re seeking a winter wonderland or an escape from subzero temperatures, follow these travel tips to stay healthy and safe during the holiday travel season.

Before Your Trip
No matter where you plan to travel, check CDC’s destination pages for travel health information . These pages include information about
- vaccines and medicines you may need, and
- diseases or health risks that are a concern at your destination.
Get up to date with your COVID-19 vaccines and seasonal flu vaccine. CDC recommends getting the flu vaccine every year.
Get up to date on routine vaccines. Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are uncommon in the United States but common in other countries.
Prepare a travel health kit that includes personal needs, especially those items that may be difficult to find at your destination. Take enough of your prescription and over-the-counter medicines to last your entire trip, plus extra in case of travel delays. You may also want to pack insect repellent , sunscreen (SPF 15 or higher), aloe, alcohol-based hand sanitizer, water disinfection tablets, and important paperwork like your health insurance card.
Make sure you have a plan for getting health care during travel . Find out if your health insurance covers medical care abroad. Travelers are usually responsible for paying hospital and other medical expenses out of pocket at most destinations. Consider buying additional insurance that covers health care and emergency evacuation, especially if you will travel to remote areas.
During Your Trip
Choose safe transportation. Always wear your seat belt. If you are traveling with children ages 12 and younger, make sure they are properly buckled in a car seat, booster seat, or seat belt—whichever is appropriate for their age, weight, and height—in the back seat.
Motor vehicle crashes are the leading cause of death among healthy travelers. Be alert when crossing the street, especially in countries where people drive on the left side of the road. Find out other steps you can take to stay safe on the roads.
Protect yourself from the sun. Apply sunscreen with SPF 15 or higher when traveling. Protecting yourself from the sun isn’t just for tropical beaches. You can sunburn even if it’s cloudy or cold. You are at the highest risk for ultraviolet light exposure during summer months, near the equator, at high altitudes, and between 10 a.m. to 4 p.m.
Stay alert in crowded areas. Does your holiday travel involve markets, festivals, or other activities that involve a large number of people at the same place (mass gathering)? If so, learn some tips to stay safe at a mass gathering.
Considerations for cold weather travel
Wear warm clothing in several loose layers when traveling in cold weather or climates. Learn practical skills and lessons like how to prevent hypothermia and frostbite .
Considerations for warm weather travel
If you are traveling in hot weather or to a hot climate, wear loose, lightweight, light-colored clothing.
Your chances of getting heat stroke, heat exhaustion, or other heat-related illness during travel depend on your destination, activities, level of hydration, and age. The more active you are in high temperatures, the more likely you are to get a heat-related illness. Learn how to prevent heat-related illness .
Use insect repellent and take steps to avoid bug bites. Bugs, including mosquitoes, ticks, and flies, can spread diseases such as Zika, dengue, Lyme, and others. These bugs are typically more active during warm weather. Check your destination’s page to determine what you need to do to protect yourself from diseases spread through bug bites, including medications or vaccines when recommended.
After Your Trip
If you recently traveled and feel sick , particularly if you have a fever, talk to a healthcare professional. Tell them about your travel. Be prepared to answer questions about your vaccination history, destination(s), reasons for traveling, itinerary, and other aspects of your trip.
- Travelers’ Health | CDC
- Traveler Advice | Travelers’ Health | CDC
- COVID-19: International Travel to and from the United States | CDC
- Cruise Ship Travel During COVID-19| CDC
Thanks in advance for your questions and comments on this Public Health Matters post. Please note that CDC does not give personal medical advice. If you are concerned you have a disease or condition, talk to your doctor.
Have a question for CDC? CDC-INFO ( http://www.cdc.gov/cdc-info/index.html ) offers live agents by phone and email to help you find the latest, reliable, and science-based health information on more than 750 health topics.
Post a Comment
Your email address will not be published. Required fields are marked *
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Fact Sheets
Frequently Asked Questions: Guidance for Travelers to Enter the U.S.
Updated Date: April 21, 2022
Since January 22, 2022, DHS has required non-U.S. individuals seeking to enter the United States via land ports of entry and ferry terminals at the U.S.-Mexico and U.S.-Canada borders to be fully vaccinated for COVID-19 and provide proof of vaccination upon request. On April 21, 2022, DHS announced that it would extend these requirements. In determining whether and when to rescind this order, DHS anticipates that it will take account of whether the vaccination requirement for non-U.S. air travelers remains in place.
These requirements apply to non-U.S. individuals who are traveling for essential or non-essential reasons. They do not apply to U.S. citizens, Lawful Permanent Residents, or U.S. nationals.
Effective November 8, 2021, new air travel requirements applied to many noncitizens who are visiting the United States temporarily. These travelers are also required to show proof of COVID-19 vaccination. All air travelers, including U.S. persons, must test negative for COVID-19 prior to departure. Limited exceptions apply. See CDC guidance for more details regarding air travel requirements.
Below is more information about what to know before you go, and answers to Frequently Asked Questions about cross-border travel.
Entering the U.S. Through a Land Port of Entry or Ferry Terminal
Q. what are the requirements for travelers entering the united states through land poes.
A: Before embarking on a trip to the United States, non-U.S. travelers should be prepared for the following:
- Possess proof of an approved COVID-19 vaccination as outlined on the CDC website.
- During border inspection, verbally attest to their COVID-19 vaccination status.
- Bring a Western Hemisphere Travel Initiative compliant border crossing document, such as a valid passport (and visa if required), Trusted Traveler Program card, a Department of State-issued Border Crossing Card, Enhanced Driver’s License or Enhanced Tribal Card when entering the country. Travelers (including U.S. citizens) should be prepared to present the WHTI-compliant document and any other documents requested by the CBP officer.
Q. What are the requirements to enter the United States for children under the age of 18 who can't be vaccinated?
A: Children under 18 years of age are excepted from the vaccination requirement at land and ferry POEs.
Q: Which vaccines/combination of vaccines will be accepted?
A: Per CDC guidelines, all Food and Drug Administration (FDA) approved and authorized vaccines, as well as all vaccines that have an Emergency Use Listing (EUL) from the World Health Organization (WHO), will be accepted.
Accepted Vaccines:
- More details are available in CDC guidance here .
- 2 weeks (14 days) after your dose of an accepted single-dose COVID-19 vaccine;
- 2 weeks (14 days) after your second dose of an accepted 2-dose series;
- 2 weeks (14 days) after you received the full series of an accepted COVID-19 vaccine (not placebo) in a clinical trial;
- 2 weeks (14 days) after you received 2 doses of any “mix-and-match” combination of accepted COVID-19 vaccines administered at least 17 days apart.
Q. Is the United States requiring travelers to have a booster dose to be considered fully vaccinated for border entry purposes?
A: No. The CDC guidance for “full vaccination” can be found here.
Q: Do U.S. citizens or lawful permanent residents need proof of vaccination to return to the United States via land POEs and ferry terminals?
A: No. Vaccination requirements do not apply to U.S. citizens, U.S. nationals, or Lawful Permanent Residents (LPRs). Travelers that exhibit signs or symptoms of illness will be referred to CDC for additional medical evaluation.
Q: Is pre- or at-arrival COVID testing required to enter the United States via land POEs or ferry terminals?
A: No, there is no COVID testing requirement to enter the United States via land POE or ferry terminals. In this respect, the requirement for entering by a land POE or ferry terminal differs from arrival via air, where there is a requirement to have a negative test result before departure.
Processing Changes Announced on January 22, 2022
Q: new changes were recently announced. what changed on january 22.
A: Since January 22, 2022, non-citizens who are not U.S. nationals or Lawful Permanent Residents have been required to be vaccinated against COVID-19 to enter the United States at land ports of entry and ferry terminals, whether for essential or nonessential purposes. Previously, DHS required that non-U.S. persons be vaccinated against COVID-19 to enter the United States for nonessential purposes. Effective January 22, all non-U.S. individuals, to include essential travelers, must be prepared to attest to vaccination status and present proof of vaccination to a CBP officer upon request. DHS announced an extension of this policy on April 21, 2022.
Q: Who is affected by the changes announced on January 22?
A: This requirement does not apply to U.S. citizens, U.S. nationals, or U.S. Lawful Permanent Residents. It applies to other noncitizens, such as a citizen of Mexico, Canada, or any other country seeking to enter the United States through a land port of entry or ferry terminal.
Q: Do U.S. citizens need proof of vaccination to return to the United States via land port of entry or ferry terminals?
A: Vaccination requirements do not apply to U.S. Citizens, U.S. nationals or U.S. Lawful Permanent Residents. Travelers that exhibit signs or symptoms of illness will be referred to CDC for additional medical evaluation.
Q: What is essential travel?
A: Under the prior policy, there was an exception from temporary travel restrictions for “essential travel.” Essential travel included travel to attend educational institutions, travel to work in the United States, travel for emergency response and public health purposes, and travel for lawful cross-border trade (e.g., commercial truckers). Under current policy, there is no exception for essential travel.
Q: Will there be any exemptions?
A: While most non-U.S. individuals seeking to enter the United States will need to be vaccinated, there is a narrow list of exemptions consistent with the Centers for Disease Control and Prevention (CDC) Order in the air travel context.
- Certain categories of individuals on diplomatic or official foreign government travel as specified in the CDC Order
- Children under 18 years of age;
- Certain participants in certain COVID-19 vaccine trials as specified in the CDC Order;
- Individuals with medical contraindications to receiving a COVID-19 vaccine as specified in the CDC Order;
- Individuals issued a humanitarian or emergency exception by the Secretary of Homeland Security;
- Individuals with valid nonimmigrant visas (excluding B-1 [business] or B-2 [tourism] visas) who are citizens of a country with limited COVID-19 vaccine availability, as specified in the CDC Order
- Members of the U.S. Armed Forces or their spouses or children (under 18 years of age) as specified in the CDC Order; and
- Individuals whose entry would be in the U.S. national interest, as determined by the Secretary of Homeland Security.
Q: What documentation will be required to show vaccination status?
A: Non-U.S. individuals are required to be prepared to attest to vaccination status and present proof of vaccination to a CBP officer upon request regardless of the purpose of travel.
The current documentation requirement remains the same and is available on the CDC website . Documentation requirements for entry at land ports of entry and ferry terminals mirror those for entry by air.
Q: What happens if someone doesn’t have proof of vaccine status?
A: If non-U.S. individuals cannot present proof of vaccination upon request, they will not be admitted into the United States and will either be subject to removal or be allowed to withdraw their application for entry.
Q: Will incoming travelers be required to present COVID-19 test results?
A: There is no COVID-19 testing requirement for travelers at land border ports of entry, including ferry terminals.
Q: What does this mean for those who can't be vaccinated, either due to age or other health considerations?
A: See CDC guidance for additional information on this topic. Note that the vaccine requirement does not apply to children under 18 years of age.
Q: Does this requirement apply to amateur and professional athletes?
A: Yes, unless they qualify for one of the narrow CDC exemptions.
Q: Are commercial truckers required to be vaccinated?
A: Yes, unless they qualify for one of the narrow CDC exemptions. These requirements also apply to bus drivers as well as rail and ferry operators.
Q. Do you expect border wait times to increase?
A: As travelers navigate these new travel requirements, wait times may increase. Travelers should account for the possibility of longer than normal wait times and lines at U.S. land border crossings when planning their trip and are kindly encouraged to exercise patience.
To help reduce wait times and long lines, travelers can take advantage of innovative technology, such as facial biometrics and the CBP OneTM mobile application, which serves as a single portal for individuals to access CBP mobile applications and services.
Q: How is Customs and Border Protection staffing the ports of entry?
A: CBP’s current staffing levels at ports of entry throughout the United States are commensurate with pre-pandemic levels. CBP has continued to hire and train new employees throughout the pandemic. CBP expects some travelers to be non-compliant with the proof of vaccination requirements, which may at times lead to an increase in border wait times. Although trade and travel facilitation remain a priority, we cannot compromise national security, which is our primary mission. CBP Office of Field Operations will continue to dedicate its finite resources to the processing of arriving traffic with emphasis on trade facilitation to ensure economic recovery.
Q: What happens if a vaccinated individual is traveling with an unvaccinated individual?
A: The unvaccinated individual (if 18 or over) would not be eligible for admission.
Q: If I am traveling for an essential reason but am not vaccinated can I still enter?
A: No, if you are a non-U.S. individual. The policy announced on January 22, 2022 applies to both essential and non-essential travel by non-U.S. individual travelers. Since January 22, DHS has required that all inbound non-U.S. individuals crossing U.S. land or ferry POEs – whether for essential or non-essential reasons – be fully vaccinated for COVID-19 and provide related proof of vaccination upon request.
Q: Are sea crew members on vessels required to have a COVID vaccine to disembark?
A: Sea crew members traveling pursuant to a C-1 or D nonimmigrant visa are not excepted from COVID-19 vaccine requirements at the land border. This is a difference from the international air transportation context.
Entering the U.S. via Air Travel
Q: what are the covid vaccination requirements for air passengers to the united states .
A: According to CDC requirements [www.cdc.gov/coronavirus/2019-ncov/travelers/noncitizens-US-air-travel.html | Link no longer valid], most noncitizens who are visiting the United States temporarily must be fully vaccinated prior to boarding a flight to the United States. These travelers are required to show proof of vaccination. A list of covered individuals is available on the CDC website.
Q: What are the COVID testing requirements for air passengers to the United States?
A: Effective Sunday, June 12 at 12:01 a.m. ET, CDC will no longer require pre-departure COVID-19 testing for U.S.-bound air travelers.
- Border Security
- Transportation Security
- Airport Security
- Coronavirus (COVID-19)
- Customs and Border Protection (CBP)
- Transportation Security Administration (TSA)
- COVID-19 travel advice
Considering travel during the pandemic? Take precautions to protect yourself from COVID-19.
A coronavirus disease 2019 (COVID-19) vaccine can prevent you from getting COVID-19 or from becoming seriously ill due to COVID-19 . But even if you're vaccinated, it's still a good idea to take precautions to protect yourself and others while traveling during the COVID-19 pandemic.
If you've had all recommended COVID-19 vaccine doses, including boosters, you're less likely to become seriously ill or spread COVID-19 . You can then travel more safely within the U.S. and internationally. But international travel can still increase your risk of getting new COVID-19 variants.
The Centers for Disease Control and Prevention (CDC) recommends that you should avoid travel until you've had all recommended COVID-19 vaccine and booster doses.
Before you travel
As you think about making travel plans, consider these questions:
- Have you been vaccinated against COVID-19 ? If you haven't, get vaccinated. If the vaccine requires two doses, wait two weeks after getting your second vaccine dose to travel. If the vaccine requires one dose, wait two weeks after getting the vaccine to travel. It takes time for your body to build protection after any vaccination.
- Have you had any booster doses? Having all recommended COVID-19 vaccine doses, including boosters, increases your protection from serious illness.
- Are you at increased risk for severe illness? Anyone can get COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness from COVID-19 .
- Do you live with someone who's at increased risk for severe illness? If you get infected while traveling, you can spread the COVID-19 virus to the people you live with when you return, even if you don't have symptoms.
- Does your home or destination have requirements or restrictions for travelers? Even if you've had all recommended vaccine doses, you must follow local, state and federal testing and travel rules.
Check local requirements, restrictions and situations
Some state, local and territorial governments have requirements, such as requiring people to wear masks, get tested, be vaccinated or stay isolated for a period of time after arrival. Before you go, check for requirements at your destination and anywhere you might stop along the way.
Keep in mind these can change often and quickly depending on local conditions. It's also important to understand that the COVID-19 situation, such as the level of spread and presence of variants, varies in each country. Check back for updates as your trip gets closer.
Travel and testing
For vaccinated people.
If you have been fully vaccinated, the CDC states that you don't need to get tested before or after your trip within the U.S. or stay home (quarantine) after you return.
If you're planning to travel internationally outside the U.S., the CDC states you don't need to get tested before your trip unless it's required at your destination. Before arriving to the U.S., you need a negative test within the last day before your arrival or a record of recovery from COVID-19 in the last three months.
After you arrive in the U.S., the CDC recommends getting tested with a viral test 3 to 5 days after your trip. If you're traveling to the U.S. and you aren't a citizen, you need to be fully vaccinated and have proof of vaccination.
You don't need to quarantine when you arrive in the U.S. But check for any symptoms. Stay at home if you develop symptoms.
For unvaccinated people
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19 . If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
Repeat the test 3 to 5 days after your trip. Stay home for five days after travel.
If at any point you test positive for the virus that causes COVID-19 , stay home. Stay at home and away from others if you develop symptoms. Follow public health recommendations.
Stay safe when you travel
In the U.S., you must wear a face mask on planes, buses, trains and other forms of public transportation. The mask must fit snugly and cover both your mouth and nose.
Follow these steps to protect yourself and others when you travel:
- Get vaccinated.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness.
- Avoid contact with anyone who is sick or has symptoms.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Don't touch frequently touched surfaces, such as handrails, elevator buttons and kiosks. If you must touch these surfaces, use hand sanitizer or wash your hands afterward.
- Wear a face mask in indoor public spaces. The CDC recommends wearing the most protective mask possible that you'll wear regularly and that fits. If you are in an area with a high number of new COVID-19 cases, wear a mask in indoor public places and outdoors in crowded areas or when you're in close contact with people who aren't vaccinated.
- Avoid touching your eyes, nose and mouth.
- Cover coughs and sneezes.
- Wash your hands often with soap and water for at least 20 seconds.
- If soap and water aren't available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub your hands together until they feel dry.
- Don't eat or drink on public transportation. That way you can keep your mask on the whole time.
Because of the high air flow and air filter efficiency on airplanes, most viruses such as the COVID-19 virus don't spread easily on flights. Wearing masks on planes has likely helped lower the risk of getting the COVID-19 virus on flights too.
However, air travel involves spending time in security lines and airport terminals, which can bring you in close contact with other people. Getting vaccinated and wearing a mask when traveling can help protect you from COVID-19 while traveling.
The Transportation Security Administration (TSA) has increased cleaning and disinfecting of surfaces and equipment, including bins, at screening checkpoints. TSA has also made changes to the screening process:
- Travelers must wear masks during screening. However, TSA employees may ask travelers to adjust masks for identification purposes.
- Travelers should keep a distance of 6 feet apart from other travelers when possible.
- Instead of handing boarding passes to TSA officers, travelers should place passes (paper or electronic) directly on the scanner and then hold them up for inspection.
- Each traveler may have one container of hand sanitizer up to 12 ounces (about 350 milliliters) in a carry-on bag. These containers will need to be taken out for screening.
- Personal items such as keys, wallets and phones should be placed in carry-on bags instead of bins. This reduces the handling of these items during screening.
- Food items should be carried in a plastic bag and placed in a bin for screening. Separating food from carry-on bags lessens the likelihood that screeners will need to open bags for inspection.
Be sure to wash your hands with soap and water for at least 20 seconds directly before and after going through screening.
Public transportation
If you travel by bus or train and you aren't vaccinated, be aware that sitting or standing within 6 feet (2 meters) of others for a long period can put you at higher risk of getting or spreading COVID-19 . Follow the precautions described above for protecting yourself during travel.
Even if you fly, you may need transportation once you arrive at your destination. You can search car rental options and their cleaning policies on the internet. If you plan to stay at a hotel, check into shuttle service availability.
If you'll be using public transportation and you aren't vaccinated, continue physical distancing and wearing a mask after reaching your destination.
Hotels and other lodging
The hotel industry knows that travelers are concerned about COVID-19 and safety. Check any major hotel's website for information about how it's protecting guests and staff. Some best practices include:
- Enhanced cleaning procedures
- Physical distancing recommendations indoors for people who aren't vaccinated
- Mask-wearing and regular hand-washing by staff
- Mask-wearing indoors for guests in public places in areas that have high cases of COVID-19
- Vaccine recommendations for staff
- Isolation and testing guidelines for staff who've been exposed to COVID-19
- Contactless payment
- Set of rules in case a guest becomes ill, such as closing the room for cleaning and disinfecting
- Indoor air quality measures, such as regular system and air filter maintenance, and suggestions to add air cleaners that can filter viruses and bacteria from the air
Vacation rentals, too, are enhancing their cleaning procedures. They're committed to following public health guidelines, such as using masks and gloves when cleaning, and building in a waiting period between guests.
Make a packing list
When it's time to pack for your trip, grab any medications you may need on your trip and these essential safe-travel supplies:
- Alcohol-based hand sanitizer (at least 60% alcohol)
- Disinfectant wipes (at least 70% alcohol)
- Thermometer
Considerations for people at increased risk
Anyone can get very ill from the virus that causes COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness. This may include people with cancer, serious heart problems and a weakened immune system. Getting the recommended COVID-19 vaccine and booster doses can help lower your risk of being severely ill from COVID-19 .
Travel increases your chance of getting and spreading COVID-19 . If you're unvaccinated, staying home is the best way to protect yourself and others from COVID-19 . If you must travel and aren't vaccinated, talk with your health care provider and ask about any additional precautions you may need to take.
Remember safety first
Even the most detailed and organized plans may need to be set aside when someone gets ill. Stay home if you or any of your travel companions:
- Have signs or symptoms, are sick or think you have COVID-19
- Are waiting for results of a COVID-19 test
- Have been diagnosed with COVID-19
- Have had close contact with someone with COVID-19 in the past five days and you're not up to date with your COVID-19 vaccines
If you've had close contact with someone with COVID-19 , get tested after at least five days. Wait to travel until you have a negative test. Wear a mask if you travel up to 10 days after you've had close contact with someone with COVID-19 .
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Feb. 4, 2022.
- Domestic travel during COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html. Accessed Feb. 4, 2022.
- Requirement for face masks on public transportation conveyances and at transportation hubs. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html. Accessed Feb. 4, 2022.
- International travel. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel/index.html. Accessed Feb. 4, 2022.
- U.S citizens, U.S. nationals, U.S. lawful permanent residents, and immigrants: Travel to and from the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html. Accessed Feb. 4, 2022.
- Non-US. citizen, non-U.S. immigrants: Air travel to the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/noncitizens-US-air-travel.html. Accessed Feb. 4, 2022.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Feb. 4, 2022.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Feb. 4, 2022.
- Pack smart. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/pack-smart. Accessed Feb. 4, 2022.
- Travel: Frequently asked questions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/faqs.html. Accessed Feb. 7, 2022.
- Coronavirus (COVID-19) information. Transportation Security Administration. https://www.tsa.gov/coronavirus. Accessed Feb. 7, 2022.
- WHO advice for international traffic in relation to the SARS-CoV-2 Omicron variant (B.1.1.529). World Health Organization. https://www.who.int/news-room/articles-detail/who-advice-for-international-traffic-in-relation-to-the-sars-cov-2-omicron-variant. Accessed Feb. 7, 2022.
- VRHP/VRMA Cleaning guidelines for COVID-19. Vacation Rental Management Association. https://www.vrma.org/page/vrhp/vrma-cleaning-guidelines-for-covid-19. Accessed Feb. 7, 2022.
- Safe stay. American Hotel & Lodging Association. https://www.ahla.com/safestay. Accessed Feb. 7, 2022.
- Khatib AN, et al. COVID-19 transmission and the safety of air travel during the pandemic: A scoping review. Current Opinion in Infectious Diseases. 2021; doi:10.1097/QCO.0000000000000771.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
U.S. travel resources
- Check CDC recommendations for travel within the U.S.
- Review testing requirements for travel to the U.S.
- Look up restrictions at your destination .
- Review airport security measures .
Related resources
Make twice the impact.
Your gift can go twice as far to advance cancer research and care!
Update April 12, 2024
Information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents, before you go.
Learn About Your Destination
While Abroad
Emergencies
Share this page:
Crisis and Disaster Abroad: Be Ready
What the Department of State Can and Can't Do in a Crisis
Information for U.S. Citizens about a U.S. Government-Assisted Evacuation
Traveler's Checklist
Safety and Security Messaging
Best Practices for Traveler Safety
Staying Connected
Smart Traveler Enrollment Program (STEP)
Traveler Information
LGBTQI+ Travelers
Adventure Travel
High-Risk Area Travelers
Travelers with Dual Nationality
Journalist Travelers
Faith-Based Travelers
Pilgrimage Travelers (Hajj and Umrah)
U.S. Students Abroad
Cruise Ship Passengers
Women Travelers
Travelers with Disabilities
Older Travelers
U.S. Volunteers Abroad
Travelers with Pets
Travelers With Firearms
Travel Agents
Travel Safety - Race and Ethnicity
U.S. Travelers in Europe's Schengen Area
Your Health Abroad
Insurance Coverage Overseas
Driving and Road Safety Abroad
Customs and Import Restrictions
Information for U.S. Citizens in Russia – Travel Options Out of Russia
Lodging Safety
Get Help with a Medical Emergency Abroad
If you or a U.S. citizen loved one become seriously ill or injured abroad, we can:
- Help locate appropriate medical services.
- Inform your family or friends, with your permission.
- Help transfer funds to U.S. citizens overseas.
The U.S. government does not pay overseas medical bills. The patient must pay all hospital and other expenses.
You can find lists of doctors and hospitals in the country you are visiting. Check the website of the U.S. embassy in the country you are visiting.
Check Your Health Insurance – Are You Covered Abroad?
Understand what medical services your health insurance will cover overseas before traveling. Carry your insurance card and a claim form if your policy covers you outside the United States.
Medicare does not cover medical care when you travel the United States. Visit Medicare.gov for more information.
Some health insurance companies pay for “customary and reasonable” hospital costs abroad. Very few pay for your medical evacuation back to the United States. The cost may exceed $250,000, depending on your location and medical condition. Consider buying medical evacuation insurance. For more information, visit our webpage on Insurance Coverage Overseas .
Traveling with Prescription Medications
- Check with the foreign embassy of the country you are visiting or passing through. Check to make sure your medications are allowed, particularly prescriptions for medical marijuana. You may need an import license or permit to travel with certain medications.
- Bring plenty of medicine for your trip. If possible, bring a few extra days’ worth in case of delays. You might not be able to get the same medication abroad.
- Carry a letter from the doctor. It should describe your medical condition. It should also list any prescription drugs and their generic names.
- Keep medications in their original, labeled containers.
- Entering a country with a prescription medication, even if legally obtained in the United States, could be illegal and result in your detention or arrest overseas.
Medical Tourism Abroad
Between 150,000 and 320,000 U.S. citizens travel abroad for medical care each year. Medical tourism includes cosmetic surgery, dentistry, and other surgical procedures.
If you are a U.S. citizen considering travel abroad for medical care, you should:
- Verify the doctor’s training, qualifications, and reputation.
- Visit the U.S. Centers for Disease Control and Prevention (CDC) Medical Tourism website for more information on medical tourism.
- Check country information for more information.

Inform Yourself About Vaccinations
Some Countries Require Vaccinations
Before you travel, check country information . You may need to carry an International Certificate of Vaccination, also called a Yellow Card. You may also need to show proof of other inoculations or medical tests. Check also current requirements directly with the foreign embassies of the countries you are visiting.
Recommended Vaccinations and Malaria Prevention
Check the U.S. Centers for Disease Control (CDC) and World Health Organization (WHO) websites for recommended vaccinations and malaria prevention for your destination. Review the CDC’s webpage on Choosing a Drug to Prevent Malaria .
Travel Smartly with Prescription Medications
- Bring an ample supply of medication to cover you for your trip, and if possible, a few extra days in case there are delays.
- Carry a letter from the attending physician that describes your medical condition and any prescription medications, including the generic name of prescribed drugs.
- Check with the foreign embassy of the country you are visiting or transiting to make sure your medications are permitted in that country. Some countries require an import license or permit to travel with certain medications.
Being Prepared for a Pandemic
Review the U.S. Centers for Disease Control and Prevention website for information about pandemics. In a pandemic, virus control measures could affect your travel:
- Travel restrictions may prevent U.S. citizens from traveling internationally.
- Foreign governments may close borders suddenly or with little advance warning.
- Commercial air, land, and sea carriers could suspend some or all transportation services.
- Some countries may quarantine people who appear sick or test positive with the virus.
These developments could delay your travel or your return to the United States.
Other Health Considerations Abroad
- Review the CDC’s Traveler Advice.
- Review Traveling With Disabilities .
- Review Considerations for Older Travelers .
Enroll in STEP

Subscribe to get up-to-date safety and security information and help us reach you in an emergency abroad.
Recommended Web Browsers: Microsoft Edge or Google Chrome.
Learn about your destination
Make two copies of all of your travel documents in case of emergency, and leave one with a trusted friend or relative.
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
An official website of the United States government Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Frequently Asked Questions
⚠ The COVID-19 Public Health Emergency expired as of May 11, 2023. This site will no longer be updated and will remain online for historical purposes only.
For current COVID-19 guidance, please visit the Centers for Disease Control and Prevention (CDC) .

- Can I wear a mask to the TSA checkpoint? Yes, CDC recommends travelers wear a mask throughout their travel journey. Travelers may be asked to adjust their mask for identity verification or remove it briefly if it alarms the security screening equipment.
Can I request that TSA officers use new gloves during my screening? Yes. TSA officers are required to wear nitrile gloves when conducting screening duties and to change them following each pat-down and upon passenger request.
Can I bring my own filled water bottle through the TSA checkpoint? No, you are not permitted to bring your own filled water bottle that exceeds 3.4 ounces through the checkpoint. Many airports now offer touchless refilling stations past security that enable travelers to fill empty bottles and containers they bring from home. Consult the directory or ask a local official for locations in your departure airport.
Do I need to remove electronics from my carry-on bags?
Yes, you should plan to remove personal electronic devices larger than a cell phone from your carry-on bag and put them in a separate bin with nothing placed on or under them for security screening. (This does not apply to TSA PreCheck™ passengers.) Some airports are using new Computed Tomography (CT) technology that allows you to keep electronics in your carry-on luggage. Passengers will be advised on the use of CT scanners at the checkpoint and of any alternate procedures.
Can TSA still open and go through my checked luggage? What precautions are being taken to reduce possible contamination? Yes, TSA may inspect your checked baggage during the screening process. If your property is physically inspected, TSA will place a notice of baggage inspection inside your bag. To reduce the likelihood of contamination, TSA officers are changing their gloves after each bag check and conducting enhanced sanitation of baggage screening areas.
What is the status of REAL ID enforcement in light of COVID-19?
The Department of Homeland Security has extended the deadline for REAL ID enforcement to May 7, 2025. Visit the REAL ID website for more information.
What happens if a passenger is unruly and does not comply with an airline’s policies and/or causes an inflight disruption or distraction for the crew?
Federal law prohibits physically assaulting or threatening to physically assault aircraft crew or anyone else on a civil aircraft. Passengers are subject to civil penalties for such misconduct, which can threaten the safety of the flight by disrupting or distracting cabin crew from their safety duties. Additionally, federal law provides for criminal fines and imprisonment of passengers who interfere with the performance of a crewmember’s duties by assaulting or intimidating that crewmember.
What happens if there is a sick passenger on an international or domestic flight?
Under current federal regulations, pilots must report all onboard illnesses and deaths to CDC before arriving to a U.S. destination. According to CDC illness response protocols, if a sick traveler has a serious contagious disease during air travel, CDC works with local and state health departments and international public health agencies to contact exposed passengers and crew. Be sure to give the airline your current contact information when booking your ticket so you can be notified if you are exposed to a sick traveler on a flight. For more information, see the CDC web page Protecting Travelers’ Health from Airport to Community: Investigating Contagious Diseases on Flights .
Can flying on an airplane increase my risk of getting COVID-19?
Most airlines and airports are enhancing their cleaning and passenger health protection protocols due to COVID-19, but air travel requires spending time in security lines and airport terminals, which can bring you in close contact with other people and frequently touched surfaces. This may increase your risk for exposure to the virus that causes COVID-19.
Most viruses and other germs do not spread easily on flights because of how air circulates and is filtered on airplanes (the air in an airplane cabin is fully renewed every 2-3 minutes, which is more frequent than most other locations in which people spend time). However, social distancing is difficult on flights, and you may have to sit near others, sometimes for hours. This is why CDC recommends the wearing of a face mask an important additional measure against exposing yourself or others to COVID-19. It is important to follow basic guidance on wearing a face mask and frequently washing your hands or using hand sanitizer with at least 60% alcohol. For more information see CDC’s Travel During the COVID-19 Pandemic .
International Travel Requirements
- What should passengers provide to airlines to show they are fully vaccinated? Both U.S. citizens and foreign nationals who are fully vaccinated should travel with proof of their vaccination status to provide to their airline prior to departure to the United States. That proof of vaccination should be a paper or digital record issued by an official source and should include the traveler’s name and date of birth, as well as the vaccine product and date(s) of administration for all doses the traveler received.
- How does the exemption from full vaccination for children work? Children under 18 are exempted from the vaccination requirement for foreign national travelers, given both the ineligibility of some younger children for vaccination, as well as the global variability in access to vaccination for older children who are eligible to be vaccinated.
- How is the United States government determining exceptions to the vaccination requirement for foreign nationals? The presidential proclamation and CDC order include a very limited set of exceptions from the vaccination requirement for foreign nationals. These include exceptions for children, certain COVID-19 vaccine clinical trial participants, those with rare medical contraindications to the vaccines, those who need to travel for emergency or humanitarian reasons, those who are traveling on non-tourist visas from countries with low-vaccine availability, members of the armed forces and their immediate families, airline crew, ship crew, and diplomats.
*All information developed in accordance with CDC guidelines.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 5 - Melioidosis
- Section 5 - Pertussis / Whooping Cough
Meningococcal Disease
Cdc yellow book 2024.
Author(s): Lucy McNamara, Amy Blain
Infectious Agent
Transmission, epidemiology, clinical presentation.
INFECTIOUS AGENT: Neisseria meningitidis
Worldwide, but greatest incidence occurs in the meningitis belt of Africa (see Map 5-01 )
TRAVELER CATEGORIES AT GREATEST RISK FOR EXPOSURE & INFECTION
PREVENTION METHODS
Meningococcal disease is vaccine-preventable
DIAGNOSTIC SUPPORT
Neisseria meningitidis is a gram-negative diplococcus bacterium. Meningococci are classified into serogroups based on the composition of their capsular polysaccharide. The 6 major meningococcal serogroups associated with disease are A, B, C, W, X, and Y.
Meningococci spread through respiratory secretions and require close contact for transmission. Both asymptomatic carriers and people with overt meningococcal disease can be sources of infection. Asymptomatic carriage is transient and typically affects ≈5%–10% of the population at any given time.
N. meningitidis is found worldwide, but incidence is greatest in the “meningitis belt” of sub-Saharan Africa ( Map 5-01 ). Meningococcal disease is hyperendemic in this region, and periodic epidemics during the dry season (December–June) reach an incidence of up to 1,000 cases per 100,000 population. By contrast, rates of disease in Australia, Europe, South America, and the United States range from 0.10–2.4 cases per 100,000 population per year.
Although meningococcal disease outbreaks can occur anywhere in the world, they are most common in the African meningitis belt, where large-scale epidemics occur every 5–12 years. Historically, outbreaks in the meningitis belt were primarily due to serogroup A. With the introduction of a monovalent serogroup A meningococcal conjugate vaccine (MenAfriVac) in the region starting in 2010, however, recent meningococcal outbreaks in the meningitis belt have primarily been caused by serogroups C and W; serogroup X outbreaks also have been reported.
Outside the meningitis belt, infants, adolescents, and adults >80 years of age have the highest rates of disease. In meningitis belt countries, high rates of disease are seen in people ≤30 years old; the highest rates are in children and adolescents aged 5–14 years.
Unvaccinated travelers visiting meningitis belt countries and having prolonged contact with local populations during an epidemic are at greatest risk for meningococcal disease. The Hajj pilgrimage to Saudi Arabia also has been associated with outbreaks of meningococcal disease among returning pilgrims and their contacts, including 4 cases in travelers from the United States during a large Hajj-associated outbreak in 2000.
Map 5-01 The meningitis belt & other areas at risk for meningococcal meningitis epidemics
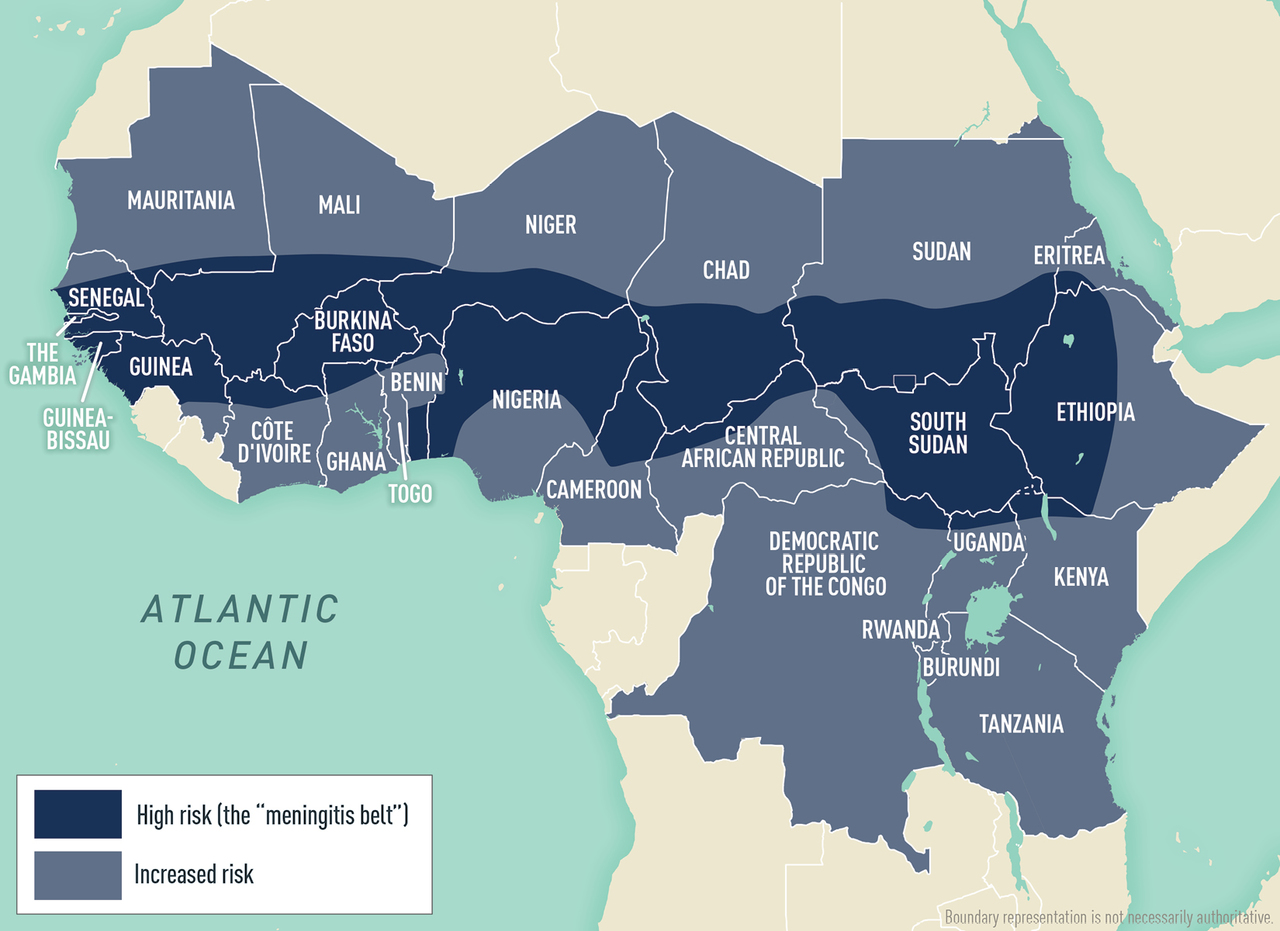
View Larger Figure
Disease data source: World Health Organization. International Travel and Health. Geneva, Switzerland: 2015.
Meningococcal disease generally occurs 1–10 days after exposure and presents as meningitis in ≈50% of cases in the United States. Meningococcal meningitis is characterized by sudden onset of headache, fever, and neck stiffness, sometimes accompanied by nausea, vomiting, photophobia, or altered mental status. Meningococcal disease progresses rapidly and has a case-fatality rate of 10%–15%, even with antimicrobial drug treatment. Without rapid treatment, fatality rates can be much higher.
Approximately 30% of people with meningococcal disease present with meningococcal sepsis, known as meningococcemia. Symptoms of meningococcemia can include abrupt onset of fever, chills, vomiting, diarrhea, and a petechial or purpuric rash, which can progress to purpura fulminans. Meningococcemia often involves hypotension, acute adrenal hemorrhage, and multiorgan failure. An additional 15% of meningococcal disease cases in the United States, primarily among adults >65 years of age, present as bacteremic pneumonia.
Other presentations (e.g., septic arthritis) also occur. Among infants and children aged <2 years, meningococcal disease can have nonspecific symptoms. Neck stiffness, usually seen in people with meningitis, might be absent in this age group.
Early diagnosis and treatment are critical. If bacterial meningitis is suspected, collect blood for culture right away and perform a lumbar puncture (LP) to collect cerebrospinal fluid (CSF) for microscopic examination and Gram stain. In general, diagnosis is made by isolating N. meningitidis from a normally sterile body site (e.g., blood, CSF) either by culture or by PCR detection of N. meningitidis –specific nucleic acid. State health departments can provide diagnostic and testing support if needed.
Signs and symptoms of meningococcal meningitis are like those of other causes of bacterial meningitis (e.g., Haemophilus influenzae , Streptococcus pneumoniae ). Proper treatment and prophylaxis depend on correctly identifying the causative organism. Meningococcal disease is nationally notifiable in the United States; report cases to the state or local health department without delay.
Meningococcal disease can be rapidly fatal and should always be viewed as a medical emergency. As soon as disease is suspected and blood cultures and CSF have been collected, deliver appropriate treatment; if the LP is to be delayed for any reason (e.g., imaging studies of the head prior to LP), administer antimicrobial drugs immediately after collecting blood cultures. Begin empiric antimicrobial drug treatment early and prior to receiving diagnostic test results.
Third-generation cephalosporins are recommended for empiric treatment. Although ampicillin or penicillin also can be used for treatment, determine meningococcal isolate susceptibility before switching to one of these antibiotics; recent reports indicate emerging penicillin resistance among meningococcal isolates in the United States. If a patient presents with suspected bacterial meningitis of uncertain etiology, some treatment algorithms recommend empiric use of dexamethasone in addition to an antimicrobial drug until a bacterial etiology is established; if meningococcal meningitis is confirmed or suspected, steroids can be discontinued.
Five meningococcal vaccines (3 quadrivalent, 2 monovalent) are licensed and available in the United States. Travelers should receive vaccines 7–10 days before travel to enable time for protective antibody levels to develop. See Table 5-03 for more information about available meningococcal vaccines.
Table 5-03 Meningococcal vaccines licensed & available in the United States: recommendations for travelers to or residents of countries where meningococcal disease is hyperendemic or epidemic 1
Abbreviations: IM, intramuscular
1 Source: TABLE 9. Recommended vaccination schedule and intervals for people who travel to or are residents of countries where meningococcal disease is hyperendemic or epidemic—Advisory Committee on Immunization Practices, United States, 2020 ( www.cdc.gov/mmwr/volumes/69/rr/rr6909a1.htm#T9_down ).
2 For people at continued risk, revaccination (booster) with meningococcal conjugate vaccine (MenACWY-CRM, -D, or -TT) is recommended for the following age groups: <7 years old, a single dose 3 years after primary vaccination and every 5 years thereafter; ≥7 years old, a single dose 5 years after primary vaccination and every 5 years thereafter.
3 A 2-dose primary series (DOSE 2 given 8–12 weeks after DOSE 1) is recommended for the following groups: people with HIV; people with anatomic or functional asplenia; people with persistent complement component deficiency (C3, C5-9, properdin, factor D, factor H); and people taking a complement component inhibitor (e.g., eculizumab [Soliris] or ravulizumab [Ultomiris]).
4 Can be administered ≥8 weeks apart in travelers.
5 MenB-FHbp and MenB-4C are not interchangeable; the same vaccine should be used for all doses, including booster doses.
6 A 3-dose primary series (DOSE 2 given 1–2 months after DOSE 1; DOSE 3 given 6 months after DOSE 2) is recommended for the following groups: people with anatomic or functional asplenia; people with persistent complement component deficiency (C3, C5-9, properdin, factor D, factor H); people taking a complement component inhibitor (e.g., eculizumab [Soliris] or ravulizumab [Ultomiris]); microbiologists routinely exposed to Neisseria meningitidis isolates; and people at risk during a serogroup B meningococcal disease outbreak.
7 A single booster dose of MenB vaccine is recommended for people at increased risk due to a serogroup B meningococcus outbreak if they completed the MenB primary series ≥1 year prior (≥6 months might also be considered by public health professionals). See: www.cdc.gov/meningococcal/downloads/meningococcal-outbreak-guidance.pdf [PDF}].
8 A booster dose of MenB vaccine is recommended 1 year after completion of the primary vaccination series and every 2–3 years thereafter for people who remain at increased risk of serogroup B meningococcal disease for any other reason.
Routine Immunization
The Advisory Committee on Immunization Practices (ACIP) recommends routine administration of a quadrivalent meningococcal conjugate vaccine (MenACWY) for all people aged 11–18 years. Administer a single dose of vaccine to patients at age 11 or 12 years and a booster dose at age 16 years. Routine immunization with MenACWY is not recommended for other age groups in the United States, except for people at increased risk for meningococcal disease, including those with a persistent complement component deficiency (C3, C5-9, properdin, factor D, factor H); people taking a complement component inhibitor (e.g., eculizumab [Soliris] or ravulizumab [Ultomiris]); people who have functional or anatomic asplenia; or people with HIV. ACIP describes vaccine, product, number of doses, and booster dose recommendations, based on age and risk factors for each risk group, in Meningococcal Vaccination: Recommendations of the Advisory Committee on Immunization Practices, United States, 2020 .
ACIP also recommends adolescents and young adults aged 16–23 years be vaccinated with a serogroup B meningococcal (MenB) vaccine series, based on shared clinical decision-making. A MenB vaccine series provides short-term protection against most strains of serogroup B meningococcus; 16–18 years is the optimal age for MenB vaccination. ACIP also recommends routine use of MenB vaccine for people aged ≥10 years who are at increased risk for meningococcal disease, including people who have persistent complement component deficiency and those with functional or anatomic asplenia. ACIP recommendations for use of MenB vaccines can be found in Meningococcal Vaccination: Recommendations of the Advisory Committee on Immunization Practices , United States, 2020.
Immunization For Travelers
Quadrivalent meningococcal conjugate (menacwy) vaccines.
ACIP recommends that travelers aged ≥2 months who visit or reside in parts of the meningitis belt of sub-Saharan Africa (see Map 5-01 ) during the dry season (December–June) receive vaccination with a MenACWY vaccine before travel. The Centers for Disease Control and Prevention (CDC) issues advisories for travelers to other countries when outbreaks of meningococcal disease are recognized; travelers should check the CDC Travelers’ Health website before travel. There are 3 meningococcal vaccines licensed and available in the United States for children; the age at vaccine initiation and schedule differs for each. See Table 5-03 for more information about meningococcal vaccines for young children.
The Kingdom of Saudi Arabia (KSA) requires travelers >2 years of age making the Umrah or Hajj pilgrimage to provide documentation of quadrivalent vaccine ≥10 days and ≤3 years before arrival for polysaccharide vaccine (MPSV4, no longer available in the United States) and ≤5 years before arrival for conjugate vaccine. Travelers should confirm visa requirements with the KSA embassy. Although the KSA Ministry of Health advises against travel to Hajj for pregnant people or children, these groups should receive meningococcal vaccination according to licensed indications for their age if they travel.
International travelers at risk for meningococcal disease who were previously vaccinated with a quadrivalent vaccine should receive a booster dose. For children who completed the primary dose or series at <7 years of age, administer a booster dose of MenACWY after 3 years and repeat every 5 years thereafter for those who live in or travel to hyperendemic areas. For people who received the primary dose or series at ≥7 years of age, administer a booster dose after 5 years and every 5 years thereafter for people who live in or travel to a hyperendemic area.
Monovalent Vaccines (Serogroups A, B & C)
In 2010, the Meningitis Vaccine Project introduced MenAfriVac, a monovalent serogroup A meningococcal conjugate vaccine, into meningitis belt countries through mass vaccination campaigns and the routine childhood immunization schedule. This vaccine is not licensed for use in the United States. US travelers going to live or work in the meningitis belt should receive a quadrivalent meningococcal conjugate vaccine (MenACWY) before leaving, to protect against 4 serogroups.
MenB vaccine is not recommended for people who live in or travel to meningitis belt countries, because serogroup B disease is extremely rare in this region. MenB vaccine is not routinely recommended for travelers to other regions of the world unless an outbreak of serogroup B disease has been reported.
In some countries outside the meningitis belt, meningococcal vaccination (e.g., monovalent conjugate C vaccine or MenB vaccine) might be recommended as part of the routine immunization program for infants. Clinicians can consider meningococcal vaccination for infants residing in these countries, according to the routine immunization recommendations of that country.
Safety & Adverse Reactions
Side effects after MenACWY vaccination include low-grade fevers and local reactions (e.g., injection-site pain, arm swelling, pain that limits movement of the injected arm). Symptoms are generally mild to moderate and resolve within 48–72 hours. Severe adverse events (e.g., high fever, chills, joint pain, rash, seizures) are rare (<5% of vaccinees).
Although no clinical trials of meningococcal vaccines have been conducted in people who are pregnant or lactating, post-licensure safety data have not identified any serious safety concerns to the mother or fetus. Pregnancy or lactation should not preclude vaccination with MenACWY if indicated.
Precautions & Contraindications
People with moderate or severe acute illness should defer vaccination until their condition improves. Vaccination is contraindicated for people who have had a severe allergic reaction to any component of the vaccines or to a prior dose of the vaccine. A severe allergic reaction to any diphtheria toxoid- or CRM197-containing vaccine also is a contraindication for MenACWY-D and MenACWY-CRM; severe allergic reaction to any tetanus toxoid–containing vaccine is a contraindication for MenACWY-TT.
To avoid interference with the immune response to meningococcal vaccine, MenACWY-D should be given either before or at the same time as DTaP in children. MenACWY-D may be given at any time in relation to Tdap or Td.
All meningococcal vaccines are inactivated and can be given to people who are immunosuppressed.
Postexposure Prophylaxis
In the United States and most industrialized countries, antibiotic chemoprophylaxis is recommended for close contacts of a patient with invasive meningococcal disease to prevent secondary cases. Chemoprophylaxis ideally should be initiated within 24 hours after the index patient is identified; prophylaxis given >2 weeks after exposure has little value.
Antibiotics used for prophylaxis include ceftriaxone, ciprofloxacin, and rifampin. Ceftriaxone is recommended for pregnant people. CDC provides detailed information on meningococcal prophylaxis in the Manual for the Surveillance of Vaccine-Preventable Diseases .
CDC website: Meningococcal disease
The following authors contributed to the previous version of this chapter: Sarah A. Mbaeyi, Lucy A. McNamara
Bibliography
American Academy of Pediatrics. Meningococcal infections. In: Kimberlin DW, Brady MT, Jackson M, Long SS, editors. Red Book: 2015 report of the Committee on Infectious Diseases, 30th edition. Elk Grove Village (IL): American Academy of Pediatrics; 2015. pp. 547–58.
Centers for Disease Control and Prevention. Public health dispatch: Update: assessment of risk for meningococcal disease associated with the Hajj 2001. MMWR Morb Mortal Wkly Rep. 2001;50(12):221–2.
Folaranmi T, Rubin L, Martin SW, Patel M, MacNeil JR. Use of serogroup B meningococcal vaccines in persons aged >/=10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(22):608–12.
Halperin SA, Bettinger JA, Greenwood B, Harrison LH, Jelfs J, Ladhani SN, et al. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30(Suppl 2):B26–36.
MacNeil JR, Rubin L, Folaranmi T, Ortega-Sanchez IR, Patel M, Martin SW. Use of serogroup B meningococcal vaccines in adolescents and young adults: recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(41):1171–6.
Mbaeyi SA, Bozio CH, Duffy J, Rubin LG, Hariri S, Stephens DS, et al. Meningococcal vaccination: recommendations of the Advisory Committee on Immunization Practices, United States, 2020. MMWR Recomm Rep. 2020;69(9):1–41.
McNamara LA, Potts C, Blain AE, Retchless AC, Reese N, Swint S, et al. Detection of ciprofloxacin-resistant, β-lactamase-producing Neisseria meningitidis serogroup Y isolates—United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):735–9.
Patton ME, Stephens D, Moore K, MacNeil JR. Updated recommendations for use of MenB-FHbp serogroup B meningococcal vaccine—Advisory Committee on Immunization Practices, 2016. MMWR Morb Mortal Wkly Rep. 2016;66(19);509–13.
Trotter CL, Lingani C, Fernandez K, Cooper LV, Bita A, Tevi-Benissan C, et al. Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–2015: an analysis of surveillance data. Lancet Infect Dis. 2017;17(8):867–72.
World Health Organization. Epidemic meningitis control in countries of the African meningitis belt, 2016. Wkly Epidemiol Rec. 2017;92(13):145–54.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Measles — United States, January 1, 2020–March 28, 2024
Weekly / April 11, 2024 / 73(14);295–300
Adria D. Mathis, MSPH 1 ; Kelley Raines, MPH 1 ; Nina B. Masters, PhD 1 ; Thomas D. Filardo, MD 1 ; Gimin Kim, MS 1 ; Stephen N. Crooke, PhD 1 ; Bettina Bankamp, PhD 1 ; Paul A. Rota, PhD 1 ; David E. Sugerman, MD 1 ( View author affiliations )
What is already known about this topic?
Although endemic U.S. measles was declared eliminated in 2000, measles importations continue to occur. Prolonged outbreaks during 2019 threatened the U.S. measles elimination status.
What is added by this report?
During January 1, 2020–March 28, 2024, a total of 338 U.S. measles cases were reported; 29% of these cases occurred during the first quarter of 2024, almost all in persons who were unvaccinated or whose vaccination status was unknown. As of the end of 2023, U.S. measles elimination status was maintained.
What are the implications for public health practice?
Risk for widespread U.S. measles transmission remains low because of high population immunity. Enhanced efforts are needed to increase routine U.S. vaccination coverage, encourage vaccination before international travel, identify communities at risk for measles transmission, and rapidly investigate suspected measles cases to reduce cases and complications of measles.
- Article PDF
- Full Issue PDF

Measles is a highly infectious febrile rash illness and was declared eliminated in the United States in 2000. However, measles importations continue to occur, and U.S. measles elimination status was threatened in 2019 as the result of two prolonged outbreaks among undervaccinated communities in New York and New York City. To assess U.S. measles elimination status after the 2019 outbreaks and to provide context to understand more recent increases in measles cases, CDC analyzed epidemiologic and laboratory surveillance data and the performance of the U.S. measles surveillance system after these outbreaks. During January 1, 2020–March 28, 2024, CDC was notified of 338 confirmed measles cases; 97 (29%) of these cases occurred during the first quarter of 2024, representing a more than seventeenfold increase over the mean number of cases reported during the first quarter of 2020–2023. Among the 338 reported cases, the median patient age was 3 years (range = 0–64 years); 309 (91%) patients were unvaccinated or had unknown vaccination status, and 336 case investigations included information on ≥80% of critical surveillance indicators. During 2020–2023, the longest transmission chain lasted 63 days. As of the end of 2023, because of the absence of sustained measles virus transmission for 12 consecutive months in the presence of a well-performing surveillance system, U.S. measles elimination status was maintained. Risk for widespread U.S. measles transmission remains low because of high population immunity. However, because of the increase in cases during the first quarter of 2024, additional activities are needed to increase U.S. routine measles, mumps, and rubella vaccination coverage, especially among close-knit and undervaccinated communities. These activities include encouraging vaccination before international travel and rapidly investigating suspected measles cases.
Introduction
Measles is a highly infectious acute, febrile rash illness with a >90% secondary attack rate among susceptible contacts ( 1 ). High national 2-dose coverage with the measles, mumps, and rubella (MMR) vaccine led to the declaration of U.S. measles elimination* in 2000 ( 2 ). However, this elimination status was threatened in 2019 because of two prolonged outbreaks among undervaccinated communities in New York and New York City; these outbreaks accounted for 29% of all reported cases during 2001–2019 ( 2 ). To assess U.S. measles elimination status after the 2019 outbreaks and to provide context for understanding more recent increases in measles cases in 2024, † CDC assessed the epidemiologic and laboratory-based surveillance of measles in the United States and the performance of the U.S. measles surveillance system during January 1, 2020–March 28, 2024.
Reporting and Classification of Measles Cases
Confirmed measles cases § ( 1 ) are reported to CDC by state health departments through the National Notifiable Disease Surveillance System and directly (by email or telephone) to the National Center for Immunization and Respiratory Diseases. Measles cases are classified by the Council of State and Territorial Epidemiologists as import-associated if they were internationally imported, epidemiologically linked to an imported case, or had viral genetic evidence of an imported measles genotype ( 1 ); cases with no epidemiologic or virologic link to an imported case are classified as having an unknown source ( 1 ). For this analysis, unique sequences were defined as those differing by at least one nucleotide in the N-450 sequence (the 450 nucleotides encoding the carboxyl-terminal 150 nucleoprotein amino acids) based on the standard World Health Organization (WHO) recommendations for describing sequence variants ¶ ( 3 ). Unvaccinated patients were classified as eligible for vaccination if they were not vaccinated according to Advisory Committee on Immunization Practices recommendations ( 4 ). A well-performing surveillance system was defined as one with ≥80% of cases meeting each of the following three criteria: classified as import-associated, reported with complete information on at least eight of 10 critical surveillance indicators (i.e., place of residence, sex, age, occurrence of fever and rash, date of rash onset, vaccination status, travel history, hospitalization, transmission setting, and whether the case was outbreak-related) ( 5 ), and laboratory-confirmed.
Assessment of Chains of Transmission
Cases were classified into chains of transmission on the basis of known epidemiologic linkages: isolated (single) cases, two-case chains (two epidemiologically linked cases), and outbreaks (three or more epidemiologically linked cases). The potential for missed cases within two-case chains and outbreaks was assessed by measuring the interval between measles rash onset dates in each chain; chains with more than one maximum incubation period (21 days) between cases could indicate a missing case in the chain. This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.**
Reported Measles Cases and Outbreaks
CDC was notified of 338 confirmed measles cases with rash onset during January 1, 2020–March 28, 2024 ( Figure ); cases occurred in 30 jurisdictions. During 2020, 12 of 13 cases preceded the commencement of COVID-19 mitigation efforts in March 2020. Among the 170 cases reported during 2021 and 2022, 133 (78%) were associated with distinct outbreaks: 47 (96%) of 49 cases in 2021 occurred among Afghan evacuees temporarily housed at U.S. military bases during Operation Allies Welcome, and 86 (71%) of 121 cases in 2022 were associated with an outbreak in central Ohio. During 2023, 28 (48%) of 58 cases were associated with four outbreaks. As of March 28, 2024, a total of 97 cases have been reported in 2024, representing 29% of all 338 measles cases reported during January 1, 2020–March 28, 2024, and more than a seventeenfold increase over the mean number of cases reported during the first quarter of 2020–2023 (five cases).
Characteristics of Reported Measles Cases
The median patient age was 3 years (range = 0–64 years); more than one half of cases (191; 58%) occurred in persons aged 16 months–19 years ( Table ). Overall, 309 (91%) patients were unvaccinated (68%) or had unknown vaccination status (23%); 29 (9%) had previously received ≥1 MMR vaccine dose. Among the 309 cases among unvaccinated persons or persons with unknown vaccination status, 259 (84%) patients were eligible for vaccination, 40 (13%) were aged 6–11 months and therefore not recommended for routine MMR vaccination, and 10 (3%) were ineligible for MMR because they were aged <6 months. †† Among 155 (46%) hospitalized measles patients, 109 (70%) cases occurred in persons aged <5 years; 142 (92%) hospitalized patients were unvaccinated or had unknown vaccination status. No measles-associated deaths were reported to CDC.
Imported Measles Cases
Among all 338 cases, 326 (96%) were associated with an importation; 12 (4%) had an unknown source. Among the 326 import-associated cases, 200 (61%) occurred among U.S. residents who were eligible for vaccination but who were unvaccinated or whose vaccination status was unknown. Among 93 (28%) measles cases that were directly imported from other countries, 34 (37%) occurred in foreign visitors, and 59 (63%) occurred in U.S. residents, 53 (90%) of whom were eligible for vaccination but were unvaccinated or whose vaccination status was unknown. One (2%) case in a U.S. resident occurred in a person too young for vaccination, two (3%) in persons who had previously received 1 MMR vaccine dose, and three (5%) in persons who had previously received 2 MMR vaccine doses. The most common source for internationally imported cases during the study period were the Eastern Mediterranean (48) and African (24) WHO regions. During the first quarter of 2024, a total of six internationally imported cases were reported from the European and South-East Asia WHO regions, representing a 50% increase over the mean number of importations from these regions during 2020–2023 (mean of two importations per year from each region).
Surveillance Quality Indicators
Overall, all but two of the 338 case investigations included information on ≥80% of the critical surveillance indicators; those two case investigations included information on 70% of critical surveillance indicators. Date of first case report to a health department was available for 219 (65%) case investigations; 127 (58%) cases were reported to health departments on or before the day of rash onset (IQR = 4 days before to 3 days after). Overall, 314 (93%) measles cases were laboratory confirmed, including 16 (5%) by immunoglobulin M (serologic) testing alone and 298 (95%) by real-time reverse transcription–polymerase chain reaction (rRT-PCR). Among 298 rRT-PCR–positive specimens, 221 (74%) were successfully genotyped: 177 (80%) were genotype B3, and 44 (20%) were genotype D8. Twenty-two distinct sequence identifiers (DSIds) ( 3 ) for genotype B3 and 13 DSIds for genotype D8 were detected (Supplementary Figure, https://stacks.cdc.gov/view/cdc/152776 ). The longest period of detection for any DSId was 15 weeks (DSId 8346).
Chains of Transmission
The 338 measles cases were categorized into 92 transmission chains (Table); 62 (67%) were isolated cases, 10 (11%) were two-case chains, and 20 (22%) were outbreaks of three or more cases. Seven (35%) of 20 outbreaks occurred during 2024. §§ The median outbreak size was six cases (range = three–86 cases) and median duration of transmission was 20 days (range = 6–63 days). Among the 30 two-case chains and outbreaks, more than one maximum incubation period (21 days) did not elapse between any two cases.
Because of the absence of endemic measles virus transmission for 12 consecutive months in the presence of a well-performing surveillance system, as of the end of 2023, measles elimination has been maintained in the United States. U.S. measles elimination reduces the number of cases, deaths, and costs that would occur if endemic measles transmission were reestablished. Investigation of almost all U.S. measles cases reported since January 2020 were import-associated, included complete information on critical surveillance variables, were laboratory-confirmed by rRT-PCR, and underwent genotyping; these findings indicate that the U.S. measles surveillance system is performing well. A variety of transmission chain sizes were detected, including isolated cases, suggesting that sustained measles transmission would be rapidly detected. However, the rapid increase in the number of reported measles cases during the first quarter of 2024 represents a renewed threat to elimination.
Most measles importations were cases among persons traveling to and from countries in the Eastern Mediterranean and African WHO regions; these regions experienced the highest reported measles incidence among all WHO regions during 2021–2022 ( 6 ). During November 2022–October 2023, the number of countries reporting large or disruptive outbreaks increased by 123%, from 22 to 49. Global estimates suggest that first-dose measles vaccination coverage had declined from 86% in 2019 to 83% in 2022, leaving almost 22 million children aged <1 year susceptible to measles ( 6 ).
As has been the case in previous postelimination years ( 7 ), most imported measles cases occurred among unvaccinated U.S. residents. Increasing global measles incidence and decreasing vaccination coverage will increase the risk for importations into U.S. communities, as has been observed during the first quarter of 2024, further supporting CDC’s recommendation for persons to receive MMR vaccine before international travel ( 4 ).
Maintaining high national and local MMR vaccination coverage remains central to sustaining measles elimination. Risk for widespread U.S. measles transmission remains low because of high population immunity; however, national 2-dose MMR vaccination coverage has remained below the Healthy People 2030 target of 95% (the estimated population-level immunity necessary to prevent sustained measles transmission) ( 8 ) for 3 consecutive years, leaving approximately 250,000 kindergarten children susceptible to measles each year ( 9 ). Furthermore, 2-dose MMR vaccination coverage estimates in 12 states and the District of Columbia were <90%, and during the 2022–23 school year, exemption rates among kindergarten children exceeded 5% in 10 states ( 9 ). Clusters of unvaccinated persons placed communities at risk for large outbreaks, as occurred during the central Ohio outbreak in 2022: 94% of measles patients were unvaccinated and 42% were hospitalized ( 10 ). Monitoring MMR vaccination coverage at county and zip code levels could help public health agencies identify undervaccinated communities for targeted interventions to improve vaccination coverage while preparing for possible measles outbreaks. As of March 28, 2024, a total of 97 confirmed measles cases have been reported in the United States in 2024, compared with a mean of five cases during the first quarter of each year during 2020–2023. Similar to cases reported during 2020–2023, most cases reported during 2024 occurred among patients aged <20 years who were unvaccinated or whose vaccination status was unknown, and were associated with an importation. Rapid detection of cases, prompt implementation of control measures, and maintenance of high national measles vaccination coverage, including improving coverage in undervaccinated populations, is essential to preventing measles and its complications and to maintaining U.S. elimination status.
Limitations
The findings in this report are subject to at least three limitations. First, importations might have been underreported: 4% of reported cases during the study period had no known source. Second, case investigations resulting in discarded measles cases (i.e., a diagnosis of measles excluded) are not nationally reportable, which limits the ability to directly evaluate the sensitivity of measles case investigations. However, surveillance remains sufficiently sensitive to detect isolated cases and outbreaks, and robust molecular epidemiology provides further evidence supporting the absence of sustained measles transmission in the United States. Finally, the date of first case report to a health department was not available for 35% of case investigations.
Implications for Public Health Practice
The U.S. measles elimination status will continue to be threatened by global increases in measles incidence and decreases in global, national, and local measles vaccination coverage. Because of high population immunity, the risk of widespread measles transmission in the United States remains low; however, efforts are needed to increase routine MMR vaccination coverage, encourage vaccination before international travel, identify communities at risk for measles transmission, and rapidly investigate suspected measles cases to maintain elimination.
Corresponding author: Adria D. Mathis, [email protected] .
1 Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Stephen N. Crooke reports institutional support from PATH. No other potential conflicts of interest were disclosed.
* Elimination is defined as the absence of endemic measles virus transmission in a defined geographic area for ≥12 months in the presence of a well-performing surveillance system.
† https://emergency.cdc.gov/han/2024/han00504.asp
§ A confirmed measles case was defined as an acute febrile rash illness with laboratory confirmation or direct epidemiologic linkage to a laboratory-confirmed case. Laboratory confirmation was defined as detection of measles virus–specific nucleic acid from a clinical specimen using real-time reverse transcription–polymerase chain reaction or a positive serologic test for measles immunoglobulin M antibody.
¶ Genotyping was performed at CDC and at the Vaccine Preventable Disease Reference Centers of the Association of Public Health Laboratories.
** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
†† MMR vaccine is not licensed for use in persons aged <6 months.
§§ At the time of this report, six measles outbreaks have ended, and one outbreak is ongoing. A measles outbreak is considered to be over when no new cases have been identified during two incubation periods (42 days) since the rash onset in the last outbreak-related case.
- Gastañaduy PA, Redd SB, Clemmons NS, et al. Measles [Chapter 7]. In: Manual for the surveillance of vaccine-preventable diseases. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html
- Mathis AD, Clemmons NS, Redd SB, et al. Maintenance of measles elimination status in the United States for 20 years despite increasing challenges. Clin Infect Dis 2022;75:416–24. https://doi.org/10.1093/cid/ciab979 PMID:34849648
- Williams D, Penedos A, Bankamp B, et al. Update: circulation of active genotypes of measles virus and recommendations for use of sequence analysis to monitor viral transmission. Weekly Epidemiologic Record 2022;97(39):481–92. https://reliefweb.int/report/world/weekly-epidemiological-record-wer-30-september-2022-vol-97-no-39-2022-pp-481-492-enfr
- McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS; CDC. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(No. RR-4):1–34. PMID:23760231
- World Health Organization. Measles: vaccine preventable diseases surveillance standards. Geneva, Switzerland: World Health Organization; 2018. https://www.who.int/publications/m/item/vaccine-preventable-diseases-surveillance-standards-measles
- Minta AA, Ferrari M, Antoni S, et al. Progress toward measles elimination—worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep 2023;72:1262–8. https://doi.org/10.15585/mmwr.mm7246a3 PMID:37971951
- Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the postelimination era, 2001–2016. J Infect Dis 2019;219:1616–23. https://doi.org/10.1093/infdis/jiy701 PMID:30535027
- Truelove SA, Graham M, Moss WJ, Metcalf CJE, Ferrari MJ, Lessler J. Characterizing the impact of spatial clustering of susceptibility for measles elimination. Vaccine 2019;37:732–41. https://doi.org/10.1016/j.vaccine.2018.12.012 PMID:30579756
- Seither R, Yusuf OB, Dramann D, Calhoun K, Mugerwa-Kasujja A, Knighton CL. Coverage with selected vaccines and exemption from school vaccine requirements among children in kindergarten—United States, 2022–23 school year. MMWR Morb Mortal Wkly Rep 2023;72:1217–24. https://doi.org/10.15585/mmwr.mm7245a2 PMID:37943705
- Tiller EC, Masters NB, Raines KL, et al. Notes from the field: measles outbreak—central Ohio, 2022–2023. MMWR Morb Mortal Wkly Rep 2023;72:847–9. https://doi.org/10.15585/mmwr.mm7231a3 PMID:37535476
FIGURE . Confirmed measles cases, by month of rash onset (N = 338) — United States, January 1, 2020–March 28, 2024
Abbreviations: IgM = immunoglobulin M; rRT-PCR = real-time reverse transcription–polymerase chain reaction; WHO = World Health Organization. * A case resulting from exposure to measles virus outside the United States as evidenced by at least some of the exposure period (7–21 days before rash onset) occurring outside the United States and rash onset occurring within 21 days of entering the United States without known exposure to measles during that time. † A case in a transmission chain epidemiologically linked to an internationally imported case. § A case for which an epidemiologic link to an internationally imported case was not identified, but for which viral sequence data indicate an imported measles genotype (i.e., a genotype that is not detected in the United States with a pattern indicative of endemic transmission). ¶ A case for which an epidemiologic or virologic link to importation or to endemic transmission within the United States cannot be established after a thorough investigation. ** Percentage is percentage of international importations. Four cases among persons who traveled to both the Eastern Mediterranean and African regions and one case in a person who traveled to both the Eastern Mediterranean and European regions were counted twice. †† Place of residence, sex, age or date of birth, fever and rash, date of rash onset, vaccination status, travel history, hospitalization, transmission setting, and whether the case was outbreak related. §§ Includes 65 cases among patients who received both positive rRT-PCR and positive IgM results. ¶¶ Percentage is percentage of total chains.
Suggested citation for this article: Mathis AD, Raines K, Masters NB, et al. Measles — United States, January 1, 2020–March 28, 2024. MMWR Morb Mortal Wkly Rep 2024;73:295–300. DOI: http://dx.doi.org/10.15585/mmwr.mm7314a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer
MomsWhoSave.com
Living Well. Shopping Smart. Family, deals, recipes, travel, reviews, home and decor, beauty, fashion, and much more!
More results...
5 Simple Tips for Healthy Travel + What to Include in your Travel Health Kit
Disclosure: Articles may contain affiliate links. As an Amazon Associate, we earn from qualifying purchases (at no additional cost to you). See our full disclosure here .
Last updated on April 1st, 2024 at 05:25 pm

Whether you plan to travel to the tropics or hit the slopes at a snowy resort, don’t forget to plan for your health. While every destination is different, these tips can help you plan for a safe and healthy trip.
Tips for Healthy Travel
Learn about your destination.
Visit the CDC travel health website to learn about any health risks and to get the most up-to-date travel information and warnings in effect in the country you’re planning to visit.
It is also important to understand the laws and culture of the places you will be visiting. You can learn about countries using resources like websites, guidebooks, and other media.
Think about your health status
No one wants to miss or postpone a trip, but there are times when staying home might be best for health reasons. Have you had any recent illnesses, injuries, or surgeries? Do you have any special health needs, due to disability, pregnancy, or a compromised immune system? Take these questions into consideration before you leave home.
See your doctor
The best time to see your doctor is four to six weeks before traveling. If it’s less than four weeks before you leave, you should still see your doctor. You might still benefit from shots or medications and information about how to protect yourself from illness and injury while traveling.
If you need Covid-19 tests to meet travel requirements, you may want to consider a concierge medicine practice. These health care providers can visit you at home or the office, allowing you easily fit a visit into your schedule before your departure.

If you’re traveling abroad, it is important to bring copies of your passport and travel documents. Put copies in each piece of luggage, in case you lose the original documents. Don’t forget to leave a copy with a friend or relative at home too.
Some people choose to save a photo or scanned copy of their important documents to Dropbox or Google Drive, or even email the the document copies to themselves. If you do this, sign out of these apps on your phone (or laptop) in the event you lose your device or it is stolen.
Along with your documents, a travel health kit can also help make your trip a safe and healthy one.
What to include in your Travel Heath Kit:
o Prescribed medicine o Over-the-counter medicine o Antidiarrheal medication o Antihistamine or allergy medication o Decongestant o Anti-motion sickness medication o Medicine for pain or fever o Mild laxative o Cough suppressant/expectorant o Cough drops o Antacid o Antifungal and antibacterial ointments or creams o 1% hydrocortisone cream o First aid supplies o First aid quick reference card o Basic first aid items (bandages, gauze, Ace bandage, antiseptic, tweezers, scissors, cotton-tipped applicators) o Moleskin for blisters o Aloe gel for sunburns o Digital thermometer o Oral rehydration solution packets o Sunscreen (SPF 15 or above) o Insect repellent o Alcohol-based hand sanitizer o Health insurance card and copies of claim forms
If you’re traveling with prescription medications, bring a copy of your prescription. Pack a note on letterhead stationery from the prescribing physician if you’re bringing controlled substances or injectable medications.
Plan ahead for illness or injury
Check your health insurance plan to see if they will cover your health needs abroad. Think about purchasing additional health or travel insurance for your trip if your insurance doesn’t cover you.
Pay attention to your health during your trip, and see a doctor if you’re injured or feel ill. When traveling abroad, be sure you know the local emergency number in case of a sudden severe illness or injury.
Additional Resources
To get more tips for healthy travel, visit http://www.cdc.gov/travel or call 1-800-CDCINFO.
Making travel plans? Find travel deals here .
You might also like… Flight Hack: How to Use the 24-Hour Rule to Save Big Gift Guide: 20 Great Gifts for Travel Lovers Find Travel Deals
You can find MomsWhoSave on Facebook , Instagram , and Twitter. Join us for updates!
Don’t miss a thing! Subscribe to MomsWhoSave’s newsletter .
Reader Interactions
Donna Martin
thank you for the tips
Amber Albertson
I needed this! Thank you! We are traveling in june with our two kids that are under two and I have been struggling so bad even thinking about it
I don’t see a mask or gloves on that list of things to pack, with the Corona Virus and all. I have to bring a doctors note because I am a Diabetic and I need to bring syringes. I also bring Benadryl, because eating foods you are not used to could cause an allergic reaction. A lot of people I know have cut down their traveling, because of the virus. The hand soap is important. Be careful and safe everyone!
Dale Steele Nicolov
it is a good idea to take some medical supplies to avoid medical issues while traveling.I took an anti biotic with me to Cuba when I went .I didn’t need it but my friend did .
Christina Gould
I’ve never seen a health kit packing list before. Thanks for posting!
Linda Linneman
I would love to take a great family vacation. I haven’t done that in a long time. I really appreciate this information you shared. Thank you so much. God Bless
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .
follow along
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
What the data says about abortion in the U.S.
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
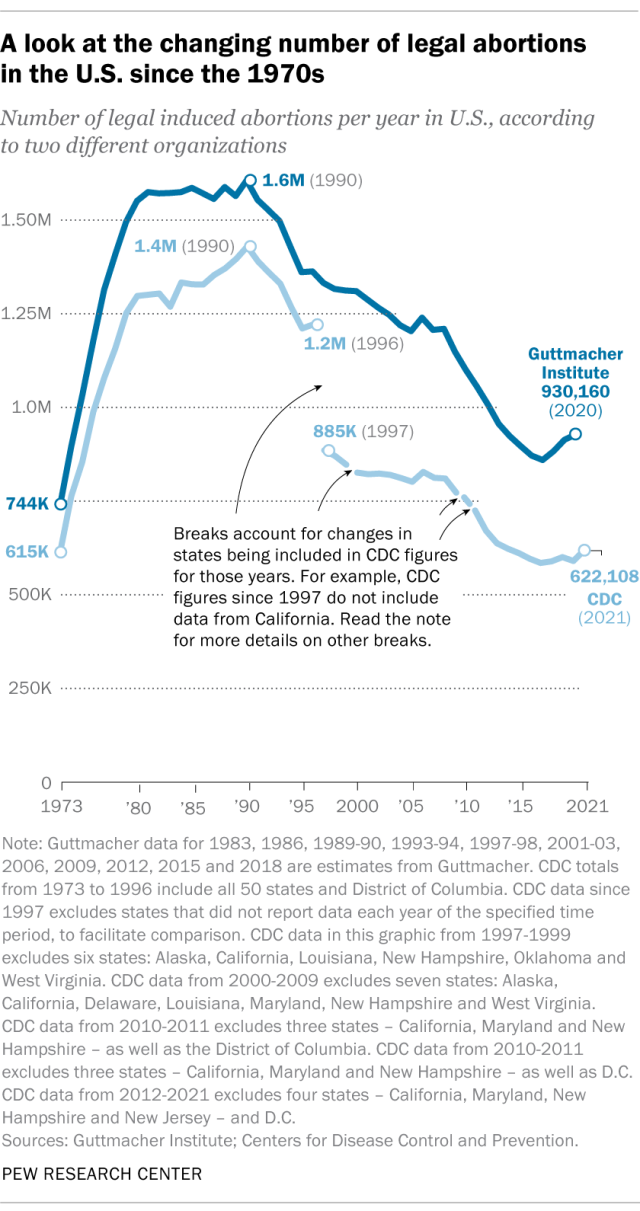
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
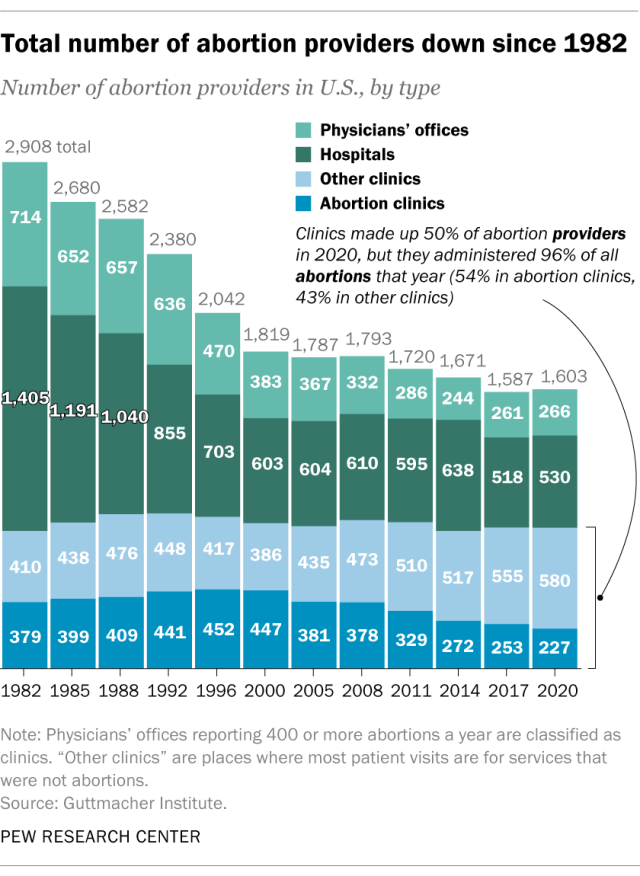
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
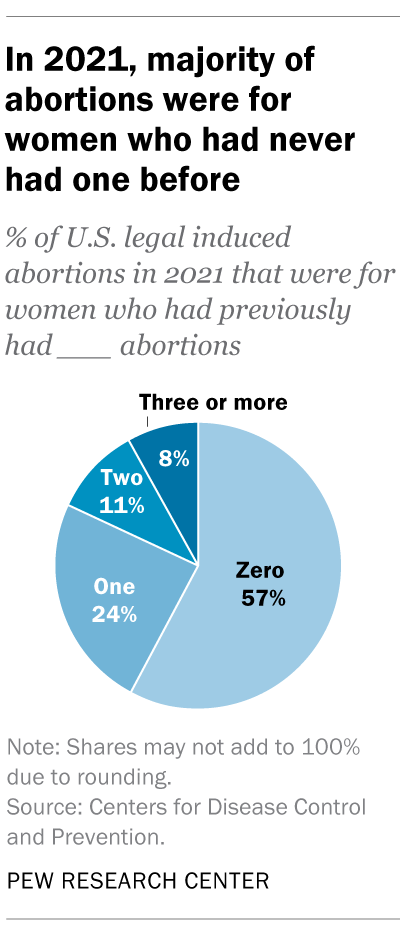
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
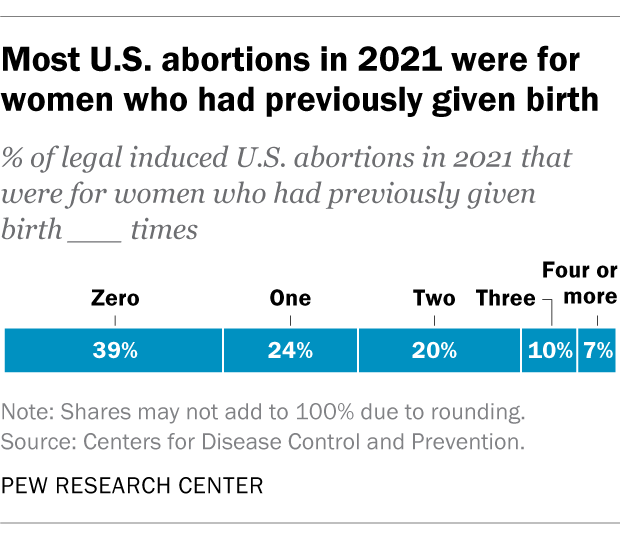
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Support for legal abortion is widespread in many countries, especially in Europe
Nearly a year after roe’s demise, americans’ views of abortion access increasingly vary by where they live, by more than two-to-one, americans say medication abortion should be legal in their state, most latinos say democrats care about them and work hard for their vote, far fewer say so of gop, positive views of supreme court decline sharply following abortion ruling, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy

IMAGES
COMMENTS
More. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Know Your Health Status. Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give ...
During 2020-2022, CDC used these authorities to restrict travel of people with COVID-19 and close contacts who were recommended to quarantine. These authorities were also used for mpox during 2022. Travel restrictions can also be used for other suspected or confirmed contagious diseases that could pose a public health threat during travel ...
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.
The nearest US embassy or consulate can help travelers locate medical services and notify your friends, family, or employer of an emergency. They are available for emergencies 24 hours a day, 7 days a week, overseas and in Washington, DC (888-407-4747 or 202-501-4444). The US Department of State maintains a list of travel medical and evacuation ...
Dengue in the Americas February 28, 2024 Dengue is a risk in many parts of Central and South America, Mexico, and the Caribbean. Some countries are reporting increased numbers of cases of the disease. Travelers to the Americas can protect themselves by preventing mosquito bites. Destination List: Argentina, Brazil, Colombia, Costa Rica, French ...
Protect your child and family when traveling in the United States or abroad by: Getting the shots required for all countries you and your family plan to visit during your trip. Making sure you and your family are up-to-date on all routine U.S. vaccines. Staying informed about travel notices and alerts and how they can affect your family's ...
Yes. CDC recommends that all travelers avoid all cruise ship travel worldwide, including river boats. Reports of COVID-19 on cruise ships highlight the risk of infection to cruise ship passengers and crew. Like many other viruses, COVID-19 appears to spread more easily between people in close quarters aboard ships.
The CDC Travelers' Health Branch provides international travel health advice, including vaccine recommendations and requirements, behavioral precautions, and advice for specific worldwide events. We play an integral role in many of CDC's global emergency response efforts, such as the H1N1 influenza pandemic and the MERS, Ebola, and Zika ...
Travelers should additionally follow any requirements at their destination. CDC also recommends that you get tested 3-5 days after international air travel AND stay home for 7 days. Even if you test negative, stay home for the full 7 days. If you don't get tested, it's safest to stay home for 10 days after travel.
CDC is the nation's leading science-based, data-driven, service organization that protects the public's health. For more than 70 years, we've put science into action to help children stay healthy so they can grow and learn; to help families, businesses, and communities fight disease and stay strong; and to protect the public's health.
No matter where you plan to travel, check CDC's destination pages for travel health information. These pages include information about. vaccines and medicines you may need, and; diseases or health risks that are a concern at your destination. Get up to date with your COVID-19 vaccines and seasonal flu vaccine.
Q. What are the requirements for travelers entering the United States through land POEs? A: Before embarking on a trip to the United States, non-U.S. travelers should be prepared for the following: Possess proof of an approved COVID-19 vaccination as outlined on the CDC website. During border inspection, verbally attest to their COVID-19 vaccination status.
By Mayo Clinic Staff. A coronavirus disease 2019 (COVID-19) vaccine can prevent you from getting COVID-19 or from becoming seriously ill due to COVID-19. But even if you're vaccinated, it's still a good idea to take precautions to protect yourself and others while traveling during the COVID-19 pandemic. If you've had all recommended COVID-19 ...
CDC uses Travel Health Notices (THNs) to alert travelers and other audiences to health threats around the world and advise on how to protect themselves. On November 21, 2020, CDC adapted its 3-level notice system to a 4-level l l system for COVID-19 and updated criteria used to determine THN levels. The system was updated to align with the same ...
Medicare does not cover medical care when you travel the United States. Visit Medicare.gov for more information. Some health insurance companies pay for "customary and reasonable" hospital costs abroad. Very few pay for your medical evacuation back to the United States. The cost may exceed $250,000, depending on your location and medical ...
This is why CDC recommends the wearing of a face mask an important additional measure against exposing yourself or others to COVID-19. It is important to follow basic guidance on wearing a face mask and frequently washing your hands or using hand sanitizer with at least 60% alcohol. For more information see CDC's Travel During the COVID-19 ...
Meningococcal disease generally occurs 1-10 days after exposure and presents as meningitis in ≈50% of cases in the United States. Meningococcal meningitis is characterized by sudden onset of headache, fever, and neck stiffness, sometimes accompanied by nausea, vomiting, photophobia, or altered mental status.
Read the country information page for additional information on travel to Saudi Arabia. The Centers for Disease Control and Prevention (CDC) has determined Saudi Arabia has a low level of COVID-19. Visit the CDC page for the latest Travel Health Information related to your travel. If you decide to travel to Saudi Arabia:
Methods Reporting and Classification of Measles Cases. Confirmed measles cases § (1) are reported to CDC by state health departments through the National Notifiable Disease Surveillance System and directly (by email or telephone) to the National Center for Immunization and Respiratory Diseases.Measles cases are classified by the Council of State and Territorial Epidemiologists as import ...
o Antacid. o Antifungal and antibacterial ointments or creams. o 1% hydrocortisone cream. o First aid supplies. o First aid quick reference card. o Basic first aid items (bandages, gauze, Ace bandage, antiseptic, tweezers, scissors, cotton-tipped applicators) o Moleskin for blisters. o Aloe gel for sunburns.
Previous reports can be found at stacks.cdc.gov by entering "abortion surveillance" into the search box. For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services.