
- Find a Doctor
- Patients & Visitors
- ER Wait Times
- For Medical Professionals
- Piedmont MyChart

- Medical Professionals
- Find Doctors
- Find Locations
Receive helpful health tips, health news, recipes and more right to your inbox.

Sign up to receive the Living Real Change Newsletter
What to expect in the emergency department
“The emergency department is an area in the hospital where we can quickly assess patients, make them better, or decide they’re going to need additional testing or management and admit them to the hospital,” says Jeffrey Oyler, M.D. , an emergency medicine physician at Piedmont Atlanta Hospital .
Every patient who visits the emergency department (ED) will go through triage, which allows the ED team to establish the severity of that person’s condition. Triage takes into account the patient’s vital signs, as well as his or her complaint. Dr. Oyler says measuring the patient’s vital signs is the most crucial component of triage because these signs are essential to assessing the patient and are something that cannot be faked. The patient is then categorized based on the Emergency Severity Index:
- Level 1 – Immediate: life-threatening
- Level 2 – Emergency: could be life-threatening
- Level 3 – Urgent: not life-threatening
- Level 4 – Semi-urgent: not life-threatening
- Level 5 – Non-urgent: needs treatment as time permits
“It’s hugely important for us to establish who is the sickest, so we can provide the interventional care they need immediately, then work our way down the list as fast as we can,” says Dr. Oyler. Based on the assessment by the triage nurse, the patient will either be:
- Taken to an exam room. If all rooms are full, that person will be next in line for a room. Dr. Oyler emphasizes that patients are not seen in the order of arrival, but based on the severity of their condition.
- Offered a fast-track service. The fast track does not have all of the capabilities of the emergency department, but is intended to help patients with minor emergencies get through the system. People in the waiting room may see other patients with minor injuries being called back before those with more serious injuries, but they are actually being treated in the fast-track area, Dr. Oyler explains.
Behind the waiting room doors
“A quiet waiting room is something we ideally love to have, but it is not a reflection of what is going on in the back,” says Dr. Oyler. “You can have one person or 20 people in your waiting room, but you could have complete chaos in the back with very, very sick patients.” Although the ED waiting room may not seem busy, the behind-the-scenes ambulance bay can bring in patients at all hours of the day. “You can have an incredibly long wait in our emergency department if you show up with a non-life-threatening condition that could have waited for treatment at your primary care physician’s office the next day,” he says. “We are sensitive to the fact that you are waiting,” says Dr. Oyler. “We want you to get back to a room and be seen as fast as possible, but we’re also prioritizing care for people who absolutely have to have it right then and there.” Dr. Oyler stresses the importance of patience if your illness or injury is not life-threatening. “We know you’re suffering and it’s not what we desire, but when your time comes, you’re going to get the service you wanted.” If your condition is not an emergency, you can save time and money by visiting an urgent care center or your primary care physician’s office. Insurance co-pays are usually more expensive at the emergency department compared to co-pays at other facilities. For more information on emergency services throughout the Piedmont system, visit our locations map to choose an emergency room near you .
Need to make an appointment with a Piedmont physician? Save time, book online .
- emergency department
- Emergency Medicine
- Jeffrey Oyler
- urgent care
Related Stories

Schedule your appointment online
Schedule with our online booking tool
*We have detected that you are using an unsupported or outdated browser. An update is not required, but for best search experience we strongly recommend updating to the latest version of Chrome, Firefox, Safari, or Internet Explorer 11+
Share this story
Download the Piedmont Now app
- Indoor Hospital Navigation
- Find & Save Physicians
- Online Scheduling
Download the app today!
- Medical Services
- Schedule an Appointment
- Children's Health
- Hollings Cancer Center
- Education at MUSC
- Research at MUSC
Emergency Department
What to expect.
If you are experiencing a life- or limb-threatening emergency, please call 911.
What to Expect During Your Emergency Department Visit

Information on know what to expect during your stay with us.
Welcome to the MUSC Emergency Department. Thank you for choosing us for your healthcare needs. We want to share some information with you so you will know what to expect during your stay with us.
When You Arrive
When you arrive, please sign in at the entrance desk. A technician will enter your information into the computer and take your vital signs including heart rate, blood pressure, oxygen level, and temperature.
We want to make sure you know that patients are not always seen in the order that they arrive to our emergency department. Our providers have to give priority to patients who are at higher risk of permanent injury, disability or death.
Initial Screening
As soon as possible, you will see a medical provider for initial screening. This may be a doctor, a nurse practitioner or a physician assistant, and a triage nurse. The provider will ask you questions about your illness or injury, review your medical history, and begin your treatment plan.
The phlebotomist/tech will see you next. This is the care team member who will start your iv, draw blood, collect additional samples.
The triage medical provider will then decide the best location for you to receive additional care. The nurse makes this decision based on your condition as well as on the condition and care of other patients being treated in the emergency department. You may not require placement in a monitored room. This will not affect the quality of the care that you receive.
Additional Care
Once you are placed in the best location for the kind of care you need, you will be evaluated further by additional care team members. Additional testing, treatments, and medications may be ordered.
You probably have questions about how long these additional tests and treatments may be expected to take.
- Blood work takes about 60 minutes to result once the lab has received your blood that was drawn.
- X-rays and CT scans may take 1-3 hours to be completed, depending on the number of patients who need these kinds of scans. Remember that people with life-threatening illness and injury may need them before you do.
- Sometimes it is necessary to consult with a specialty provider who doesn’t normally work in the emergency department. In this case, we have to contact the provider and make arrangements for the consultation. Consultations with other specialty providers vary by the type of provider and how emergent the situation is. This may take just a few minutes but may also take several hours depending on how busy the providers are treating other patients.
- Medications should be administered in a timely fashion but may have to be prepared in a pharmacy that is not in the emergency department.
Please rest assured that all the care team members in the emergency department are working as quickly and efficiently as possible to care for you and the other patients who need us. We understand that delays and uncertainty are difficult under any circumstances but especially difficult when you are not feeling well or in pain. Your Care Team Members will make every effort to keep you and your family updated on your plan of care. Please do not hesitate to ask for an update at any time. Thank you for partnering with us for your healthcare needs.

CDC: Emergency department visits for life-threatening conditions declined in pandemic’s early months

A new study released today by the Centers for Disease Control and Prevention shows emergency department visits dropped by 23% for heart attacks, 20% for strokes and 10% for hyperglycemic crises in first 10 weeks after the COVID-19 public health emergency declaration.
The study’s authors captured 73% of the nation’s ED visits from the CDC’s National Syndromic Surveillance Program and local partners and compared numbers from the Jan. 5-March 14 period to those from March 15 to May 23. The study’s authors said public health and health care professionals must publicly reinforce the importance of timely care for medical emergencies and give assurance that EDs are implementing infection prevention and control guidelines.
Related News Articles
- Research article
- Open access
- Published: 20 September 2021
Older patients’ perspectives on factors contributing to frequent visits to the emergency department: a qualitative interview study
- Daisy Kolk ORCID: orcid.org/0000-0003-1443-5323 1 , 2 ,
- Anton F. Kruiswijk 2 , 3 ,
- Janet L. MacNeil-Vroomen 2 ,
- Milan L. Ridderikhof 1 &
- Bianca M. Buurman 2 , 4
BMC Public Health volume 21 , Article number: 1709 ( 2021 ) Cite this article
2215 Accesses
13 Citations
1 Altmetric
Metrics details
Older patients are at high risk of unplanned revisits to the emergency department (ED) because of their medical complexity. To reduce the number of ED visits, we need more knowledge about the patient-level, environmental, and healthcare factors involved. The aim of this study was to describe older patients’ perspectives and experiences before and after an ED visit, and to identify factors that possibly contribute to frequent ED revisits.
This was a qualitative description study. We performed semi-structured individual interviews with older patients who frequently visited the ED and were discharged home after an acute visit. Patients were enrolled in the ED of a university medical centre using purposive sampling. Interviews were recorded, transcribed, and coded independently by two researchers. Theoretical analysis was used to identify recurring patterns and themes in the data. Interviews were conducted until thematic saturation was reached.
In-depth interviews were completed with 13 older patients. Three main themes emerged: 1) medical events leading to feelings of crisis, 2) patients’ untreated health problems, and 3) persistent problems in health and daily functioning post discharge. Participants identified problems before and after their ED visit that possibly contributed to further ED visits. These problems included increasing symptoms leading to feelings of crisis, the relationship with the general practitioner, incomplete discharge information at the ED, and inadequate follow-up and lack of recovery after an ED visit.
Conclusions
This qualitative study identified multiple factors that may contribute to frequent ED visits among older patients. Older patients in need of acute care might benefit from hospital-at-home interventions, or acute care provided by geriatric emergency teams in the primary care setting. Identifying frailty in the ED is needed to improve discharge communication and adequate follow-up is needed to improve recovery after an acute ED visit.
Peer Review reports
More than 18% of all emergency department (ED) visitors in the United States, like many other countries, are older than 65 years [ 1 ] and the number of older patients presenting to overcrowded EDs is increasing [ 2 , 3 ]. Older patients that frequently visit the ED have multiple chronic conditions, more severe illness, and more complex care questions [ 3 , 4 , 5 , 6 , 7 ]. Moreover, older patients are at high risk of unplanned revisits; more than 50% are discharged home from the ED [ 6 , 8 ] and approximately 10 to 23% have to return unexpectedly within the first month [ 5 , 6 , 9 ].
The complex care needs and unique challenges of older patients presenting to the ED often involve geriatric syndromes [ 9 ]. Geriatric syndromes like cognitive and functional impairment, falls, and malnutrition are highly prevalent among older patients [ 9 , 10 ] and may explain the need for frequent visits to the ED. However, geriatric syndromes often remain undiagnosed or undertreated, which increases the need for further ED visits [ 9 ].
The development of effective interventions to reduce ED visits among older patients is challenging [ 11 ]. Interventions focusing on discharge planning [ 12 ], transitional care [ 13 ], and phone calls after discharge [ 14 ] have not effectively reduced ED revisits. Developing effective interventions to prevent unplanned ED visits requires in-depth knowledge of patient-related, environmental, and healthcare-related factors. Given the complexity of these factors and the interaction between them, a qualitative approach is well suited for exploring this phenomenon.
The aim of this study was to describe the perspectives and experiences of older patients before and after a visit to the ED and to identify why these patients may have to return unexpectedly to the ED.
We utilized the Standards for Reporting of Qualitative Research [ 15 ], the criteria for reporting qualitative research (COREQ) [ 16 ], and the best practice guidelines to generate and report our findings [ 17 , 18 ].
Study design
We performed a qualitative description study [ 19 ], to provide a rich description of older patients’ perspectives and experiences before and after their visit to the ED and to identify possible contributing factors to unplanned revisits. This inductive approach is suitable for problem identification and hypothesis generation and is especially useful for research questions in health care because it helps to focus on the patients’ experiences and views on the health care system [ 20 ]. This method aims to provide a rich, straight description of perceptions and experiences and is founded in existing knowledge and clinical experiences of the research group, instead of other qualitative methods that are theory-driven [ 20 , 21 ]. We conducted semi-structured individual interviews which allow for a detailed in-depth exploration of the patient’s perceptions and experiences [ 22 ].
Study setting and population
Between June 2019 and September 2019 this study was conducted in the ED of a University Hospital’s Level I trauma center in the Netherlands, treating approximately 30.000 patients annually. The hospital had an accredited residency program in Emergency Medicine and the department is staffed by fully trained Emergency Physicians 24/7. When required, consultants of all medical specialties are available, including geriatrics. In this ED, approximately 46% of the older patients are discharged home by the treating physician, who decides what type of after care is needed (e.g., follow-up consultation; referral to the general practitioner or to an outpatient clinic).
Older patients (≥ 70 years) who frequently visited the ED and were discharged home after their last visit (the index visit) were eligible for inclusion. Further inclusion criteria were a medical history of two or more morbidities, and a previous visit to the ED or hospital during the past 18 months. Patients were ineligible if they were not able to speak Dutch sufficiently to perform the interview or were not able to give informed consent or perform the interview due to moderate/severe cognitive impairment judged by the treating physician. We used a purposive sampling method to identify relevant patients to interview, and to reach maximum variation in heterogeneity within this population regarding age, admission diagnosis, treating physician, and living situation [ 23 ]. All participants gave informed consent to take part in the study. The Institutional Review Board waived the need for approval under the Medical Research Involving Human Subjects Act.
Study protocol
One of two researchers (DK and AK) recruited participants and performed the interviews. DK is a clinical epidemiologist and PhD student in the department of Emergency Medicine and Geriatrics with formal qualitative research training. AK is a physician and worked as a research assistant in the ED. DK trained AK in qualitative research techniques. Neither interviewer was part of the participants’ medical care team.
Patients were recruited at the ED prior to or immediately after the discharge conversation. Patients were screened for eligibility by the treating physician and eligible patients were contacted by the study staff. The researcher informed the patient about the study, answered questions, ensured that the patient had comprehended the information and obtained informed consent. The researcher collected basic demographic information at the ED and an appointment for the interview was made. To minimize recall bias, interviews were conducted between 7 and 30 days after discharge [ 24 ]. Interviews lasted approximately 90 min and took place face-to-face at the participant’s home to ensure their privacy and comfort. Family members or informal caregivers of the participant were allowed to participate.
The interview guide consisted of a topic list and open-ended questions that were formulated based on a literature search and (clinical) experiences of senior researchers, emergency physicians, geriatricians, and nurses. The complete interview guide is shown is an additional file (see Additional file 1 ). The interview guide was pilot-tested and was iteratively revised during the interview process. All interviews were voice-recorded and transcribed verbatim by the research staff. During the interview the researcher took field notes for recall of the context. Given this specific population, transcripts were not returned to the participants and participants were not asked to provide feedback on the findings afterwards, but the interview was verbally summarized and discussed immediately with the participant after the interview.
Data analysis
We used theoretical analysis, a type of thematic analysis used when the researcher has some pre-understanding of the topic, to identify, analyse and report patterns in the data and formulate themes [ 25 ]. DK and AK independently generated initial themes using an inductive open-coding approach, by highlighting meaningful sentences in the text and coding all relevant topics. After the initial coding, DK and AK reread all coded data to identify patterns. Patterns were compared between interviews to reach a conclusion about main themes throughout the interviews. During the analysis, we remained open to the possibility of new categories coming up, and thoughts and changes in the coding scheme were discussed thoroughly within the research team. Finally, a list of relevant main themes with subthemes was created and the results were described in detail, illustrated with extracts from the transcripts. We conducted interviews until theoretical data saturation was reached [ 26 ]. The Computer Assisted Qualitative Data Analysis program (MaxQDA) was used to code and manage the qualitative data [ 27 ]. During this process, memo’s and manual version control were used to increase the auditability.
Thirteen participants completed the interviews, and thematic saturation was reached after nine interviews. Thirty-two older patients were screened for eligibility; 23 were eligible and asked to participate. Four patients were not interested in research in general and two felt too ill to give informed consent. Seventeen older patients gave informed consent, but eventually four of these patients felt too ill to be interviewed and withdrew their informed consent. Table 1 presents the characteristics of the 13 participants. They had a mean (SD) age of 75 (6), ranging from 70 to 91 years, a median (IQR) number of 4 (3–4.5) comorbidities, and 7 (54%) participants had their informal caregiver involved in the interview.
Based on the thematic analysis of the interviews, three main themes emerged: 1) medical events leading to feelings of crisis; 2) patients’ untreated health problems; and 3) persistent problems in health and daily functioning post discharge. Table 2 summarizes the themes and provides illustrative quotes. Figure 1 summarizes the conceptual model that was constructed based on the identified themes.
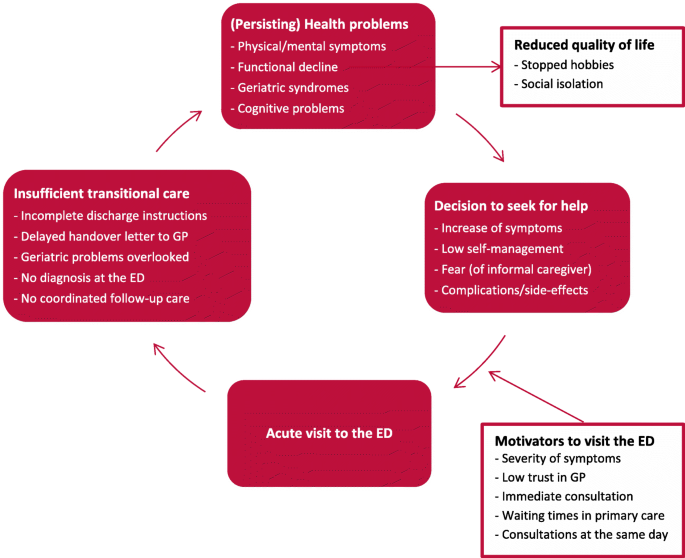
Possible contributing factors to frequent ED visits based on reported patient experiences. ED, emergency department; GP, general practitioner
Theme 1 – medical events leading to feeling of crisis
We identified two categories that came up in most interviews regarding events leading up to the index visit: 1) the decision to seek medical care, and 2) motivators to visit the ED.
Decision to seek medical care
In most participants, health problems and symptoms were already present for several weeks or months before the current ED visit. Some of them had visited the ED recurrently for the same symptoms before the index visit. Some participants said that the index visit was a result of escalation as they suddenly experienced an increase in severity of symptoms for a longer period, as participant 1 (female, 71) recounted: “So first I was just waiting and then I was just thinking whether this would take care of itself or would these symptoms persist? I wanted to wait two weeks, but then I just felt so sick. So then I just thought I will just call the doctor [medical specialist].” Or participants or their informal caregivers were afraid of an increase in symptom severity, or they did not know how to handle the symptoms anymore. They thought it was inevitable to present to the ED. This was true for participant 5 (female, 70), who recounted, “It is getting so bad, I really don’t know what to do. I have never been so sick and used so much medication. I really panicked: what is happening to me?” In other cases, participants decided to visit the ED after an unexpected acute situation, like a fall, as participant 8 (male, 91) said, “I have had falls, but not as bad as this. There was a puddle of blood, and it was not stopping because of my blood thinners.” Some participants described that they were clearly instructed by their treating medical specialist to go to the ED if a particular symptoms occurred after a medical intervention. In some cases, this occurred several times. For example, participant 12 (female, 82) recounted, “I was discharged home and instructed to come back if I had a fever. So, we went to the ED when I had a fever, but they could not find anything. So I was sent home and the fever returned. I went back to the ED several times as the doctor told me to.”
Motivators to visit the ED
Participants most frequently mentioned logistic or organizational aspects in their decision to visit the ED instead of initially referring to other healthcare services. There were many underlying thoughts and opinions related to their situations. Some participants decided to visit the ED by themselves, because they experienced before that they needed specific diagnostics after a fall. For example, participant 11 recounted: “By every fall, you never know what you have. You never know if something is broken, so you have to go to the ED to get X-rays taken.” In other cases, participants experienced symptoms for a longer period but decided to visit the ED as they thought waiting times in the outpatient clinic or general practice would be too long for consultation and diagnostics. Even though they had waited a long time at the ED before, they still went there because they wanted a consultation including ancillary testing on the same day. Some participants who were vulnerable or had a small social network said that visiting the ED once was less of a burden than visiting the outpatient clinic several times. For example, participant 3 (female, 73) had experienced symptoms for a long time and was not in good physical condition. Her informal caregiver recounted, “Yes, I called the outpatient clinic to talk to her treating medical specialist. And he advised us that it was more efficient to go to the ED, otherwise we would have to make several outpatient appointments to get same care and that would be far too burdensome.”
When asked why they visited the ED, many participants mentioned their relationship with their general practitioner (GP) and recounted a wide array of experiences. Many patients described that they had a good relationship with their GP but felt that they needed the expert opinion of their medical specialist because of their particular conditions. Others described past experiences that diminished their confidence in their GP, such as participant 5 (female, 70), who said, “I don’t expect anything from my new GP. When I see the GP, I sit down, I say what the problem is; and then nothing happens. I would like to have new one, but the waiting lists are too long.”
Theme 2 – patients’ untreated health problems
Two categories emerged under this theme: 1) discharge from the ED, and 2) follow-up and continuity of care.
Discharge from the ED
The majority of the participants indicated that they were happy to be discharged home after often a whole day in the ED. Many participants felt stressed at the time of the ED visit, and could not remember all the details after being discharged. In particular, those who did not receive a clear diagnosis stated that they would like to talk about their health problems some days after the ED visit, when they were less stressed. Some participants described visiting the ED with severe symptoms and being discharged without a diagnosis. They felt temporarily reassured, but then felt insecure back at home because their symptoms were unresolved. These patients felt frustrated because they did not receive further information at discharge, as participant 3 (female, 72) described: “They [ED doctors] didn’t say that much. I do not even know if I got a discharge letter. No, I did not! All they said was ‘Madam, we did not find anything wrong with you.’ Then they said, ‘Your GP will do further follow-up.’ Or maybe they said the medical specialist.”
Some participants felt the focus in the ED was solely on somatic care, even though they also needed psychological support and practical help. Participant 8 (male, 91) said that he was alone in the ED and was told he would be discharged in the late evening. He felt unsatisfied because he did not receive any help arranging his discharge. Many participants felt the information at discharge was incomplete. One informal caregiver described that they received a lot of verbal information, but could not remember it all after discharge. This informal caregiver said that written information at discharge would have been more helpful and would have reduced the stress they felt in the ED at not understanding everything they were told. This was less of a problem for the two participants who visited the ED with cancer-related medical problems. They said they received very good cancer-related care in specific care pathways. Because they were already familiar with their diagnosis and had follow-up appointments with their medical specialist, they felt less need for a comprehensive conversation at discharge. For example, participant 6 (male, 70) recounted: “I did have meetings with the palliative care team, and they called again today. Together with the palliative care team, my GP, and my oncologist in the hospital. As I already had regularly scheduled check-ups, an appointment for follow-up care after my ED admission was not necessary. I did not need any comprehensive discharge instructions as I know how everything works already.”
Follow-up and continuity of care
Many participants said that a follow-up appointment was quickly arranged after discharge. They felt reassured by their post-discharge appointment and the medical follow-up it provided. Many participants felt the need for more information and had many questions for their physician. In cases where follow-up was not arranged, patients felt stressed or unsafe. Moreover, participants also felt they needed to participate actively in their own care, as the informal caregiver of participant 4 (female, 72) explained: “You really need to think for yourself; otherwise something could be forgotten or missed in your patient file. But you have to figure that out yourself the hard way. If you are cognitively impaired and are on your own, then you are really vulnerable.” Some participants also said that they called their physician soon after discharge when symptoms increased. One participant described that she went to see her GP, but was referred back to the ED because the GP had not received the discharge letter after the last ED visit.
Most patients with a diagnosis of cancer said that a follow-up appointment with their medical specialist was already planned before the index visit. They often felt that their frequent visits to the ED were minor events in their declining health and were part of their illness. Participant 9 (female, 72 years) stated: “A visit to the ED is an accepted part of the process in my declining health. With cancer it is inevitable.”
Theme 3 – persistent problems in health and daily functioning post discharge
Within this theme, two categories emerged: 1) physical and mental symptoms, and 2) effects on daily life.
Physical and mental symptoms
All participants described that increasing symptoms negatively affected their physical and mental health. Some participants felt that the index visit did not resolve their current health problems, and usually ended up back at the ED, where they did not receive a diagnosis. This resulted in persisting symptoms and concern, unless serious diseases were excluded. Participant 1 (female, 71) recalled: “After the ED visit, I thought to myself ‘I still have the same symptoms.’ Then I started to second-guess the advice of the ED and I wondered if they had missed something. And then I really started to worry and just kept on worrying.”
After they were discharged from the ED, participants experienced problems with recovery and reported several physical and psychological problems. Most of these health problems were already present prior to the ED visit, however, more than half of the participants mentioned new problems that occurred after leaving the ED. When asked about their problems, they mentioned several symptoms like decreased appetite, loss of muscle strength, fear of falling, and fatigue. Participant 8 (male, 91) described his recovery after his last ED visit: “I know I really must eat, as I already lost 10 pounds. I am doing the best I can. In the morning and in the afternoons, I have more appetite. However, at dinnertime I just cannot eat. I am afraid to fall if I go outside. I always take my cane to go to the garage. It is not easy, but it gives me some security.”
Effects on daily life
The majority of participants described that they experienced problems in their daily functioning and were not able to resume all their usual activities because of their health problems. They recounted a decline in functioning before their recent ED visit, for example after a previous hospital admission. Many participants felt that the index visit had not improved their current health problems nor their functionality. They were disappointed because they expected their symptoms to decrease and their physical functioning to increase. Participant 6 (male, 70) described: “I cannot do anything. No, I can walk a bit. I sit a lot. Vacuuming, cleaning, that sort of things, I cannot do that. Yes of course, I am not happy about it. I do not see any progression in my recovery, and I expected that. Because, until now … so far things are not so positive.” Some participants believed that ageing and their declining health were responsible for their frequent ED visits and functional decline, as participant 8 (male, 91) described: “That’s what happens when you get older. It is like a snowman, you just melt away with time and that is hard to accept. You just keep on declining.”
Some participants felt that their symptoms and functional decline affected their quality of life. For example, the informal caregiver of participant 5 (female, 70) recounted that his mother was not able to go outside anymore because she had lost functional ability, resulting in social isolation which negatively affected her mental health. The informal caregiver said: “I think it would be better for her to move to a place with an elevator and where she can use a scooter or something. Then it is easier for her to go outside and to the local city centre. Now she is stuck inside worrying the entire day. She would be happier if she could go outside and find some nice distractions.”
Many participants also recounted that frequent hospital visits caused a lot of stress and energy loss. Older informal caregivers described that ED visits caused an overload as they had to arrange everything unexpectedly in a very short time and they felt very insecure. Participant 12 (female, 82) recounted that she and her partner gave up their hobby after so many stressful hospital visits: “We gave up Nordic walking even though we love it. With all those ED visits, we are exhausted and it is too difficult for my husband. We have been so many times to the hospital for ED and outpatient visits. We are just so burnt out from it all.”
Through in-depth interviews, we identified three major themes related to older adults’ experiences before and after an ED visit: 1) medical events leading to feelings of crisis, 2) patients’ untreated health problems, and 3) persisting health problems in health and daily functioning post discharge. This in-depth description of the events leading up to an ED visit and the lack of recovery after discharge highlights potential reasons for ED revisits. These findings may improve future interventions in older patients who frequently visit the ED, and may help reduce the number of ED revisits.
Before their ED visit, most patients were experiencing symptoms that had been present for several weeks or months. These symptoms suddenly increased in severity, causing anxiety and compelling the patients to seek urgent help [ 28 ]. They felt that they were not able to control their symptoms and could no longer manage their situation, so made an acute visit to the ED. In some older patients, lower levels of self-efficacy and self-management seemed to play a role, which is a major problem among older patients with multiple chronic illnesses [ 29 ]. These results suggest that the escalation of symptoms before the ED visit could have been prevented if the patients’ symptoms were managed earlier on. When asked about ways to prevent new ED visits, some patients mentioned that they trusted the care in the ED more than they trusted the care from their GP. Trust in a very important component of the doctor-patient relationship [ 30 ] and previous studies have shown that a good relationship with the GP and greater continuity of primary care reduces ED visits in older patients [ 31 , 32 , 33 ]. An important determinant of older patients’ trust in the GP is the sense of shared-decision making [ 34 ]. In the Netherlands, the GP holds a central role in primary healthcare including care for older patients [ 35 ]. Therefore, it is especially important to educate GPs on the complex care needs of older patients [ 36 ]. However, older patients often need different healthcare services [ 2 ], so case management and hospital care at home would help GPs to reduce ED visits. For example, specialized geriatric medical emergency teams with access to diagnostics could provide high-quality care to patients in their own home, thereby reducing the need for ED visits [ 37 ].
After treatment in the ED, all patients included in this study were discharged home. They all agreed to be discharged, but found it very difficult to manage the transition to home life. They found their ED visit stressful [ 38 ] and did not receive the information they needed at discharge [ 39 ]. Especially in older patients with limited health literacy, incomplete information at discharge may not meet the patient’s needs [ 40 ]. Our participants reported that care in the ED was focused on somatic treatment, and failed to meet all of their needs. Previously, it has been suggested that current disease-oriented and episodic models of emergency care do not adequately meet the complex care needs of frail older patients [ 2 ]. Identifying frailty in the ED is a major problem in caring for older adults [ 41 ], but is important for a fully informative discharge and for adequate follow-up to prevent further decline [ 11 , 41 , 42 ]. For example, any cognitive impairment should be stated in the discharge letter because it increases the chance of readmission after discharge [ 43 ]. All physicians working with older patients in the ED need to be trained in geriatric competencies [ 44 , 45 ], and older patients that frequently visit the ED should consult a geriatrician [ 44 , 46 ]. Moreover, trained nurses specializing in the complex care needs of older patients may improve care transitions, effectively reducing functional decline and hospital admissions [ 47 , 48 ].
Older patients who were discharged home without a specific diagnosis experienced physical and mental problems that persisted or even increased. These patients felt reassured at discharge but started worrying when they were back home and needed proper follow-up. Moreover, many of these patients experienced common post-hospital symptoms after discharge [ 10 , 49 ]. Most patients had experienced functional decline before visiting the ED, and did not feel they had recovered to their baseline level after discharge. Older patients have a high risk of functional decline after being discharged from the ED [ 8 , 50 ], and more than half of older patients need help with rehabilitation after discharge [ 51 ]. Based on what our participants described, we concluded that patients were passively waiting for recovery and did not consider asking for help with rehabilitation. However, a previous qualitative study [ 38 ] showed that older patients who seek emergency care have a strong desire for functional recovery. They expected that their functional difficulties would be addressed in the ED, but realized at discharge that the ED was not the right place for improving functionality and health-related quality of life. These findings are in line with our results; it seems that patients do not fully understand what care the ED provides. According to geriatric emergency department guidelines, to decrease revisits and improve quality of care for geriatric patients, the ED should improve transition care at discharge through comprehensive discharge conversations, written discharge instructions that can be understood by older patients, and a follow-up plan that includes post-discharge care [ 44 ].
Implications for practice and research
According to older patients’ experiences, medical events leading to feelings of crises and a lower trust in the care of the GP played a role in their decision to visit the ED. After discharge, older patients experienced issues such as untreated health problems, insufficient discharge instructions, inadequate follow-up, and a lack of recovery, which may play a role in future acute care needs and new ED admissions. Given the problems identified in this study, we hypothesize that greater continuity of primary care including the identification of frailty and complex care needs, and an adequate assessment and management of symptoms by the GP or by a health care professional educated in geriatric care, may reduce the onset of crisis, and new ED admissions [ 36 , 37 ]. In addition, comprehensive discharge instructions from the ED, a structured care pathway for patients with multiple chronic conditions, and hospital-at-home interventions may also reduce the onset of new crises and ED revisits [ 52 , 53 ].
Moreover, we found that comprehensive discharge instructions and after care were not required for patients who were already in a specific care pathway for cancer treatment, as their home care and follow-up meetings had been pre-arranged. Geriatric patients with multiple chronic conditions may benefit from such an organized care pathway, but further research is needed to develop an effective geriatric care pathway that will reduce the number of ED revisits among older patients [ 46 , 51 , 54 ].
Limitations
Patients were recruited in a university hospital, so our results might not be generalizable to patients being treated in secondary hospitals who likely have less complex conditions and other problems and perspectives. Moreover, we noticed that patients who were more fatigued by their ED visit declined to participate, so we did not obtain the perspectives of more vulnerable patients in our study. Furthermore, although all patients were interviewed within 4 weeks after their ED visit, recall bias may have occurred, i.e., patients might not have remembered all the details and experiences before their ED visit. However, we believe this effect is likely to be minimal.
Conclusions and implications
This qualitative study identified multiple factors that may contribute to frequent ED revisits and provides insight into the perspectives and experiences of older patients. This can be useful in the development of effective interventions to reduce the need for emergency care in older patients. The identified factors included escalating feelings of crisis when symptoms increase, a poor relationship with the GP, incomplete information at discharge from the ED, and untreated, persistent health problems, inadequate follow-up and lack of recovery after an ED visit. To reduce feelings of crises and subsequent ED admissions, older patients might benefit from hospital-at-home interventions [ 52 , 53 ], which can be provided by geriatric emergency teams. Identifying frailty in the ED is important for proper communication at discharge and adequate follow-up after an acute ED visit. In conclusion, our findings provide a sound basis for future studies investigating interventions to reduce the need for emergency care in older patients.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available as this could potentially compromise participant privacy. Study participants consented to interviews with the understanding that their data would remain anonymous and confidential, and would not be shared beyond the researchers. The codebook generated during the analysis is available from the corresponding author on reasonable request.
Abbreviations
Emergency department
Consolidated criteria for reporting qualitative research
Computer assisted qualitative data analysis program
General practitioner
Hooker EA, Mallow PJ, Oglesby MM. Characteristics and trends of emergency department visits in the United States (2010-2014). The Journal of emergency medicine. 2019;56(3):344–51. https://doi.org/10.1016/j.jemermed.2018.12.025 .
Article PubMed Google Scholar
Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238–47. https://doi.org/10.1067/mem.2002.121523 .
Pines JM, Asplin BR, Kaji AH, Lowe RA, Magid DJ, Raven M, et al. Frequent users of emergency department services: gaps in knowledge and a proposed research agenda. Acad Emerg Med Off J Soc Acad Emerg Med. 2011;18(6):e64–9. https://doi.org/10.1111/j.1553-2712.2011.01086.x .
Article Google Scholar
Arendts G, Etherton-Beer C, Jones R, Bullow K, MacDonald E, Dumas S, et al. Use of a risk nomogram to predict emergency department reattendance in older people after discharge: a validation study. Intern Emerg Med. 2015;10(4):481–7. https://doi.org/10.1007/s11739-015-1219-3 .
Biese K, Massing M, Platts-Mills TF, Young J, McArdle J, Dayaa JA, et al. Predictors of 30-Day Return Following an Emergency Department Visit for Older Adults. N C Med J. 2019;80(1):12–8. https://doi.org/10.18043/ncm.80.1.12 .
de Gelder J, Lucke JA, de Groot B, Fogteloo AJ, Anten S, Heringhaus C, et al. Predictors and outcomes of revisits in older adults discharged from the emergency department. J Am Geriatr Soc. 2018;66(4):735–41. https://doi.org/10.1111/jgs.15301 .
Friedmann PD, Jin L, Karrison TG, Hayley DC, Mulliken R, Walter J, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19(2):125–9. https://doi.org/10.1053/ajem.2001.21321 .
Article CAS PubMed Google Scholar
Nagurney JM, Fleischman W, Han L, Leo-Summers L, Allore HG, Gill TM. Emergency department visits without hospitalization are associated with functional decline in older persons. Ann Emerg Med. 2017;69(4):426–33. https://doi.org/10.1016/j.annemergmed.2016.09.018 .
Article PubMed PubMed Central Google Scholar
Costa AP, Hirdes JP, Heckman GA, Dey AB, Jonsson PV, Lakhan P, et al. Geriatric syndromes predict postdischarge outcomes among older emergency department patients: findings from the interRAI multinational emergency department study. Acad Emerg Med Off J Soc Acad Emerg Med. 2014;21(4):422–33. https://doi.org/10.1111/acem.12353 .
van Seben R, Reichardt LA, Aarden JJ, van der Schaaf M, van der Esch M, Engelbert RHH, et al. The course of geriatric syndromes in acutely hospitalized older adults: the hospital-ADL study. J Am Med Dir Assoc. 2019;20(2):152–8 e2. https://doi.org/10.1016/j.jamda.2018.08.003 .
Hastings SN, Heflin MT. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med Off J Soc Acad Emerg Med. 2005;12(10):978–86. https://doi.org/10.1197/j.aem.2005.05.032 .
Guttman A, Afilalo M, Guttman R, Colacone A, Robitaille C, Lang E, et al. An emergency department-based nurse discharge coordinator for elder patients: does it make a difference? Acad Emerg Med Off J Soc Acad Emerg Med. 2004;11(12):1318–27. https://doi.org/10.1197/j.aem.2004.07.006 .
Verhaegh KJ, MacNeil-Vroomen JL, Eslami S, Geerlings SE, de Rooij SE, Buurman BM. Transitional care interventions prevent hospital readmissions for adults with chronic illnesses. Health Aff (Millwood). 2014;33(9):1531–9. https://doi.org/10.1377/hlthaff.2014.0160 .
Biese KJ, Busby-Whitehead J, Cai J, Stearns SC, Roberts E, Mihas P, et al. Telephone follow-up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66(3):452–8. https://doi.org/10.1111/jgs.15142 .
O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/acm.0000000000000388 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Choo EK, Garro AC, Ranney ML, Meisel ZF, Morrow GK. Qualitative research in emergency care part I: research principles and common applications. Acad Emerg Med Off J Soc Acad Emerg Med. 2015;22(9):1096–102. https://doi.org/10.1111/acem.12736 .
Ranney ML, Meisel ZF, Choo EK, Garro AC, Sasson C, Morrow GK. Interview-based qualitative research in emergency care part II: data collection, analysis and results reporting. Acad Emerg Med Off J Soc Acad Emerg Med. 2015;22(9):1103–12. https://doi.org/10.1111/acem.12735 .
Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40. https://doi.org/10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g .
Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description - the poor cousin of health research? BMC Med Res Methodol. 2009;9(1):52. https://doi.org/10.1186/1471-2288-9-52 .
Sandelowski M. What's in a name? Qualitative description revisited. Res Nurs Health. 2010;33(1):77–84. https://doi.org/10.1002/nur.20362 .
DeJonckheere M, Vaughn LM. Semistructured interviewing in primary care research: a balance of relationship and rigour. Fam Med Community Health. 2019;7(2):e000057. https://doi.org/10.1136/fmch-2018-000057 .
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Admin Pol Ment Health. 2015;42(5):533–44. https://doi.org/10.1007/s10488-013-0528-y .
Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43(1):87–91. https://doi.org/10.1016/0895-4356(90)90060-3 .
Percy WH, Kostere K, Kostere S. Generic qualitative research in psychology. Qual Rep. 2015;20(2):76–85.
Google Scholar
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. https://doi.org/10.1007/s11135-017-0574-8 .
VERBI-Software. MAXQDA 2018. Berlin: VERBI Software; 2017.
Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient's perspective. Emergency medicine journal : EMJ. 2001;18(6):430–4. https://doi.org/10.1136/emj.18.6.430 .
Article CAS PubMed PubMed Central Google Scholar
Gallagher R, Donoghue J, Chenoweth L, Stein-Parbury J. Self-management in older patients with chronic illness. Int J Nurs Pract. 2008;14(5):373–82. https://doi.org/10.1111/j.1440-172X.2008.00709.x .
Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–39, v. https://doi.org/10.1111/1468-0009.00223 .
Henninger S, Spencer B, Pasche O. Deciding whether to consult the GP or an emergency department: a qualitative study of patient reasoning in Switzerland. Eur J Gen Pract. 2019;25(3):136–42. https://doi.org/10.1080/13814788.2019.1634688 .
Ionescu-Ittu R, McCusker J, Ciampi A, Vadeboncoeur AM, Roberge D, Larouche D, et al. Continuity of primary care and emergency department utilization among elderly people. CMAJ. 2007;177(11):1362–8. https://doi.org/10.1503/cmaj.061615 .
Rosenblatt RA, Wright GE, Baldwin LM, Chan L, Clitherow P, Chen FM, et al. The effect of the doctor-patient relationship on emergency department use among the elderly. Am J Public Health. 2000;90(1):97–102. https://doi.org/10.2105/ajph.90.1.97 .
Croker JE, Swancutt DR, Roberts MJ, Abel GA, Roland M, Campbell JL. Factors affecting patients' trust and confidence in GPs: evidence from the English national GP patient survey. BMJ Open. 2013;3(5). doi: https://doi.org/10.1136/bmjopen-2013-002762 .
Schellevis FG, Westert GP, De Bakker DH. The actual role of general practice in the dutch health-care system. Results of the second dutch national survey of general practice. Med Klin (Munich). 2005;100(10):656–61. https://doi.org/10.1007/s00063-005-1090-5 .
Moriarty JP, Wu BJ, Blake E, Ramsey CM, Kumar C, Huot S, et al. Assessing resident attitudes and confidence after integrating geriatric education into a primary care resident clinic. Am J Med. 2018;131(6):709–13. https://doi.org/10.1016/j.amjmed.2018.03.001 .
Low LF, Yap M, Brodaty H. A systematic review of different models of home and community care services for older persons. BMC Health Serv Res. 2011;11(1):93. https://doi.org/10.1186/1472-6963-11-93 .
Dresden SM, McCarthy DM, Engel KG, Courtney DM. Perceptions and expectations of health-related quality of life among geriatric patients seeking emergency care: a qualitative study. BMC Geriatr. 2019;19(1):209. https://doi.org/10.1186/s12877-019-1228-6 .
Nielsen LM, Gregersen Ostergaard L, Maribo T, Kirkegaard H, Petersen KS. Returning to everyday life after discharge from a short-stay unit at the emergency department-a qualitative study of elderly patients' experiences. Int J Qual Stud Health Well-being. 2019;14(1):1563428. https://doi.org/10.1080/17482631.2018.1563428 .
Samuels-Kalow M, Rhodes K, Uspal J, Reyes Smith A, Hardy E, Mollen C. Unmet needs at the time of emergency department discharge. Acad Emerg Med Off J Soc Acad Emerg Med. 2016;23(3):279–87. https://doi.org/10.1111/acem.12877 .
Brouwers C, Merten H, Willems M, Habraken DJ, Bloemers FW, Biesheuvel TH, et al. Improving care for older patients in the acute setting: a qualitative study with healthcare providers. Neth J Med. 2017;75(8):335–43.
CAS PubMed Google Scholar
Frumkin K. Toppling oranges: death, disability, decline, and readmission of community-dwelling elderly patients after an emergency department visit. The Journal of emergency medicine. 2020;58(2):339–45. https://doi.org/10.1016/j.jemermed.2019.12.014 .
Lucke JA, de Gelder J, Heringhaus C, van der Mast RC, Fogteloo AJ, Anten S, et al. Impaired cognition is associated with adverse outcome in older patients in the emergency department; the acutely presenting older patients (APOP) study. Age Ageing. 2018;47(5):679–84. https://doi.org/10.1093/ageing/afx174 .
Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7–25. doi: https://doi.org/10.1016/j.annemergmed.2014.02.008 .
Hogan TM, Losman ED, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med Off J Soc Acad Emerg Med. 2010;17(3):316–24. https://doi.org/10.1111/j.1553-2712.2010.00684.x .
Liberman T, Roofeh R, Sohn N, Brave M, Smith A, Willis H, et al. The GAP-ED project: improving Care for Elderly Patients Presenting to the emergency department. The Journal of emergency medicine. 2020;58(2):191–7. https://doi.org/10.1016/j.jemermed.2019.10.006 .
Hwang U, Dresden SM, Rosenberg MS, Garrido MM, Loo G, Sze J, et al. Geriatric emergency department innovations: transitional care nurses and hospital use. J Am Geriatr Soc. 2018;66(3):459–66. https://doi.org/10.1111/jgs.15235 .
Wallis M, Marsden E, Taylor A, Craswell A, Broadbent M, Barnett A, et al. The geriatric emergency department intervention model of care: a pragmatic trial. BMC Geriatr. 2018;18(1):297. https://doi.org/10.1186/s12877-018-0992-z .
van Seben R, Reichardt LA, Essink DR, van Munster BC, Bosch JA, Buurman BM. "I feel worn out, as if I neglected myself": older Patients' perspectives on post-hospital symptoms after acute hospitalization. The Gerontologist. 2019;59(2):315–26. https://doi.org/10.1093/geront/gnx192 .
de Gelder J, Lucke JA, Blomaard LC, Booijen AM, Fogteloo AJ, Anten S, et al. Optimization of the APOP screener to predict functional decline or mortality in older emergency department patients: cross-validation in four prospective cohorts. Exp Gerontol. 2018;110:253–9. https://doi.org/10.1016/j.exger.2018.06.015 .
Nielsen LM, Maribo T, Kirkegaard H, Petersen KS, Lisby M, Oestergaard LG. Effectiveness of the "elderly activity performance intervention" on elderly patients' discharge from a short-stay unit at the emergency department: a quasi-experimental trial. Clin Interv Aging. 2018;13:737–47. https://doi.org/10.2147/CIA.S162623 .
Levine DM, Ouchi K, Blanchfield B, Saenz A, Burke K, Paz M, et al. Hospital-level Care at Home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77–85. https://doi.org/10.7326/m19-0600 .
Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):Cd007491. https://doi.org/10.1002/14651858.CD007491.pub2 .
Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15(9):1107–17. https://doi.org/10.1111/ggi.12538 .
Download references
Acknowledgements
Not applicable.
No specific funding was received for this study.
Author information
Authors and affiliations.
Amsterdam UMC, University of Amsterdam, Emergency Medicine, Amsterdam Movement Sciences, Meibergdreef 9, Amsterdam, Netherlands
Daisy Kolk & Milan L. Ridderikhof
Internal Medicine, Section of Geriatric Medicine, Amsterdam UMC, University of Amsterdam, Internal Medicine, Section of Geriatric Medicine, Amsterdam Public Health, Meibergdreef 9, Amsterdam, Netherlands
Daisy Kolk, Anton F. Kruiswijk, Janet L. MacNeil-Vroomen & Bianca M. Buurman
OLVG Hospital, Department of Geriatric Medicine, Amsterdam, the Netherlands
Anton F. Kruiswijk
ACHIEVE - Centre of Applied Research, Faculty of Health, Amsterdam University of Applied Sciences, Amsterdam, Netherlands
Bianca M. Buurman
You can also search for this author in PubMed Google Scholar
Contributions
DK, AK, JMV, MLR, and BB made substantial contributions to the conception and design of the work. DK and AK did the data acquisition. DK, AK, JMV, MLR, and BB were involved in the analysis and did the interpretation of data. DK and AK did the drafting and DK, AK, JMV, MLR, and BB did the revisions. DK, AK, JMV, MLR, and BB did the final approval of the version to be published.
Corresponding author
Correspondence to Daisy Kolk .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This is a qualitative study. The Institutional Review Board of the Amsterdam UMC in Amsterdam, the Netherlands waived the need for approval under the Medical Research Involving Human Subjects Act (Reg. No. W19_270). Written informed consent wat obtained from all individual participants included in this study.
Consent for publication
No identifiable data is included in this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kolk, D., Kruiswijk, A.F., MacNeil-Vroomen, J.L. et al. Older patients’ perspectives on factors contributing to frequent visits to the emergency department: a qualitative interview study. BMC Public Health 21 , 1709 (2021). https://doi.org/10.1186/s12889-021-11755-z
Download citation
Received : 17 September 2020
Accepted : 08 September 2021
Published : 20 September 2021
DOI : https://doi.org/10.1186/s12889-021-11755-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient experiences
- Qualitative research
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Real-World Management of Hyperkalemia in the Emergency Department: An Electronic Medical Record Analysis
- Original Research
- Open access
- Published: 27 December 2021
- Volume 39 , pages 1033–1044, ( 2022 )
Cite this article
You have full access to this open access article
- Jill Davis 1 ,
- Rubeen Israni 1 ,
- Keith A. Betts 2 ,
- Fan Mu ORCID: orcid.org/0000-0003-0252-0387 2 ,
- Erin E. Cook 2 ,
- Deborah Anzalone 1 ,
- Harold Szerlip 3 ,
- Lei Yin 2 ,
- Gabriel I. Uwaifo 4 &
- Eric Q. Wu 2
2804 Accesses
2 Citations
1 Altmetric
Explore all metrics
Introduction
Hyperkalemia is often managed in the emergency department (ED) and it is important to understand how ED management and post-discharge outcomes vary by hyperkalemia severity. This study was conducted to characterize ED management and post-discharge outcomes across hyperkalemia severities.
Adults with an ED visit with hyperkalemia (at least one serum potassium lab measure above 5.0 mEq/L) were selected from US electronic medical record data (2012–2018). Patient characteristics, potassium levels, treatments, and monitoring prior to and during the ED visit were compared by hyperkalemia severity (mild [> 5.0–5.5 mEq/L], moderate [> 5.5–6.0], severe [> 6.0]) using unadjusted analyses. Death, immediate inpatient admission, 30-day hyperkalemia recurrence, and 30-day inpatient admission were also assessed by severity.
Of 6222 patients included, 4432 (71.2%) had mild hyperkalemia, 1085 (17.4%) had moderate, and 705 (11.3%) had severe hyperkalemia. Chronic kidney disease (39.9–50.1%) and heart failure (21.6–24.3%) were common. In the ED, electrocardiograms (mild, 56.5%; moderate, 69.6%; severe, 81.0%) and patients with at least two potassium laboratory values increased with severity (15.0%; 40.4%; 75.5%). Among patients with at least two potassium laboratory values, over half of patients (60.4%) had potassium levels ≤ 5.0 mEq/L prior to discharge. Use of potassium-binding treatments (sodium polystyrene sulfonate: mild = 4.1%; moderate = 17.1%; severe = 27.4%), temporizing agents (5.6%; 15.5%; 31.6%), or dialysis (0.4%; 0.8%; 3.0%) increased with severity; treatment at discharge was not common. Death (1.1%; 3.7%; 10.6%), immediate admission to inpatient care (5.8%; 8.7%; 12.7%), 30-day hyperkalemia recurrence (2.9%; 19.0%; 32.5%), 30-day inpatient admission with hyperkalemia (6.5%; 7.9%; 9.3%) also increased with severity.
Patients with moderate and severe hyperkalemia experienced elevated risk of hyperkalemia recurrence and hyperkalemia-related inpatient readmission following discharge from the ED from a descriptive analysis. Future research to assess strategies to reduce hyperkalemia recurrence and inpatient admission in this patient population would be beneficial.
Similar content being viewed by others
Epidemiology and health outcomes associated with hyperkalemia in a primary care setting in England
Laura Horne, Akhtar Ashfaq, … James B. Wetmore

The burden of hyperkalemia in Germany – a real world evidence study assessing the treatment and costs of hyperkalemia
Jennifer Scarlet Haas, Kim-Sarah Krinke, … Sebastian Braun
Real-world clinical burden and economic assessment associated with hyperkalaemia in a large integrated healthcare system: a retrospective analysis
Joseph B. Muhlestein, Jennifer Kammerer, … Heidi T. May
Avoid common mistakes on your manuscript.
Hyperkalemia is an electrolyte disorder defined as abnormally high levels of serum potassium [ 1 , 2 , 3 , 4 ]. In 2014, 1.55% (3.7 million) of adults in the general population in the United States (US) were estimated to have hyperkalemia, with a higher prevalence (6.35%) estimated for adults with chronic kidney disease (CKD) and/or heart failure [ 5 ]. The prevalence of hyperkalemia is expected to increase owing to the increase in prevalence of risk factors associated with hyperkalemia (e.g., heart failure, hypertension, CKD) [ 6 ]. Hyperkalemia presents a substantial economic burden, as patients with hyperkalemic events incurred $15,606 higher 1-year total healthcare costs than patients without hyperkalemia [ 7 ].
Although mild hyperkalemia (> 5.0–5.5 mEq/L) is often asymptomatic, severe forms of hyperkalemia (> 6.0 mEq/L) may be life-threatening, resulting in cardiac arrhythmias and sudden death [ 2 , 4 , 8 ]. However, there is large inter-individual variation and symptoms do not always correlate with the absolute potassium level observed [ 9 ]. As a result of these potentially fatal symptoms associated with very high potassium levels, patients are often managed in the emergency department (ED) where they are recommended to receive prompt and aggressive care [ 10 , 11 ]. Following laboratory and electrocardiogram (ECG) assessments to confirm elevated potassium levels, treatment typically begins with agents to stabilize the membrane (e.g., calcium gluconate, calcium chloride) [ 9 ]. If there is no resolution, agents that redistribute potassium into cells (e.g., insulin and glucose or albuterol) are utilized [ 9 ], and sodium bicarbonate may be administered if metabolic acidemia occurs [ 9 ]. In the event that elevated potassium levels persist, excess levels are eliminated through use of potassium-binding agents, dialysis, and loop diuretics [ 8 , 9 , 10 , 12 , 13 ]. Ongoing monitoring of cardiac function using ECGs and laboratory assessments of serum potassium levels are also recommended for patients with moderate to severe hyperkalemia within the ED [ 11 ].
Evidence regarding the management of patients with hyperkalemia in the ED and outcomes following ED visits, such as hyperkalemia recurrence, is limited [ 14 , 15 , 16 , 17 ]. One retrospective study [ 16 ] showed that ED treatment patterns varied widely and that higher potassium levels were associated with increased rates of hospitalization and mortality. Other studies have focused on the management of patients with more severe hyperkalemia (> 6.0 mEq/L), but few studies have characterized mild or moderate hyperkalemia.
Real-world evidence can help clinicians manage patients with hyperkalemia across different severities in the ED. In this study, we characterized the demographics and clinical characteristics of patients with hyperkalemia in the ED setting. We also examined the rates of monitoring and treatments administered in the ED setting as well as the rates of subsequent inpatient admission and hyperkalemia recurrence after discharge from the ED. All analyses were stratified by the severity of hyperkalemia.
Data Source
This study was a retrospective cohort study using electronic medical record (EMR) data from the US Research Action for Health Network (REACHnet) from 2012 to 2018. REACHnet, formed in 2014, is one of nine clinical data research networks participating in PCORnet, the National Patient-Centered Outcomes Research Network, and contains EMR data for over five million patients of all ages, sexes, and racial/ethnic groups from five different health systems.
Compliance with Ethics Guidelines
The New England Independent Review Board provided written approval for this study on June 25, 2018 (NEIRB# 1-5667-1). Written and verbal consent from participants are not applicable to this study.
Sample Selection
The study population included adult patients with at least one ED visit with hyperkalemia (at least one potassium laboratory value > 5.0 mEq/L). Potassium laboratory results were identified on the basis of Logical Observation Identifier Names and Code (LOINC) codes and laboratory names (Supplementary Table 1). The first potassium laboratory value during the ED visit was used to categorize patients by hyperkalemia severity (mild [> 5.0–5.5 mEq/L], moderate [> 5.5–6.0 mEq/L], or severe [> 6.0 mEq/L]). The ED admission date was required to be at least 6 months after the start of the data and the ED discharge date was required to be at least 90 days prior to the end of the data. Patients were also required to have at least one additional encounter after the discharge from the ED.
For patients with multiple eligible ED admissions with hyperkalemia, the index ED visit was randomly selected. The index date was defined as the admission date for the index ED visit with hyperkalemia. The baseline period was defined as the 6-month period prior to the index date. The period spanning from the index date to the date of ED discharge was defined as the ED visit period. The period up to 90 days after ED discharge was defined as the post-discharge period.
Study Variables
During the 6-month baseline period, patient characteristics, comorbidities (identified using the International Classification of Diseases-Ninth/Tenth Revision [ICD-9, ICD-10] codes), previous hyperkalemia treatments (identified using RxNorm codes), and potassium laboratory values were described (Supplementary Table 1). Potassium levels, treatments, and monitoring were described during the ED visit period.
Outcome Measures
Death during the ED visit and the proportion of patients immediately admitted to inpatient care from the ED (i.e., admitted to inpatient care on the same day as their discharge from the ED) were reported. Among patients alive and not immediately admitted to inpatient care, hyperkalemia recurrence (defined as at least one potassium laboratory value > 5.0 mEq/L in any setting) was described within 30, 60, and 90 days of discharge from the ED. All-cause inpatient admissions and inpatient admissions with hyperkalemia (defined as an inpatient admission with at least one potassium laboratory value > 5.0 mEq/L) were also described within 30, 60, and 90 days of ED discharge.
Statistical Analysis
Study variables and outcome measures were described and compared among patients with mild, moderate, and severe hyperkalemia. Counts and percentages were provided for categorical variables and means and standard deviations (SD) were provided for continuous variables. Chi-squared tests for categorical variables and analysis of variance tests for continuous variables were used to compare outcomes in patients with mild hyperkalemia to patients with moderate hyperkalemia and patients with mild hyperkalemia to patients with severe hyperkalemia; p < 0.05 was considered statistically significant. All statistical analyses were conducted using SAS 9.4.
Baseline Patient Characteristics by Hyperkalemia Severity
A total of 6222 patients admitted to the ED with hyperkalemia were eligible for the analysis, among whom 4432 (71.2%) patients had mild hyperkalemia, 1085 (17.4%) patients had moderate hyperkalemia, and 705 (11.3%) patients had severe hyperkalemia (Table 1 ). The mean ages of patients with mild, moderate, and severe hyperkalemia were similar (mild, 61.9; moderate, 62.1; severe, 62.0 years). About half of patients were female (mild, 51.7%; moderate, 51.9%; severe, 47.8%). Overall, the majority of patients were White (49.0%) or African American (49.4%).
Comorbidities were common in patients with an ED visit with hyperkalemia, with an average Charlson comorbidity index (CCI) of 1.9 in mild patients, 2.2 in moderate patients, and 2.4 in severe patients (mild vs. moderate p < 0.001, mild vs. severe p < 0.001). Hypertension was the most common comorbidity, followed by CKD stage 3–5, type 2 diabetes, and heart failure. Rates of CKD stage 3–5, end-stage renal disease, acute kidney injury, and type 2 diabetes increased with severity of hyperkalemia. Heart failure, hypertension, and prior renin–angiotensin–aldosterone system inhibitor use were similar among patients in all hyperkalemia severities (Table 1 ).
Comparison of Clinical Characteristics Across Hyperkalemia Severities During the Emergency Department Visit
Most patients with mild hyperkalemia (85.0%) and over half of patients with moderate hyperkalemia (59.6%) had only one potassium laboratory assessment during their ED visit (Table 2 ). However, most patients with severe hyperkalemia (75.5%) had at least two potassium laboratory assessments. Among patients with multiple potassium laboratory values, potassium levels returned to ≤ 5.0 mEq/L in over half of all patients (mild, 59.7%; moderate, 65.5%; severe, 57.1%).
During the ED visit, patients with more severe hyperkalemia received more hyperkalemia treatments, which included potassium-binding treatments, temporizing agents, diuretics, or dialysis (mild, 13.4%; moderate, 30.8%; severe, 45.7%; all p < 0.001). Temporizing agents were the most common treatment and were more commonly used by patients with severe hyperkalemia (31.6%). Sodium polystyrene sulfonate (SPS) treatment was reserved mostly for patients with severe hyperkalemia (severe 27.4% vs. mild 4.1%, p < 0.001). Diuretics, dialysis, and patiromer were not commonly used during the ED visit (5.7%, 0.8%, 0.0% overall, respectively). Among patients with available ECG data, the proportion of patients receiving ECG monitoring increased with hyperkalemia severity (mild, 56.5%; moderate, 69.6%; severe, 81.0%; mild vs. moderate p < 0.001, mild vs. severe p < 0.001). At ED discharge, only a small proportion of patients received treatment with a potassium-binding treatment (SPS or patiromer) (mild, 0.03%; moderate, 1.9%; severe, 5.2%; mild vs. moderate p < 0.001, mild vs. severe p < 0.001).
Emergency Department and Post-Discharge Outcomes Across Hyperkalemia Severities
A total of 10.6% of patients with severe hyperkalemia died during their ED visit, compared with 3.7% of patients with moderate hyperkalemia and 1.1% with mild hyperkalemia (mild vs. moderate p < 0.001; mild vs. severe p < 0.001). The proportion of patients directly admitted to inpatient care increased as hyperkalemia severity increased (mild, 5.8%; moderate, 8.7%; severe, 12.7%; mild vs. moderate p < 0.001, mild vs. severe p < 0.001) (Table 2 ).
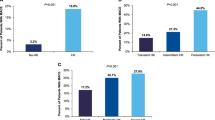
Among patients not directly admitted to inpatient care, the proportion of patients with hyperkalemia recurrence within 30 days post-discharge increased with hyperkalemia severity (mild, 12.9%; moderate, 19.0%; severe, 32.5%; mild vs. moderate hyperkalemia p < 0.001, mild vs. severe hyperkalemia p < 0.001). Similar patterns were observed within 60 and 90 days post-discharge from the ED (Fig. 1 ). Across all severity cohorts, all-cause inpatient admissions were similar 30 days post-discharge (mild, 14.9%; moderate, 15.8%; severe, 14.0%). A similar trend was observed for all-cause inpatient admissions 60 and 90 days post-discharge (Fig. 1 ). The proportion of patients with inpatient admissions with hyperkalemia 30 days post-discharge increased with hyperkalemia severity (mild, 6.5%; moderate, 7.9%; severe, 9.3%; mild vs. moderate hyperkalemia p = 0.16, mild vs. severe p < 0.05) with similar trends observed within 60 and 90 days post-discharge (Fig. 1 ).
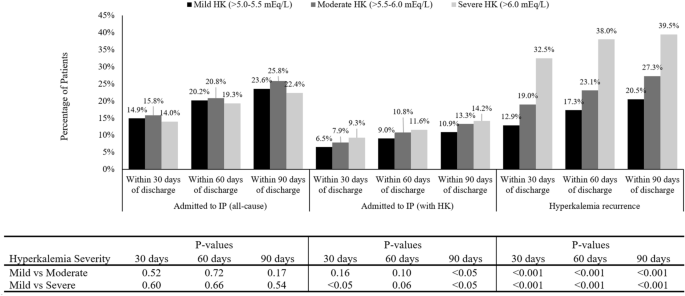
Post-discharge events 30, 60, and 90 days after ED visit by hyperkalemia severity among patients discharged from the ED a . a Calculated among patients alive and not immediately admitted to discharge after the ED visit (mild, n = 4130; moderate, n = 954; severe, n = 550); p values for categorical variables were calculated using chi-squared tests; p values for continuous variables were calculated using ANOVA tests. ED emergency department, HK hyperkalemia, IP inpatient
This study comprehensively characterized the patient demographics and clinical characteristics, hyperkalemia monitoring and management practices, and post-discharge outcomes among patients with hyperkalemia in the ED. This study found that in the ED setting, patients with moderate and severe hyperkalemia had elevated rates of death and immediate inpatient admission, using descriptive analyses. After ED discharge, these patients also had higher rates of inpatient admission and hyperkalemia recurrence. Given the arrival of the novel potassium binders, the management of hyperkalemia has entered a new era and this study provides a contemporary description of the ED management of patients with hyperkalemia by severity.
As a result of the potentially fatal consequences of severe hyperkalemia, patients with hyperkalemia are often managed in the ED [ 11 , 18 ]. The absence of robust and evidence-based treatment guidelines for hyperkalemia management in the ED has posed a challenge for treating hyperkalemia in the ED setting [ 14 , 15 , 16 ]. Prior treatment algorithms that have been published to aid in the clinical management of hyperkalemia in the ED were largely based on anecdotal experience and findings from a small number of patients [ 8 , 14 ]. However, a recent Kidney Disease: Improving Global Outcomes Controversies Conference was held where a multidisciplinary group composed of emergency medicine specialists, nephrologists, renal physiologists, endocrinologists, cardiologists, and dieticians convened to identify best practices in the clinical management of hyperkalemia [ 9 ]. In addition to consensus on an evidence-based treatment algorithm, this conference highlighted the need for frequent evaluations to assess treatment success [ 9 ].
ECG monitoring and repeated assessments of serum potassium levels is a common practice to monitor hyperkalemia, particularly in acute hyperkalemic episodes and among patients with comorbidities [ 4 , 13 , 19 ]. In this study, most patients with severe hyperkalemia were monitored via ECG and had repeated laboratory assessments of serum potassium levels, which aligns with previous studies [ 16 , 18 , 20 ]. Temporizing agents (e.g., albuterol, calcium, etc.) were administered to 16–32% of patients with moderate and severe hyperkalemia during the ED visit. Although temporizing agents are helpful in stabilizing cardiac function, they do not eliminate excess potassium from the body [ 3 , 14 , 19 ]. After treatment with a temporizing agent, SPS was the most commonly used treatment. However, SPS provides limited value in the short-term management of hyperkalemia and it is occasionally associated with severe adverse events (e.g., colonic necrosis and intense diarrhea) [ 14 , 15 ]. The study results pointed to a clear unmet need in treatment of patients with hyperkalemia in the ED setting.
The proportion of patients who died during the ED visit increased as the severity of hyperkalemia increased (mild, 1.1%; moderate, 3.7%; severe, 10.6%; all p < 0.001). Many previous studies [ 2 , 16 , 21 ] also reported an increase in mortality with increased hyperkalemia severity. For example, a 2017 retrospective study found that compared to patients with normal potassium levels (3.5–5.0 mEq/L), patients with “severely elevated” potassium levels (> 6.0 mEq/L) had five times higher odds of dying (95% confidence interval 2.9–8.6) [ 16 ]. However, a recent study found that reducing potassium levels to < 5.5 mEq/L in the ED was associated with a 50% mortality reduction after adjusting for age, creatinine, comorbidities, and initial potassium level, which highlighted the importance of appropriate management of hyperkalemia in the ED setting [ 17 ].
At the end of the ED visit, 34–43% of the patients still had elevated potassium levels (i.e., > 5.0 mEq/L). However, at discharge, only a small proportion of patients (less than 6% in the severe group) received treatment with a potassium-binding treatment (SPS or patiromer). The gap between the elevated potassium level at the end of the ED visit and the low prescription rate of hyperkalemia treatment at discharge may indicate an unmet need for post-ED management of hyperkalemia. The post-discharge burden of hyperkalemia recurrence and hyperkalemia-related inpatient admission further demonstrate such an unmet need.
Using a large EMR database, this study characterized ED management and post-discharge outcomes across hyperkalemia severities; future studies that examine predictors of post-ED outcomes including hyperkalemia recurrence and inpatient admission would be valuable. Furthermore, as the awareness of the unmet need of patients with hyperkalemia increases, in both the ED and post-discharge settings [ 22 ], there is an impetus to understand how clinicians can more effectively treat patients within the ED and after discharge from the ED to ultimately lower rates of hyperkalemia recurrence and readmission. With the development of novel potassium binders [ 23 ], future studies are needed to identify which patient groups (e.g., those with moderate to severe hyperkalemia or with recurring hyperkalemia) would benefit the most from emerging therapies.
Limitations
The findings in this study offer a valuable benchmark that can help healthcare stakeholders assess progress in the clinical management of hyperkalemia. This study, conducted in a large EMR database, provides a rich data source including laboratory data and longitudinal information on patients with care across multiple settings, which enabled a characterization of events that occurred both during and after an ED visit. One of the limitations of the study is that although we assessed a large number of variables at baseline and during the ED visit, not all clinical characteristics were assessed such as serum bicarbonate level. Despite that recent meta-analysis [ 24 ] has shown that risk of hyperkalemia and mortality among patients with ESRD can be partially dependent on the duration of between-dialysis period, we found the proportion of stage 5 or patients with ESRD increased as hyperkalemia severity increases. However, we did not have the data on duration of between-dialysis period to provide additional insights into this patient population with ESRD.
Although the large number of patients in this study likely comprise a representative sample of patients with hyperkalemia in Louisiana, the generalizability of this study may be limited if the management of hyperkalemia in Louisiana differs from other areas in the US. Additionally, because out-of-network healthcare encounters were not captured in the EMR database, the baseline and post-discharge results in this study may be slightly underestimated.
Conclusions
Patients with moderate and severe hyperkalemia experienced elevated risk of death and direct inpatient admission after an ED visit, as well as hyperkalemia recurrence and hyperkalemia-related inpatient readmissions following discharge from the ED, from a descriptive analysis. Additional studies are warranted to assess strategies to reduce recurrence and inpatient admission in this patient population.
Lehnhardt A, Kemper MJ. Pathogenesis, diagnosis and management of hyperkalemia. Pediatr Nephrol. 2011;26(3):377–84.
Article Google Scholar
Luo J, Brunelli SM, Jensen DE, Yang A. Association between serum potassium and outcomes in patients with reduced kidney function. Clin J Am Soc Nephrol. 2016;11(1):90–100.
Article CAS Google Scholar
Mushiyakh Y, Dangaria H, Qavi S, et al. Treatment and pathogenesis of acute hyperkalemia. J Community Hosp Intern Med Perspect. 2012. https://doi.org/10.3402/jchimp.v1i4.7372 .
Article PubMed PubMed Central Google Scholar
Hollander-Rodrigues JC, Calvert JF. Hyperkalemia. Am Fam Physician. 2006;73(2):283–90.
Google Scholar
Betts KA, Woolley JM, Mu F, et al. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34(6):971–8.
Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018. https://doi.org/10.1161/JAHA.118.008888 .
Betts KA, Woolley JM, Mu F, et al. The cost of hyperkalemia in the United States. Kidney Int Rep. 2018;3(2):385–93.
Rossignol P, Legrand M, Kosiborod M, et al. Emergency management of severe hyperkalemia: guideline for best practice and opportunities for the future. Pharmacol Res. 2016;113:585–91.
Lindner G, Burdmann EA, Clase CM, et al. Acute hyperkalemia in the emergency department: a summary from a Kidney Disease: Improving Global Outcomes conference. Eur J Emerg Med. 2020;27(5):329–37.
Ahee P, Crowe AV. The management of hyperkalaemia in the emergency department. J Accid Emerg Med. 2000;17(3):188–91.
Kovesdy CP. Management of hyperkalemia: an update for the internist. Am J Med. 2015;128(12):1281–7.
Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158(8):917–24.
Lane D. 2008. Hyperkalemia, Society for Academic Emergency Medicine Philadelphia, Pennsylvania: Temple University School of Medicine. https://www.saem.org/cdem/education/online-education/m4-curriculum/group-m4-endocrine-electrolytes/hyperkalemia . Accessed 6 June 2019.
Rafique Z, Chouihed T, Mebazaa A, Frank PW. Current treatment and unmet needs of hyperkalaemia in the emergency department. Eur Heart J Suppl. 2019;21(Suppl A):A12–9.
Peacock WF, Rafique Z, Clark CL, et al. Real world evidence for treatment of hyperkalemia in the emergency department (REVEAL-ED): a multicenter, prospective, observational study. J Emerg Med. 2018;55(6):741–50.
Singer AJ, Thode HC Jr, Peacock WF. A retrospective study of emergency department potassium disturbances: severity, treatment, and outcomes. Clin Exp Emerg Med. 2017;4(2):73–9.
Singer AJ, Thode HC, Peacock WF. Rapid correction of hyperkalemia is associated with reduced mortality in ED patients. Am J Emerg Med. 2019;38(11):2361–64.
Freeman K, Feldman JA, Mitchell P, et al. Effects of presentation and electrocardiogram on time to treatment of hyperkalemia. Acad Emerg Med. 2008;15(3):239–49.
National Kidney Foundation. 2016. Best practices in managing hyperkalemia in chronic kidney disease. https://www.kidney.org/sites/default/files/02-10-7259%20Hyperkalemia%20Tool.pdf . Accessed 23 Aug 2019.
Pfortmüller CA, Leichtle AB, Fiedler GM, Exadaktylos AK, Lindner G. Hyperkalemia in the emergency department: etiology, symptoms and outcome of a life threatening electrolyte disorder. Eur J Intern Med. 2013;24(5):e59–60.
Goyal A, Spertus JA, Gosch K, et al. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307(2):157–64.
Aggarwal S, Topaloglu H, Kumar S. Trends in emergency room visits due to hyperkalemia in the United States. Value Health. 2015;18:A386.
Rossignol P. A new area for the management of hyperkalaemia with potassium binders: clinical use in nephrology. Eur Heart J Suppl. 2019;21(Suppl A):A48–54.
Bem D, Sugrue D, Wilding B, et al. The effect of hyperkalemia and long inter-dialytic interval on morbidity and mortality in patients receiving hemodialysis: a systematic review. Ren Fail. 2021;43(1):241–54.
Download references
Acknowledgements
Sponsorship for this study and the journal’s Rapid Service Fees were funded by AstraZeneca.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Dr. Gloria DeWalt of Analysis Group, Inc. Support for this assistance was funded by AstraZeneca.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Jill Davis, Rubeen Israni, Keith A. Betts, Fan Mu, Erin E. Cook, Deborah Anzalone, Harold Szerlip, Lei Yin, Gabriel I. Uwaifo, and Eric Q. Wu contributed to the study’s design, data acquisition, analysis, and interpretation. Keith A. Betts, Fan Mu, Erin E. Cook, and Eric Q. Wu had a significant role in conducting formal analyses. All authors contributed to writing and editing of the manuscript.
Disclosures
Jill Davis, Rubeen Israni, and Deborah Anzalone were employees of AstraZeneca at the time the study was conducted. Jill Davis is currently affiliated with ENDO Pharmaceuticals, Rubeen Israni is currently affiliated with GlaxoSmithKline, and Deborah Anzalone has since retired and so has no current affiliation. Keith A. Betts, Fan Mu, Erin E. Cook, Lei Yin, and Eric Q. Wu are employees of Analysis Group, Inc., which received payment from AstraZeneca for the conduct of this analysis. Harold Szerlip is on the advisory board and speaker’s bureau for AstraZeneca. Gabriel I. Uwaifo has nothing to disclose.
Data Availability
The datasets analyzed in this study are not publicly available. The research reported in this article was conducted in partnership with Research Action for Health Network (REACHnet), funded by the Patient Centered Outcomes Research Institute ® (PCORI Award RI-CRN-2020–008). REACHnet is a partner network in PCORnet ® , the National Patient-Centered Clinical Research Network, which was developed with funding from PCORI ® . The content of this article is solely the responsibility of the author(s) and does not necessarily represent the views of other organizations participating in, collaborating with, or funding REACHnet or PCORnet ® , or of PCORI ® . The authors acknowledge the participation of REACHnet partner health systems: Tulane Medical Center and Ochsner Medical Center in this project.
Author information
Authors and affiliations.
Formerly AstraZeneca, Wilmington, DE, USA
Jill Davis, Rubeen Israni & Deborah Anzalone
Analysis Group, Inc., 111 Huntington Avenue, 14th Floor, Boston, MA, 02199, USA
Keith A. Betts, Fan Mu, Erin E. Cook, Lei Yin & Eric Q. Wu
Baylor University Medical Center, Dallas, TX, USA
Harold Szerlip
Ochsner Medical Center, New Orleans, LA, USA
Gabriel I. Uwaifo
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Fan Mu .
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 160 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/ .
Reprints and permissions
About this article
Davis, J., Israni, R., Betts, K.A. et al. Real-World Management of Hyperkalemia in the Emergency Department: An Electronic Medical Record Analysis. Adv Ther 39 , 1033–1044 (2022). https://doi.org/10.1007/s12325-021-02017-w
Download citation
Received : 29 October 2021
Accepted : 06 December 2021
Published : 27 December 2021
Issue Date : February 2022
DOI : https://doi.org/10.1007/s12325-021-02017-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Electronic medical records
- Emergency department
- Hyperkalemia
- Post-discharge
- Real-world outcomes
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 08 November 2022
Acute severe asthma in emergency department: clinical characteristics, risk factors, and predictors for poor outcome
- Ashraf Zin E L-Abdeen Mohamed 1 ,
- Lamiaa Hassan Shaaban 1 ,
- Shereen Frghaly Gad 1 ,
- Esraa Abdel Azeem 2 &
- Waleed Gamal Elddin ORCID: orcid.org/0000-0002-3367-5499 1
The Egyptian Journal of Bronchology volume 16 , Article number: 57 ( 2022 ) Cite this article
3076 Accesses
Metrics details
Severe asthma exacerbation can be a frightening experience to the patient and physician. Despite continuous efforts to frame management guidelines and advances in treatment, severe exacerbations still occur. In order to prevent and judicious management of asthma exacerbations, we should predict them first. This study aims to evaluate distinct clinical trajectories and management outcome of patients with severe asthma exacerbations and also evaluate predictors for poor outcome.
Patients suffering from acute asthma exacerbation and presented to emergency room (forty patients) were grouped into 2 groups (groups A and B) according to severity of exacerbation. Assessment included full clinical history, laboratory investigations (including eosinophil cell count and serum IgE level), Beck’s anxiety and depression inventory scales, assessment of asthma medication adherence and control level, and peak expiratory flow measurement (at presentation, 1 and 6 h after).
Fifty-five percent of patients suffered from severe and life-threatening asthma exacerbations, 63.6% of them were females. The most important predictors for severe exacerbations were SO2 < 90% at baseline (OR = 4.56; 95% CI = 3.45–7.56; P < 0.001), PEFR after 1 h (OR= 3.34; 95%CI = 1.90–4.90; P < 0.001), and uncontrolled asthma (OR= 3.33; 95%CI = 2.50–5.05; P < 0.001). Predictors for hospitalization were old age (OR = 1.11; 95%CI = 1.09–2.11; P < 0.001), uncontrolled asthma (OR = 2.34; 95%CI = 2.01–4.40; P < 0.001), PEFR after 1 h (OR= 4.44; 95%CI= 3.24–7.68; P < 0.001), and SO2 <90% at baseline (OR= 5.67; 95%CI= 3.98–8.50; P < 0.001).
Conclusions
Severe asthma exacerbations can be predicted by old age, previous history of mechanical ventilation, obstructive sleep apnea, overuse of SABA, uncontrolled asthma, moderate to severe depression, eosinophilia, SO 2 <90%, and low peak expiratory flow rates.
Asthma is a common and potentially serious chronic disease that imposes a substantial burden on patients, their families, and the community. It causes respiratory symptoms, limitation of activity, and flare-ups (attacks) that sometimes require urgent health care and may be fatal [ 1 ].
Severe exacerbation can occur in patients with mild or well-controlled asthma. Exacerbations may occur in patients with a pre-existing diagnosis of asthma or, occasionally, as the first presentation of asthma in response to exposure to an external agent risk factor (e.g., viral upper respiratory tract infection, pollen, or pollution) and/or poor adherence with controller medication; however, a subset of patients presents more acutely and without exposure to known risk factors [ 2 ].
Acute severe asthma is considered a major economic & health burden. It represents about 3% of hospital admissions [ 3 ]. Some other entities similar not identical to that of acute severe asthma also require precise definitions: so Kenyon et al. [ 4 ] proposed the term critical asthma syndromes (CAS) to identify any child or adult who is at risk of fatal asthma.
Around 300 million people have asthma worldwide (likely by 2025, a further 100 million may be affected) and account for 1 in every 250 deaths [ 5 ]. Acute severe asthma attack is increasingly associated with different specific phenotypes and it represents a major unmet therapeutic need [ 6 ].
Asthma critically depends on a series of cell adhesion molecule-mediated interactions between vascular endothelium and leukocytes especially associated with T-helper cell type 2 (Th2) immune responses, which are typical of other atopic conditions. Elevated levels of Th2 cells in the airways release specific cytokines, including interleukin IL-4, IL-5, IL-9, and IL-13 that activate B lymphocytes to produce allergen-specific IgE which binds to the high affinity mast cell receptors, leading to their activation and the release of inflammatory mediators as histamine [ 7 , 8 ].
This study aims to evaluate the management outcome of patients with severe asthma exacerbations and also evaluate predictors for both hospitalization and poor outcome.
Patients and methods
Study participants and ethical approval.
This prospective observational study was performed on 40 asthmatic patients in the age group of 18–70 years suffering from asthma exacerbation who were identified using the diagnostic criteria defined by Global Initiative for Asthma [ 9 ] belonging to either gender and referred to emergency department of Assiut university hospital during the period from October 2019 to October 2020. Severe asthma exacerbation was considered for a patient who talks in words, is agitated, uses accessory respiratory muscles, and has a respiratory rate > 30/min, heart rate > 120/min, O2 saturation on air < 90%, and PEF ≤ 50% of their best or predicted value [ 9 ].
Patients were categorized according to exacerbation severity into group A including mild and moderate asthma exacerbation and group B including severe and life-threatening asthma exacerbation. All participants or their legal guardians gave informed written consent. Exclusion criteria were pregnancy, presence of other chronic pulmonary diseases, evidence of heart failure, pneumonia, and inability to obtain written informed consent. Study protocol was approved by the ethical committee of Faculty of Medicine, Assiut University, and it was carried out in accordance with the Declaration of Helsinki (IRB: 17100097).
Demographic, clinical, and laboratory data
Included patients underwent careful history taking and full clinical examination. Chest radiography to exclude comorbid conditions, complications, and mimics of asthma (pneumonia, pneumothorax, and heart failure). Medical care for asthma, number of prior hospitalizations for asthma, past mechanical ventilation for asthma, any psychic disturbance, hospitalization for asthma in the past 12 months, and past ED visits for asthma in the past 12 months were assessed.
Comorbidities as diabetes, hypertension, gastro-esophageal reflux disease (GERD), allergic rhino-sinusitis (AR), obstructive sleep apnea (OSA), and confirmed food allergy were assessed. Assessment of asthma medication adherence was done using Morisky Medication Adherence Scales (MMAS-4) in which a questionnaire from relatives of the patient was taken [ 10 ], as well as assessment of asthma control level [ 11 ]. Arterial blood gases (ABG): ABG was obtained on room air using heparinized blood sample from radial artery and analyzed using blood gases analyzer (Rapid lab 850; CHIRON /Diagnostics, Critical care systems). Complete blood count (CBC): Using CELL-DYN Ruby, 2ml of venous blood was placed in standard tubes containing K3 EDTA anticoagulant. Total RBCs, HB, total WBCs, eosinophils, platelet count, and random distribution width (RDW) were assessed. Serum non-specific IgE level was measured for all participants.
Assessment of anxiety and depression
Beck’s anxiety inventory (bai).
This 21-item self-report questionnaire was originally developed to assess clinical anxiety differentiated from normal anxiety. The Beck Anxiety Inventory Scores Interpretation: A grand sum between 0 and 21 indicates low anxiety, grand sum between 22 and 35 indicates moderate anxiety, and grand sum that exceeds 36 is high [ 12 ].
Beck Depression Inventory 2 (BDI-II)
A 4-point scale indicates degree of severity; items are rated from 0 (not at all) to 3 (extreme form of each symptom). The Beck Depression Inventory Scores Interpretation: minimal range (0–13), mild depression (14–19), moderate depression (20–28), and severe depression (29–63) [ 13 ].
Peak expiratory flow measurement
Serial measurement of lung function by using Microlife Digital Peak Flow Meter (PEF) performed at presentation and again 1 to 6 h after initial treatment for categorizing the severity of the exacerbation and predicting the need for hospitalization.
Statistical analysis
Data was collected and analyzed using SPSS (statistical package for social sciences) program (version 20, IMB and Armonk, New York). Continuous data was expressed in the form of mean (± SD) and compared by t -test while nominal data was expressed in the form of frequency (percentage) and compared by chi-square test. Predictors of asthma exacerbation and hospitalization among enrolled patients were determined by regression analysis. Accuracy of PEF in prediction of acute severe asthma was assessed by receiver operator characteristics curve (ROC curve). Odds ratios were provided with 95% confidence intervals (CI), and hence, P -value was considered significant if <0.05.
Forty-five percent of patients (group A) presented with mild and moderate exacerbations while 55% (group B) had severe and life-threatening exacerbation. Demographic data and patient characteristics are shown in Table 1 .
Patients of group B had significantly higher age and body mass index (BMI) in comparison to those of group A [50.32 ± 10.92 Vs. 36.78 ± 8.86; P < 0.001 and 28.64 ± 3.86 Vs. 26.33 ± 2.76 (kg/m2); P = 0.04].
Patients with severe and life-threatening exacerbation (group B) had higher frequency of previous emergency room visits (100% vs. 66.7%; P < 0.001), hospitalization (86.4% vs. 33.3%; P < 0.001), and mechanical ventilation (50% vs. 11.1%; P = 0.01).
Moderate and high anxiety levels were prevalent in patients of group B. Mild, moderate, and severe depression was significantly higher in group B patients 40.9%, 50%, and 9.1%, respectively (Table 2 ).
Regarding laboratory data, severe group showed significantly lower SO 2 ( P < 0.001), higher eosinophil count ( P < 0.001), and higher serum IgE level ( P < 0.001) (Table 3 ). 61.1% patients of non-severe group vs. 18.2% of severe group were discharged. Frequency of hospitalization was 33.3% in the case of non-severe group vs. 72.7% in the case of severe group (Table 4 ).
Regarding the assessment of PEFR accuracy in the prediction of exacerbation severity among enrolled patients, PEFR after 1 h at cut-off point < 110 had 100% sensitivity and 62% specificity for the prediction of severe acute asthma with an overall accuracy of 82.9% and area under the curve was 0.81 (Tables 5 and 6 ); the predictors for severe exacerbation were old age, previous history of mechanical ventilation, obstructive sleep apnea, overuse of SABA, uncontrolled asthma, moderate to severe depression, eosinophilia, SO <90%, and low peak expiratory flow rates (Table 7 ).
The most important predictors were SO2 <90% at baseline (OR= 4.56; 95%CI= 3.45–7.56; P < 0.001), PEFR after 1 h (OR= 3.34; 95%CI= 1.90–4.90; P < 0.001), and uncontrolled asthma (OR= 3.33; 95%CI= 2.50–5.05; P < 0.001).
Based on the current study, the predictors of hospitalization were old age (OR= 1.11; 95%CI= 1.09–2.11; P < 0.001), uncontrolled asthma (OR= 2.34; 95%CI= 2.01–4.40; P < 0.001), PEFR after 1 h (OR= 4.44; 95%CI= 3.24–7.68; P < 0.001), and SO2 <90% at baseline (OR= 5.67; 95%CI= 3.98–8.50; P < 0.001) (Table 8 ).
In this study, the mean age of patients of the severe group was 50.32 ± 10.92 significantly higher compared to 36.78 ± 8.86 for the non-severe group. Patient’s age >40 years was detected to be a significant predictor for exacerbation severity. That risk is mostly attributed to more comorbidities together with gradual decrease of lung function which will adversely affect asthma prognosis.
Most of the patients enrolled were females and most of group B were females. BMI was significantly higher in group B with mean values of 28.64 ± 3.86 vs. 26.33 ± 2.76 for group A. Percentage of current, passive, and ex-smokers were higher in group B.
Loymans et al. in their quest to develop a multivariate prediction model revealed that patients with exacerbations showed higher mean age (42.1 Vs 39) and higher percentage of females (77.5 vs 67) versus patients without exacerbations during a 12-month follow-up period [ 14 ].
On the contrary, Kang et al. [ 15 ] stated that frequent hospitalization history and poor drug adherence are the main factors responsible for severe exacerbations while patients with mild asthma require greater attention to their age and comorbidities.
Medical history showed that previous ED visit, hospitalization, and previous mechanical ventilation were significantly higher among patients of group B. Yii et al. [ 16 ] followed 177 patients with problematic asthma for 5 years; risk factors included two or more exacerbations in the last year, elevated body mass index, obstructive sleep apnea, depression, and GERD. 9.5% had frequent severe exacerbations [ 16 ].
Regarding previous hospital admission, our study confirmed it as a risk factor for future severe asthma exacerbation which is proved also by Alvarez et al. (2005) showing that a history of previous hospitalizations due to asthma exacerbations is independent predictor of near-fatal and fatal asthma [ 17 ]. Also Gonzalez-Barcala et al. [ 18 ] showed that the combination of previous hospital admissions and new episodes of hospitalization is consistently observed.
According to Silverman et al. [ 19 ], approximately 36% of emergency department patients with asthma aggravation were current smokers. Exposure to environmental tobacco smoke (ETS) has been cited as a risk factor for asthma exacerbations and emergency room visits and has been associated with worse asthma severity according to Merianos et al. [ 20 ].
Retrospective observational study by To et al. [ 21 ] showed that obesity was demonstrated to be independently and closely associated with severe acute exacerbations of asthma.
Obesity and asthma overlap with each other continuously and many phenotypes were described. Holguin et al. [ 22 ] stated that earlier onset asthma associated with obesity mostly suffer severe course (tended to have higher markers of Th2 inflammation). There is also a group with later-onset disease, mostly females, with a little airway inflammation, but significant inflammation in adipose tissue and increased airway oxidative stress [ 23 ]. The most notable changes caused by obesity in lung physiology are shown in a reduction of FRC and ERV.
In contrast to previous reports, a study by Kimura et al. [ 24 ] showed that the presence of several asthma comorbidities, such as obesity and GERD, was not associated with exacerbation status. These discrepancies may be explained by the ethnic differences between the study’s samples (i.e., lower prevalence of obesity and/or GERD).
OSA was one of the predictors of acute severe asthma exacerbation according to our study with an odds ratio of 1.11 and a 95% confidence interval of 1.01–2.35. Also Belachew et al. [ 25 ] concluded that obstructive sleep apnea was considerably linked with repeated exacerbations of asthma and the most prevalent among significantly associated predictors.
SABA overuse is considered a significant risk factor for severe asthma exacerbation that could be explained by the fact that the types of asthma that are uncontrolled or severe require more SABA use to relieve the frequent spasms and predicts that future exacerbations will be of more severity. UK registry data suggested SABA overuse or overreliance may be linked to asthma-related deaths [ 26 ].
Data from 1778 asthma patients attending primary care and specialist clinic were analyzed revealing that 66.2 % were poorly controlled, SABA overuse found in 26.2% who were prescribed ≥10 canisters per year. Findings from this African cohort of the SABINA III study indicate that SABA over-prescription and SABA over-the-counter purchase are common and associated with poor asthma-related outcomes. This highlights the need for healthcare providers/policymakers to align clinical practices with the latest treatment recommendations [ 27 ].
In terms of asthma control level, our study validated that patients of severe exacerbation group were significantly uncontrolled which made them more prone to asthma exacerbation severity and thus hospitalization. Also, Neffen et al. [ 28 ] found that 31% of patients had severe asthma, and of these, 64.1% were uncontrolled. Asthma control level remains unsatisfactory among most asthma patients; variables associated with poor control included non-adherent to medication (OR = 0.16, 95%CI (0.059, 0.48)), low level of patient enablement (OR = 0.19, (95%CI (0.08, 0.49)), and poor relationship with healthcare provider (OR = 0.024, 95%CI (0.02, 0.23)). Belachew et al. [ 29 ] highlighted multifaceted interventions, including comprehensive asthma education along with an integrated treatment plan to improve asthma control and quality of life.
High asthma adherence was found to significantly affects the exacerbation severity in this study which is explained by the fact that there may be deficient asthma management for group B patients and that illiterate patients are more in group B who are non-comprehensive of the proper use of ICS inhaler techniques mostly and are not aware of the importance of disease follow-up visits to the doctors. A cohort study by Sideleva et al. [ 23 ] concluded that most of the subjects with severe exacerbation adhered well to medicines; one of the explanations for the discrepancy is that patients with poor medication adherence were carefully excluded.
Regarding psychological impact on asthma exacerbation severity, we concluded that clinically concerning levels of anxiety and depression significantly and inversely affect patients of group B in this study and considered as a predictor for severe asthma attacks. Our study showed that female patients suffered clinically concerning scores of anxiety and depression more than males.
Most studies regarding asthma and anxiety and depression are cross-sectional; however, longitudinal studies have confirmed that the correlation between psychological abnormalities and asthma is stable over time. This could be explained by the following hypotheses: asthma itself increases the risk of developing anxiety and depression, mood and anxiety disorders lead to a higher risk of developing asthma, and asthma, anxiety, and depression are linked by a common underlying pathway [ 30 ].
Also, a cross-sectional study by Ritz et al. [ 31 ] confirmed that psychological triggers were consistently associated with exacerbations and emergency treatments over and above other triggers and affective disorders.
We investigated potential biomarkers related to Th2-driven inflammatory pathways, such as blood eosinophil count as it is a long-standing characteristic of asthma. In our study, higher eosinophilia (a blood eosinophil count > 300 cells/μL) was among group B versus group A [13 (59%) vs 1 (5.6%); p <0.001]. Zeiger et al. [ 32 ] likewise concluded that a blood eosinophil count > 400 cells/μL was an independent risk factor for asthma exacerbations and asthma-related emergency department visits or hospitalizations. Also, Jackson et al. [ 33 ] concluded the same results regarding eosinophil count, while serum IgE concentrations had no influence on asthma attack frequency.
The normal range of blood eosinophil count is 30–350 cells/μL; however, there is controversy with respect to the cut-off level associated with increased risk of asthma complications. In clinical trials involving mepolizumab, Austin et al. [ 34 ] found that the rate of clinically significant asthma exacerbations varied according to blood eosinophil level and employed blood eosinophil cut-offs of ≥ 150 to ≥ 300 cells/μL.
Severe asthma that is not controlled despite optimal treatment represents about 10% of asthma population. Presence of eosinophilic inflammation pathway in the respiratory tract and blood is involved and interleukin-5 (IL-5) has recently been identified as a major promotor of this pathway. The anti-IL-5 antibodies reduce the incidence of exacerbation and allowed steroid sparing in severe asthma patients. Anti-IL-5 antibodies are now a standard treatment for severe eosinophilic asthma that can also be useful in an emergency to treat steroid-refractory eosinophilic acute severe asthma [ 35 ].
IgE biomarker was a significant risk factor for acute severe asthma but not a predictor for asthma exacerbation severity according to this study. A recent study by Haselkorn et al. [ 36 ] on the long-term predictors of poorly controlled asthmatics demonstrated that higher total IgE levels were noted in poorly-controlled persistent asthmatics than in other asthmatics.
In this study, SO 2 < 90% is considered a predictor for asthma exacerbation severity and hospitalization significantly with odds ratio value equals 4.56 and 5.67 respectively which is in concordance with previous studies.
In patients with asthma, the PEFR percent predicted correlates reasonably well with the percent predicted value for the forced expiratory volume in one second (FEV1) and provides an objective measure of airflow limitation when spirometry is not available. In this current study, each patient was asked to perform PEFR on three occasions but the results showed that PEFR after 1-h treatment was a predictor for acute severe exacerbation with OR =3.34 and 95% confidence interval (1.90–4.9). PEFR values after 1 h and 6 h of treatment were reliable predictors for exacerbation severity but PEFR value on admission was not (Figs. 1 and 2 ).
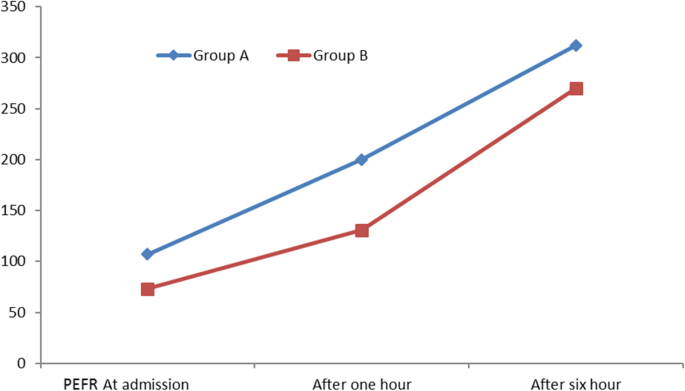
Line graph showing mean PEF rates on admission, 1 h after treatment and after 6 h of treatment among patients of both groups. PEFR, peak expiratory flow rate
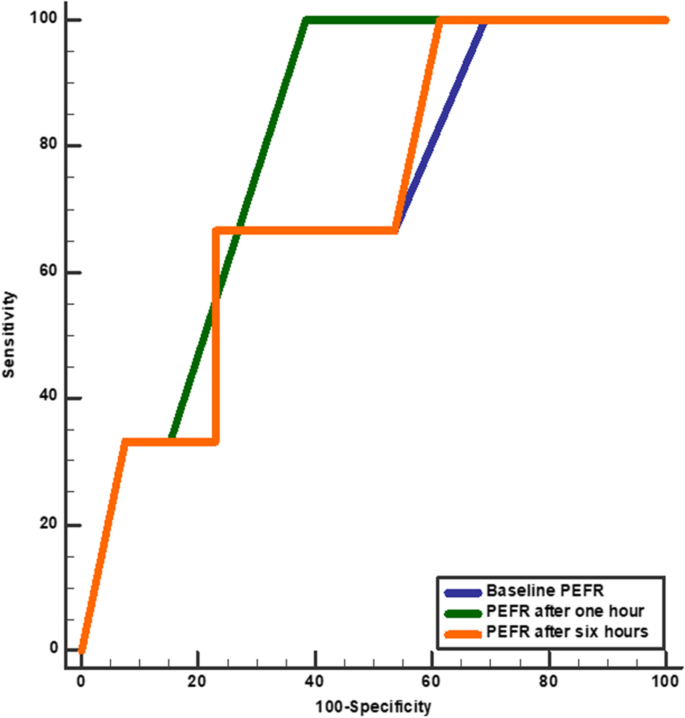
ROC curve shows accuracy of PEFR in prediction of severe acute exacerbation in asthmatic patients. PEFR, peak expiratory flow rate. Baseline PEFR (blue line) cut-off point< 80 (sensitivity 45%, specificity 89%, accuracy 64.8%, and AUC 0.70), PEFR after 1 h (green line) cut-off point < 260 (sensitivity 100%, specificity 62%, accuracy 82.9%, and AUC 0.81), and PEFR after 6 h (orange line) cut-off point < 110 (sensitivity 65%, specificity 88.2%, accuracy 75.5%, and AUC 0.72).
Kole and colleagues stated that persistent airflow limitation (PAL) defined as a post-bronchodilator FEV1/forced vital capacity (FVC) < lower limit of normal represented 33% of severe asthma recruited patients and also in 16% of patients with milder disease. In patients with mild asthma, more caution and intense treatment should be considered as this group was associated with a higher level of eosinophilic inflammation and a higher risk of exacerbations [ 37 ].
Bloom et al.’s study [ 38 ] showed that during 7 years of follow-up, exacerbations occur in around one-third of patients. Of those who exacerbate, half did not frequently exacerbate, so the timing of future exacerbations is largely unpredictable. Just 2% exhibit a frequent-exacerbating phenotype. Past exacerbation patterns are the most informative risk factor for predicting future exacerbations [ 38 ].
Severe asthma exacerbations can be anticipated by determined risk factors as age >40 years, uncontrolled disease symptoms, oral steroids use, and overuse of SABA. Comorbidities as DM, GERD, OSA, food allergy, and moderate and severe depression make patients at risk for acute severe asthma exacerbation. Patients with high blood eosinophils and high Ig E levels are at risk for acute severe asthma. The most accurate independent predictor for severe asthma exacerbation is the PEFR value after 1 h of treatment.
Limitations of the study
Our study recruited a limited sample of selected patients in a single-center study; also, specific clinical characteristics of the study population (acute severe asthma) may limit the generalization of the results.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Arterial blood gases
Allergic rhino-sinusitis
Beck’s Anxiety Inventory
Beck Depression Inventory 2
Critical asthma syndromes
Environmental tobacco smoke
Expiratory reserve volume
Forced expiratory volume in 1st second
Forced vital capacity
Functional residual capacity
Gastro-esophageal reflux disease
Inhaled corticosteroids
Immunoglobulin E
Morisky Medication Adherence Scales
Persistent airflow limitation
Peak expiratory flow
Peak expiratory flow rate
Short acting ßeta agonist
T-helper cell type 2
Global Initiative for Asthma (GINA) Global Strategy for Asthma Management and Prevention (2021 Update) [(accessed on 10 August 2021)]; Available online: https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf
Ramnath VR, Clark S, Camargo CA (2007) Multicenter study of clinical features of sudden-onset versus slower-onset asthma exacerbations requiring hospitalization. Respiratory care. 52(8):1013–1020
PubMed Google Scholar
Serrano-Pariente J, Rodrigo G, Fiz JA, Crespo A, Plaza V, High Risk Asthma Research Group (2015) Identification and characterization of near-fatal asthma phenotypes by cluster analysis. Allergy. 70(9):1139–1147
Article Google Scholar
Kenyon N, Zeki AA, Albertson TE, Louie S (2015) Definition of critical asthma syndromes. Clinical reviews in allergy & immunology. 48(1):1–6
Kostakou E, Kaniaris E, Filiou E, Vasileiadis I, Katsaounou P, Tzortzaki E et al (2019) Acute severe asthma in adolescent and adult patients: current perspectives on assessment and management. Journal of clinical medicine. 8(9):1283
Article CAS PubMed Central Google Scholar
Gaga M, Zervas E, Samitas K, Bel EH (2012) Severe asthma in adults: an orphan disease? Clinics in chest medicine. 33(3):571–583
Article PubMed Google Scholar
Aron J, Akbari O (2017) Regulatory T cells and type 2 innate lymphoid cell-dependent asthma. Allergy. 72(8):1148–1155
Article CAS PubMed Google Scholar
Papi A, Brightling C, Pedersen S, Reddel H (2017) Asthma. Lancet 391(2):783–800
Global Initiative for Asthma (GINA) Global Strategy for Asthma Management and Prevention (2019 Update) [(accessed on 6 August 2019)]; Available online: https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf
Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. The journal of clinical hypertension. 10(5):348–354
Article PubMed PubMed Central Google Scholar
Thomas M, Kay S, Pike J, Williams A, Rosenzweig J, Hillyer E et al (2009) The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Primary Care Respiratory Journal 18(1):41–49
Steer RA, Beck AT (1997) Beck Anxiety Inventory. In: Zalaquett CP, Wood RJ (eds) Evaluating stress: a book of resources. Scarecrow Education, pp 23–40
Google Scholar
Beck AT, Steer RA, Brown GK (1996) Manual for the beck depression inventory-II. San Antonio, TX: Psychological Corporation. 1(82):10–37
Loymans RJ, Honkoop PJ, Termeer EH, Snoeck-Stroband JB, Assendelft WJ, Schermer TR et al (2016) Identifying patients at risk for severe exacerbations of asthma: development and external validation of a multivariable prediction model. Thorax. 71(9):838–846
Kang HR, Song HJ, Nam JH, Hong SH, Yang SY, Ju S et al (2018) Risk factors of asthma exacerbation based on asthma severity: a nationwide population-based observational study in South Korea. BMJ open. 8(3):e020825
Yii ACA, Tan JHY, Lapperre TS, Chan AKW, Low SY, Ong TH et al (2017) Long term future risk of severe exacerbations: distinct 5 year trajectories of problematic asthma. Allergy 72:1398–1405
Alvarez GG, Schulzer M, Jung D, Fitzgerald JM (2005) A systematic review of risk factors associated with near-fatal and fatal asthma. Canadian respiratory journal. 12(5):265–270
Gonzalez-Barcala FJ, San-Jose ME, Nieto-Fontarigo JJ, Carreira JM, Calvo-Alvarez U, Cruz MJ, et al (2018) Association between blood eosinophil count with asthma hospital readmissions. Eur J Intern Med 53:34–9
Silverman RA, Hasegawa K, Egan DJ, Stiffler KA, Sullivan AF, Camargo CA Jr (2017) Multicenter study of cigarette smoking among adults with asthma exacerbations in the emergency department, 2011–2012. Respiratory medicine. 125(7):89–91
Merianos AL, Dixon CA, Mahabee-Gittens EM (2017) Secondhand smoke exposure, illness severity, and resource utilization in pediatric emergency department patients with respiratory illnesses. Journal of Asthma. 54(8):798–806
To M, Hitani A, Kono Y, Honda N, Kano I, Haruki K, To Y (2018) Obesity-associated severe asthma in an adult Japanese population. Respiratory investigation. 56(6):440–447
Holguin F, Bleecker ER, Busse WW, Calhoun WJ, Castro M, Erzurum SC et al (2011) Obesity and asthma: an association modified by age of asthma onset. Journal of Allergy and Clinical Immunology. 127(6):1486–1493
Sideleva O, Suratt BT, Black KE, Tharp WG, Pratley RE, Forgione P et al (2012) Obesity and asthma: an inflammatory disease of adipose tissue not the airway. American journal of respiratory and critical care medicine. 186(7):598–605
Article CAS PubMed PubMed Central Google Scholar
Kimura H, Konno S, Makita H, Taniguchi N, Shimizu K, Suzuki M et al (2018) Prospective predictors of exacerbation status in severe asthma over a 3-year follow-up. Clinical & Experimental Allergy. 48(9):1137–1146
Article CAS Google Scholar
Belachew SA, Erku DA, Yimenu DK, Gebresillassie BM (2018) Assessment of predictors for acute asthma attack in asthmatic patients visiting an Ethiopian hospital: are the potential factors still a threat? Asthma research and practice. 4(1):1–7
Levy M, Andrews R, Buckingham R, Evans H, Francis C, Houston R, Lowe D, Nasser S, Pation J, Puri N, Stewart K (2014) Why asthma still kills: The national review of asthma deaths (NRAD) confidential enquiry report. Royal College of Physicians.
Khattab A, Madkour A, Ambaram A, Smith C, Muhwa CJ, Mecha JO et al (2022) Over-prescription of short-acting β 2 -agonists is associated with poor asthma outcomes: results from the African cohort of the SABINA III study. Curr Med Res Opin. 27:1–13
Neffen H, Chahuàn M, Hernández DD, Vallejo-Perez E, Bolivar F, Sánchez MH et al (2020) Key factors associated with uncontrolled asthma–the Asthma Control in Latin America Study. Journal of Asthma. 57(2):113–122
Belachew EA, Tadess S, Alemayehu M, Ayele EM (2022) Level of asthma control and its determinants among adults living with asthma attending selected public hospitals in northwestern, Ethiopia: using an ordinal logistic regression model. Asthma Res Pract. 8(1):5
Chen E, Miller GE (2007) Stress and inflammation in exacerbations of asthma. Brain, behavior, and immunity. 21(8):993–999
Ritz T, Wittchen H-U, Klotsche J, Mühlig S, Riedel O (2016) Asthma trigger reports are associated with low quality of life, exacerbations, and emergency treatments. Annals of the American Thoracic Society. 13(2):204–211
Zeiger RS, Schatz M, Dalal AA, Chen W, Sadikova E, Suruki RY et al (2017) Blood eosinophil count and outcomes in severe uncontrolled asthma: a prospective study. The Journal of Allergy and Clinical Immunology. In Practice. 5(1):144–153
Jackson DJ, Humbert M, Hirsch I, Newbold P, Gil EG (2020) Ability of serum IgE concentration to predict exacerbation risk and benralizumab efficacy for patients with severe eosinophilic asthma. Advances in therapy. 37(2):718–729
Austin D, Pouliquen I, Yancey S, Bleeker E (2016) A blood eosinophil count of greater than 150 cells/uL predicts sputum eosinophilia≥ 3% in patients with severe asthma with other markers of inflammatory lung disease. InB101. PHENOTYPING OF ASTHMA IN THE ERA OF BIOMARKERS AND OMICS. American Thoracic Society, p A4338–A4338
Barbarot N, Nourry E, Massart N, Legay F, Debarre M, Fillatre P et al (2022) Treating acute severe eosinophilic asthma with IL-5 inhibitors in ICU. Case Rep Pulmonol. 21(2022):2180795
Haselkorn T, Szefler SJ, Chipps BE, Bleecker ER, Harkins MS, Paknis B et al (2020) Disease burden and long-term risk of persistent very poorly controlled asthma: TENOR II. The Journal of Allergy and Clinical Immunology. In Practice. 8(7):2243–2253
Kole TM, Berghe EV, Kraft M, Vonk JM, Nawijn MC, Siddiqui S, Sun K, Fabbri LM, Rabe KF, Chung KF, Nicolini G (2022) Predictors and associations of the persistent airflow limitation phenotype in asthma: a post-hoc analysis of the ATLANTIS study. Lancet Respir Med
Bloom CI, Palmer T, Feary J, Quint JK, Cullinan P (2019) Exacerbation patterns in adults with asthma in England. A population-based study. American journal of respiratory and critical care medicine. 199(4):446–453
Download references
Acknowledgements
Author information, authors and affiliations.
Chest Department, Faculty of Medicine, Assiut University Hospital, Assiut University, Assiut, 71515, Egypt
Ashraf Zin E L-Abdeen Mohamed, Lamiaa Hassan Shaaban, Shereen Frghaly Gad & Waleed Gamal Elddin
Assiut Chest Hospital, Assiut, 71515, Egypt
Esraa Abdel Azeem
You can also search for this author in PubMed Google Scholar
Contributions
AZEM, LHS, SSF: conception and design. WGE and EA: data collection. EA: statistical analysis. LHS and WGE: medical writing. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Waleed Gamal Elddin .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the institutional review board and ethical committee of Faculty of Medicine- Assiut University in compliance with the Helsinki Declaration (IRB: 17100097).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mohamed, A.Z.E.LA., Shaaban, L.H., Gad, S.F. et al. Acute severe asthma in emergency department: clinical characteristics, risk factors, and predictors for poor outcome. Egypt J Bronchol 16 , 57 (2022). https://doi.org/10.1186/s43168-022-00160-8
Download citation
Received : 03 July 2022
Accepted : 22 October 2022
Published : 08 November 2022
DOI : https://doi.org/10.1186/s43168-022-00160-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Severe asthma
- Hospitalization
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Pediatr Adolesc Med
- v.6(2); 2019 Jun
Management of asthma exacerbation in the emergency departments
1. introduction.
Asthma is one of the most common pediatric emergencies among children throughout the world, where an estimated 300 million individuals are affected [ 1 ]. The prevalence of asthma in Saudi Arabia is 23% according to Alfrayeh [ 2 ]. Most asthma is uncontrolled and Jahdali estimated that up to 64% of patients have uncontrolled asthma [ 3 ]. Morbidity related to asthma has also increased in recent years. In addition, hospitalization for asthma has increased [ 4 ]. However, mortality due to asthma is decreasing worldwide [ 5 ]. Asthma is one of the main causes of health care utilization and the costs related to asthma are increasing [ 6 ]. Approximately 50% of pediatric asthma cases are still uncontrolled in Saudi Arabia, even in tertiary centers [ 7 ]. Numerous guidelines are available online and the guidelines of the Saudi Initiative for Asthma (SINA), which were updated in 2016, are very useful for the pediatric age group [ 8 ]. The availability of asthma guidelines can improve the outcomes of asthma in children [ 9 ].
In general, asthma treatments that involve the administration of oxygen, inhaled bronchodilators, systemic steroids, and anticholinergic agents are common, and these agents are the main forms of therapy. Frequent assessments and monitoring the response to these therapies are crucial for tailoring medications to needs. In this study, we aimed to minimize the controversy regarding asthma exacerbation management by providing the best evidence for patient care according to the resources available at a specific institute [ 10 ].
1.1. Definition of exacerbation
Asthma exacerbation is recognized clinically based on the following features: progressive increase in shortness of breath, coughing, wheezing, or chest tightness, and a progressive reduction in lung function that requires medical intervention [ 5 , 11 ]. An exacerbation may include an increase in coughing, especially when the child is asleep, a decrease in exercise tolerance, impairment of daily activities, and acute or sub-acute increases in wheezing or shortness of breath [ 12 , 13 ].
1.2. Goal of therapies
- • Assessing the severity of an exacerbation.
- • Correcting hypoxemia/hypercarbia and rapidly reversing the airflow obstruction by using appropriate and prompt medical interventions.
- • Preventing complications that might occur, such as air leakage.
- • Ensuring the appropriate disposition of the patient after initial therapies are provided at the emergency department.
- • Reducing the possibility of recurrence by providing adequate baseline control therapies and arranging follow-up [ 8 , [13] , [14] , [15] ].
1.3. Initial assessment and severity
Acute asthma exacerbation is a medical emergency that should be diagnosed and managed immediately [ 11 ]. The treatment of asthma exacerbation depends on the severity of the exacerbation. The assessment of an asthma exacerbation is a continuous process with two different stages: (1) a static assessment to determine the severity of the attack, and (2) frequent assessments to evaluate the response to treatment. Overall, the assessment process requires the analysis of several factors [ 5 ]. Different scoring systems exist, such as the Asthma Scoring System or Pediatric Respiratory Assessment Measure (PRAM). The SINA group adopted the PRAM scoring system as a valid and reliable scoring system for assessing the severity of exacerbation in children aged 2–17 years [ 8 ]. The PRAM score is a 12-point score based on the oxygen saturation, suprasternal retractions, scalene muscle contractions, air entry, and wheezing [ 12 ]. The PRAM clinical pathway for inpatient management has been shown to decrease the length of stay in the emergency department and with no adverse outcomes. The SINA expert panel recommends determining the PRAM score for asthmatic patients in the emergency department to categorize the risk of hospital admission [ 8 , 16 , 17 ].
- • Total score of 1–3: Low risk (<10%) of hospital admission.
- • Total score of 4–7: Moderate risk (10–50%) of hospital admission.
- • Total score of 8–12: High risk (>50%) of hospital admission.
1.4. Medical history
A brief history should be obtained for any exacerbation. The objective of taking the history is to determine the duration of symptoms and the severity of the exacerbation. Therefore, it is necessary to determine precipitating factors, including medications the child has been given, any previous exacerbations such as previous admissions, number of bronchodilators used, courses of steroids, environmental triggers, compliance, psycho-social factors, and risk factors for death in intensive care unit (ICU), including previous pediatric ICU (PICU) admission, intubation, severe life-threatening conditions, and deterioration while taking systemic steroids [ 13 , 18 ].
1.5. Physical examination
A physician should inspect the patient thoroughly and focus on the patient's general appearance and vital signs. Is the child able to lie down, or does he or she prefer a sitting position? Is the child sweating, using accessory muscles to talk, or wheezing audibly? It should be noted that although the degree of wheezing is not correlated with the severity of obstruction, a silent chest is an ominous sign. Agitation, confusion, and mental drowsiness are extreme signs of cerebral hypoxia, which requires immediate intervention. Each patient should be screened for risk factors for fatal asthma ( Table 1 1,12,13,15 ). Objective evaluations of disease severity and response to therapy are most important, and scores for objective measures should be obtained. Frequent assessment is crucial. The lung function test (spirometry) is difficult to perform in younger children age, especially in those aged less than 6 years during exacerbation, and the results may not correlate with the asthma scoring system. Therefore, spirometry is unreliable in children [ 19 , 20 ].
Table 1
Risk factors for death from asthma.
ICU: Intensive Care Unit, Adapted from British Thoracic Society, Scottish Intercollegiate Guidelines Network. “British Guideline on the Management of Asthma,” Revised 2018.
Recommendation: The severity level of any patient with an exacerbation should be assessed using both clinical and objective evaluations, including pulse oximetry or blood gas in severe cases.
1.6. Oxygen therapy
Hypoxia is the primary cause of death from exacerbation, and oxygen may help to decrease dyspnea, aid bronchodilation, support the myocardium, and minimize the risk of arrhythmia [ 21 ]. Oxygen should be titrated to achieve saturation ≥ 94% [ 8 , 12 , 15 ]. Oxygen will not suppress respiratory drive in the absence of preexisting CLD [ 20 ]. Oxygen saturation < 92% in room air can predict admission [ 8 , 13 , 22 , 23 ].
Recommendations : Oxygen supplements should be provided for patients with oxygen saturation levels below 92% in room air, and patients should be weaned from oxygen when the saturation level exceeds 94%.
Beta2 agonist bronchodilators: A bronchodilator trial should occur during an asthma exacerbation. Most researchers prefer metered-dose inhalers (MDIs) with a spacer to nebulizers. These inhalers are the first choice for pediatric asthma exacerbations, and strong evidence (evidence based medicine-A) supports their use for mild to moderate exacerbations [ 8 , 12 , 14 , 15 , 24 ]. The recommended doses for pediatric patients are 4–5 puffs for children < 20 kg and 6–10 puffs for those > 20 kg. Nebulization should be limited to: severe patients <5 years: 2.5 mg/3–4 ml, and >5 years: 5.0 mg/3–4 ml (see Table 2 ) [ [25] , [26] , [27] , [28] , [29] , [30] ]. MDIs and nebulizers are equally effective methods for delivering beta2 agonists to children with acute asthma and mild to moderate exacerbations.
Table 2
Summary recommendations for bronchodilator according to common international asthma guidelines.
GINA : Global Initiative National for Asthma; PRAM : Pediatric Respiratory Assessment Measure; SINA : Saudi Initiative for Asthma; SIGN : Scottish Intercollegiate Guidelines Network (British guide); NS : normal saline.
Recommendations : Inhaled short-acting beta2-agonist should be administered as the drug of choice for rapid reversal of airflow obstruction.
Recommendations: MDIs improve discharge from the emergency department and shorten the duration of stay, and they are either equally effective or superior to nebulizers for mild to moderate exacerbations.
Recommendations: Nebulization should be reserved for severe exacerbations or for patients who do not respond well to oxygen-driven MDIs.
Recommendations: Continuous nebulized salbutamol is more effective than intermittent treatment in severe cases.
1.7. Anticholinergic agents
The role of anticholinergics in acute asthma management is not well defined. However, ipratropium bromide is commonly added to an inhaled bronchodilator in the emergency department, which can lead to synergistic effects with the bronchodilator [ 31 , 32 ]. Ipratropium bromide is also often administered as a regular medication after admission [ 33 ]. The current best evidence for anticholinergic treatment confirms that multiple doses may be given in an emergency but that its use should be limited to moderate to severe cases. This treatment may reduce admission by 30–60% and with no apparent significant side effects. There are apparent benefits from the use of single doses of anticholinergic in asthma with mild exacerbation, or any added benefit due to administration after admission [ 34 ]. Anticholinergics are less effective than inhaled beta-agonists and they should not be used alone [ 35 ].
Recommendations: Anticholinergic treatment is recommended for moderate to severe exacerbations rather than for mild cases.
Recommendations: Anticholinergics should not be used alone or more than 24 h after admission.
1.8. Steroids
Steroid should be limited for children with moderate to severe asthma exacerbations (evidence based medicine-A) [ 8 , 12 , 23 , 36 ]. Different mechanisms allow steroids to interfere with leukotriene and prostaglandin synthesis, prevent cell migration, and upregulate airway b receptors, which can accelerate the resolution of the exacerbation, decrease hospitalization, and facilitate earlier discharge from the emergency department (evidence based medicine-A) [ [37] , [38] , [39] ]. Different steroid regimens are recommended ( Table 3 ). Oral prednisone is the most convenient and least expensive steroid, and its effects are equivalent to those of intravenous methylprednisolone. However, methylprednisolone is the preferred medication when the patient is sick or unable to tolerate oral or IV medications. Oral dexamethasone is equivalent to several days of oral prednisolone [ [40] , [41] , [42] , [43] , [44] ]. Studies have shown that divided doses of oral steroids (AM and PM doses) minimize the symptoms late at night, and that tapering the steroid is not necessary if it is used for one week or less.
Table 3
Types and doses of steroids used for asthma exacerbation [ 8 , 12 , 14 , 19 , [39] , [40] , [41] ].

Recommendations : Steroids should be used in moderate or severe cases.
Recommendations : Steroids decrease admission and relapse if given during the first hour of an exacerbation.
Recommendations: Oral steroids are the most convenient and least expensive route of administration.
Recommendations: IV steroids should be administered to patients who do not respond to oral therapy.
Recommendations: One dose of dexamethasone is equal in efficacy to several days of prednisolone.
Recommendations : It is not necessary to wean patients from steroids if they are used for less than 7 days.
1.9. Inhaled corticosteroids for acute asthma
Multiple trials of different types of inhaled corticosteroids for asthma exacerbations have determined minimal improvements in the respiratory scores. However, no convincing evidence is available regarding their use as an add-on therapy for severe asthma exacerbations [ 23 , [45] , [46] , [47] , [48] , [49] , [50] , [51] ].
Recommendations : High-dose inhaled steroids are not recommended for acute asthma attacks.
1.10. Fluids
Patients are often dehydrated because of an increased basal metabolic rate and euvolemia is recommended. Syndromes resulting from inappropriate ADH are very rare but they may be considered in the presence of hyponatremia with markedly reduced urine output [ 14 , 52 ].
Recommendations: Euvolemia is recommended unless there are signs of dehydration or suspected SIADH .
Recommendations: Aggressive rehydration should be avoided during asthma exacerbation.
1.11. Antibiotics
The use of antibiotics for asthma exacerbation caused by viral illness is not necessary.
However, antibiotics may be considered if the patient has a high temperature and appears toxic, there is evidence of consolidation on the chest X-ray, or the patient expectorates purulent sputum with the presence of polymorphs [ 8 , 12 , 14 ].
Recommendations: Antibiotics should not be used to treat asthma exacerbation unless bronchopneumonia or another focus of infection is suspected.
1.12. Chest X-ray
Chest X-rays are obtained excessively in asthma exacerbation. Furthermore, the misinterpretation of peribronchial opacity as pneumonic infiltrate is common and can lead to the prescription of unnecessary medications [ 13 , 53 ].
Recommendations : Chest X-rays should be limited to the following conditions:
- 1. Status asthmaticus (the patient is not responding to standard therapy);
- 2. Presence of complications, e.g., barotrauma pneumothorax or pneumomediastinum;
- 3. Suspected bronchopneumonia;
- 4. Suspicion of a foreign body as the cause of wheezing and respiratory distress.
1.13. Serum electrolytes
The measurement of serum electrolytes is important in severe asthma, particularly for monitoring the serum potassium levels. The frequent use of ventolin to treat status asthmaticus may cause hypokalemia, and acidosis may result in transient hyperkalemia [ 8 , 14 , 15 ].
Recommendations: Electrolytes should be monitored in severe asthma exacerbation, especially potassium and lactate.
Serum glucose : Blood sugar levels are often affected in asthma exacerbation in children due to stress, infection, and the use of beta-agonists and corticosteroids. Hyperglycemia may be a predictor of longer admission [ 54 ]. However, younger children are more susceptible to hypoglycemia in response to infection because of their poor reserves.
Recommendations: Blood sugar should be monitored in severe asthma exacerbation.
1.14. Complete blood cell count (CBC)
Cell counts and differentials are commonly requested in the emergency department in the majority of cases of asthma exacerbation. Leukocytosis is common but neutrophilia should be interpreted with caution because beta-agonists and corticosteroids may result in the demargination of white cells and an increase in the peripheral white cell count with a predominant left shift [ 14 , 30 ]. Recommendations: CBC should not be performed routinely in cases of asthma exacerbation and leukocytosis could be a result of dermargination.
Viral study: It well known that viruses are the main trigger of asthma exacerbation [ 8 ].
Recommendations : Screening for viral illness should be limited to moderate or severe exacerbations or admitted cases, and it may aid in the discontinuation of unnecessary antibiotics [ 14 , 30 ].
1.15. Blood gas analysis
Recommendations : This analysis is not routinely required for asthma exacerbation. Asthma exacerbation is a clinical diagnosis and blood gas analysis should be limited to at least moderate exacerbations or patients who exhibit a suboptimal response to standard asthma therapy. [ 8 , 13 , 14 ].
1.16. Magnesium sulfate
Magnesium is an important cofactor in numerous enzymatic reactions, including the inhibition of calcium uptake in smooth muscles to cause muscle relaxation [ 55 , 56 ]. Magnesium may also inhibit cholinergic transmission, stimulate nitric oxide and prostacyclin synthesis, and stabilize mast cells and T-lymphocytes [ 57 ]. Meta-analyses and systematic reviews have demonstrated the effect of intravenous magnesium. Magnesium is administered in moderate to severe asthma exacerbations. The usual recommended dose is 25–75 mg/kg/20 min initially and then every 6 h as needed. IV magnesium is safe and beneficial for moderate to severe asthma exacerbations at doses of 4–6 mg/dl, but it exhibits toxicity at >12 mg/dl. Nausea and flushing are common side effects, and muscle weakness, hyporeflexia, and respiratory depression are manifestations of toxicity. Renal impairment and heart blockage are contraindications. Some studies obtained minimal evidence supporting the use of nebulized magnesium sulfate, especially in severe cases, depending on the scoring system or pulmonary function results [ [58] , [59] , [60] , [61] , [62] , [63] ].
Recommendations: Magnesium sulfate may be given for moderate to severe asthma exacerbations in patients who exhibit minimal responses to bronchodilators and steroids. [ [64] , [65] , [66] , [67] , [68] , [69] , [70] ].
Recommendations: Insufficient data are available to support recommending the use of inhaled magnesium sulfate for severe asthma exacerbation.
1.17. Salbutamol
This treatment should be limited for patients with status asthmaticus who fail to respond to a continuous nebulized beta2-agonist. IV salbutamol improves lung function tests and gas exchange [ 71 ] but its toxicity increases as the concentration increases [ 72 ]. IV salbutamol should be limited to use in the pediatric ICU, where continuous cardiac monitors are available. Cardiac toxicity signs such as arrhythmia and significant tachycardia are common side effects of this medication. In an emergency, we recommend an initial dose of 15 μg/kg over 10 min under cardiac monitoring, and electrolyte measurement to avoid potential hypokalemia and increased lactate. Infusion should only occur in the ICU as indicated. Some researchers consider that there is no extra benefit of IV salbutamol compared with continuous salbutamol nebulization [ 73 , 74 ]. Recommendations: IV salbutamol may be administered under cardiac monitoring in refractory patients who do not respond to standard asthma therapy .
1.18. Aminophylline
This bronchodilator is unlikely to provide additional bronchodilatory effects compared with standard therapy (i.e., continuous inhaled beta2 agonist, ipratropium bromide, and IV steroids) and it should be reserved for children with severe asthma exacerbations who fail to improve despite maximized therapy after consulting a pediatric intensivist. The effects of aminophylline on patient oxygenation, duration of ventilation, and length of stay in PICU are still unknown. Side effects such as vomiting or dysrhythmia are common due to its narrow therapeutic range. Therefore, this medication should not be used without permission from the intensivist and it should be administered under patient cardiac monitoring. The general recommended dose is aminophylline infusion at 5 mg/kg over 20 min, followed by 0.9 mg/kg/h [ 75 ]. Aminophylline has a widely accepted therapeutic range of 10–20 mg/l, which determines dosing decisions in children [ 76 ].
Recommendation: Aminophylline should not be used for mild to moderate asthma exacerbation.
Recommendations: IV aminophylline should be reserved for severe asthma patients who fail to improve despite maximum therapy in the PICU, and its use may increase the frequency of adverse effects during an exacerbation [ [77] , [78] , [79] , [80] ].
1.19. Inhaled heliox
A gas mixture of oxygen and helium (heliox) is commonly administered at a concentration ratio of 80:20 to decrease the progression of respiratory failure and prevent intubation. This mixture also increases laminar flow and reduces turbulent flow. Heliox should be reserved for patients with severe asthma exacerbation who fail to respond to maximum therapies in the ICU [ 13 , 14 , 23 , [81] , [82] , [83] , [84] ].
Recommendation: Heliox-driven salbuterol nebulization might be considered in any patient with life-threatening exacerbation or with severe exacerbation that persist after intensive conventional adjunctive therapies.
1.20. Noninvasive PPV (NIPPV)
NIPPV is a safe and effective treatment for status asthmaticus in pediatric patients. It can prevent intubation as well as reducing mortality and treatment costs. Therefore, its use has become frequent. The main mechanism involves stenting the airway combined with the a bronchodilator, which induces alveolar recruitment [ [85] , [86] , [87] , [88] , [89] , [90] ].
Recommendation: NIPPV use should be encouraged in refractory cases with the supervision of an intensivist.
Indications for ICU admission: The indications for admission to the ICU vary widely among centers [ 13 ]. The indications are summarized as follows [ 13 , 23 ].
- • Failure to exhibited a sustained clinical response to continuous bronchodilators and steroids;
- • Worsening of gas exchange;
- • Apparent fatigue or exhaustion;
- • Changes in the level of sensorium.
1.21. Endotracheal intubation and ventilation in asthmatic patients with respiratory failure
Intubation and mechanical ventilation are expected in less than 10% of cases admitted to the PICU, including lifesaving efforts for severe asthma attacks with respiratory failure. However, their use in children is commonly associated with significant complications, e.g., hypotension or pneumothorax, which occur in up to 50% of cases. Therefore, intubation should be avoided as much as possible [ 85 ,91−93]].
Recommended The indications under the supervision of a pediatric intensivist are as follows:
- • Respiratory or cardiac arrest;
- • Progressive hypoxemia despite O 2 or NIPPV administration;
- • Progressive rising PaCo 2 despite maximum therapy and/or NIPPV;
- • Deterioration of mental status;
- • Progressive exhaustion.
1.22. Recommendations
Intubation should be avoided as much as possible and only used as a last resort and under the supervision of a pediatric intensivist [ 13 , 85 ].
Intubation: Clinicians should follow the rapid sequence intubation protocol, where intubation should be conducted cautiously under cardio-respiratory monitoring by the most expert clinician in the unit [ 85 ]. Rapid ventilation during resuscitation should be avoided. Aim to ensure adequate oxygenation and sufficient gas exchange.
Setting: Controlled mechanical ventilation should be provided using the most familiar mode. However, PRVC is the optimum mode of ventilation for asthmatic patients. The goal is to save the child. Permissive hypercapnia may be beneficial using the following strategy: slow rate, low tidal volume (approximately 5 ml/kg), short inspiratory time ratio to allow time for exhalation and washout of PCO 2 , Fi O 2 with 100% oxygen, and use fo physiological PEEP [ [91] , [92] , [93] ].
Disposition: Patients may be discharged when they have been extubated successfully with a stable hemodynamic status, have been weaned off continuous intravenous beta-agonists and are stable under intermittent beta-agonist aerosol therapy for more than 3 h [ 13 , 14 ]. Education has been proven to minimize the risk of re-admission or unscheduled visits to the emergency department. Follow-up should be conducted for any exacerbation to ensure that the patient is doing well after discharge.
Recommendations Education should be provided for any asthmatic patient and their families prior to discharge from the emergency department or inpatient unit. Education should be provided by an asthma educator or any staff trained in the field of asthma to ensure that the families understood the nature of asthma, the signs and symptoms of asthma, how to use asthma medications, how to recognize the risk factors, and when to ask for medical support [ 36 , 45 ]
Admission criteria [ 8 , 13 , 23 , 30 ]
- - An ongoing need for supplemental oxygen despite initial treatment.
- - A need for frequent beta2-agonist therapy (more than 3 h).
- - Any feature of life-threatening asthma.
- - Previous near-fatal event.
- - Exacerbation despite use of oral steroids.
- - Underlying psychosocial conditions.
- - Exacerbation despite adequate doses of oral steroids and presenting again.
- - Residence in a remote location or without transportation/communication.
Discharge criteria [ 8 , 13 , 23 , 30 ]
- - Need for beta2-agonists every 4–6 h.
- - Minimal signs of respiratory distress.
- - Saturation more than 92% in room air.
- - Good air entry.
- - No psychosocial illness.
2. Conclusion
The management of asthma exacerbation in children remains a challenge for public health systems, and thus we have provided updated guidelines in this review. Previous studies support MDI salbutamol as the best beta2 agonist of choice. Ipratropium bromide is effective in moderate to severe cases, and steroids are indicated for moderate and severe exacerbations. The first hour is the optimal treatment time, and medications should be adjusted according to progression, severity, and response to the asthma therapy. Inhaled steroids play no role in exacerbation. Magnesium sulfate administration is encouraged for patients who did not respond well to the initial therapy, and the use of aminophylline should be limited to severe cases in the PICU. Heliox and noninvasive ventilation may be used to prevent intubation. Intubation should be avoided, and clinicians should take great caution during intubation, which should always be performed by an expert. These guidelines require implementation and revision. It should be noted that exacerbation is a failure of the underlying regimen, which requires urgent revision and follow-up with a primary doctor after the parents have been fully educated.
Acknowledgments
Acknowledgment to the Saudi Pediatric Pulmonology Association (SPPA) for supporting this manuscript.
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Heat-Related Emergency Department Visits — United States, May–September 2023
Weekly / April 18, 2024 / 73(15);324–329
Ambarish Vaidyanathan, PhD 1 ; Abigail Gates, MSPH 2 ; Claudia Brown, MDP 1 ; Emily Prezzato, MPH 1 ; Aaron Bernstein, MD 3 ( View author affiliations )
What is already known about this topic?
Unprecedented heat waves can affect all persons, but some are more sensitive to the effects of heat, including children and adults with underlying health conditions, pregnant women, and outdoor workers.
What is added by this report?
During the 2023 warm-season months (May–September), rates of emergency department visits for heat-related illness substantially increased across several U.S. regions compared with previous years, especially among males and adults aged 18–64 years.
What are the implications for public health practice?
Heat-related illness will continue to be a significant public health concern as climate change results in longer, hotter, and more frequent episodes of extreme heat. By monitoring heat-related health impacts, public health agencies can detect trends in health care utilization rates, identify subpopulations at increased risk, and guide public health actions tailored to specific heat exposure levels.
- Article PDF
- Full Issue PDF

Unprecedented heat waves can affect all persons, but some are more sensitive to the effects of heat, including children and adults with underlying health conditions, pregnant women, and outdoor workers. Many regions of the United States experienced record-breaking high temperatures in 2023, with populations exposed to extremely high temperatures for prolonged periods. CDC examined emergency department (ED) visits associated with heat-related illness (HRI) from the National Syndromic Surveillance Program and compared daily HRI ED visit rates during the warm-season months (May–September) of 2023 with those during 2018–2022. In the 2023 warm-season months, daily HRI ED visit rates peaked in several regions and remained elevated for a prolonged duration. More males than females sought care in EDs for HRI, especially males aged 18–64 years. CDC issued multiple public health alerts using the Epidemic Information Exchange system to bring attention to increases in ED utilization for HRI. Deaths and illnesses associated with heat exposure are a continuing public health concern as climate change results in longer, hotter, and more frequent episodes of extreme heat. Near real-time monitoring of weather conditions and adverse health outcomes can guide public health practitioners’ timing of risk communication and implementation of prevention measures associated with extreme heat.
Introduction
The warm-season months (May–September) of 2023 were the hottest ever recorded in the United States,* and adverse health impacts, including deaths and illnesses attributable to high ambient temperatures, received considerable attention. † Hot weather conditions can affect all persons; however, for certain specific populations, exposure and health risks are compounded by adverse physiologic, behavioral, demographic, or socioeconomic factors that result in their being disproportionately affected by extreme heat ( 1 ). Populations at highest risk typically include older persons, children and adolescents, persons with preexisting health conditions, pregnant women, outdoor workers, persons with limited access to cooling resources, and persons living in low-income communities. § Further, exceptionally hot conditions can increase the demand for medical services and strain health systems (e.g., a surge in persons seeking emergency department [ED] care) ( 2 ). Successful public health measures to reduce heat-related illness (HRI), including targeted communication and outreach campaigns for populations at risk, require coordination across various health care sectors and are often guided by near real-time assessments of heat exposure and its resulting adverse health impacts. To assess the health impact of exceedingly high temperatures observed during the warm-season months of 2023, CDC analyzed National Syndromic Surveillance Program (NSSP) data to compare daily HRI ED visit rates during May–September 2023 with those during May–September 2018–2022.
Data Sources
Data on HRI ED visits ¶ occurring during January 2018–December 2023 were extracted from NSSP’s Electronic Surveillance System for the Early Notification of Community-Based Epidemics (ESSENCE).** The daily number of HRI and all-cause ED visits were tabulated for each of the 10 U.S. Department of Health and Human Services (HHS) regions. †† NSSP data were analyzed to compare the 2023 heat season with the 2018–2022 seasons. To account for temporal changes among facilities sharing data with NSSP, comparisons between 2023 and previous years were restricted to those EDs with consistent reporting during the study period. §§
Descriptive and Statistical Analyses
After applying data quality filters to reduce artifactual changes in reporting patterns during 2018–2023, a maximum of 826 (range = 3–826; median = 36) ED facilities that participate in NSSP reported one or more visits associated with HRI. The HHS region–specific daily HRI ED visit rate (the number of ED visits for HRI per 100,000 all-cause ED visits) observed during the warm-season months of 2023 was compared with the 95th percentile value of the daily HRI ED visit rate distribution. The 95th percentile for each region was computed based on HRI ED data recorded for the 2018–2022 warm-season months.
Differences in HRI ED visit rates were evaluated by age group (0–17, 18–25, 26–54, 55–64, 65–74, and ≥75 years), sex, HHS region, and occurrence of the HRI ED visits during the hotter warm-season months (i.e., July and August). Rate ratios (RRs) and associated 95% CIs were estimated using a multivariate Poisson regression model. The daily number of HRI visits was regressed against predictors such as age group, sex, HHS region, and an indicator to denote the occurrence of HRI ED visits during the hotter warm-season months of July and August. The model also included the logarithm of all-cause ED visits to account as an offset term. For each predictor, the category with the lowest warm-season HRI ED visit rate was identified as the referent population. Regressions were executed for 2023 and 2018–2022 with the same model specifications and parameters. Analysis and visualization were conducted using R software (version 4.1.2; R Foundation) and SAS software (version 9.4; SAS Institute). This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy. ¶¶
Characteristics of HRI ED Visits
During January 1–December 31, 2023, a total of 119,605 HRI ED visits were recorded in the ESSENCE system***; 92% of these visits occurred during May–September. Across the study period, July and August accounted for a higher average HRI ED visit rate (303 per 100,000 ED visits) compared with other warm-season months (May, June, and September) (97) ( Table 1 ). Further, the risk observed during July–August 2023 was more than three times that during May, June, and September (mean RR = 3.07), consistent with record-breaking temperatures observed across several HHS regions in 2023. ††† In comparison, the risk observed in July–August 2018–2022 was approximately twice as high as that of May, June, and September of the same period.
Demographic Characteristics of Persons with HRI ED Visits
In 2023, among the demographic groups considered, higher rates of HRI ED visits were observed among males (271 per 100,000 ED visits) than among females (104) and among adults aged 18–64 years (range = 207–222) than adults aged ≥65 years (range = 120–173). In addition, the risk for HRI ED visits among adults aged 18–25 and 26–54 years was approximately 2.5 times the risk in the referent population (persons aged <18 years).
Regional Differences in HRI ED Visits
HHS regional differences in warm-season HRI ED visit rates were observed in 2023. The lowest average warm-season HRI ED visit rate (51 per 100,000 ED visits) was reported by HHS Region 2 (New Jersey and New York), whereas the highest rate was reported by Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) (483). Compared with Region 2 (the referent region), the HRI ED visit risks for regions 4, 6, 7, and 9 in 2023 were 1.5–2.5 times those during 2018–2022.
Daily HRI ED visit rates during the warm-season months in 2023 for several regions exceeded the 95th percentile of the daily HRI ED visit rate distribution for the warm-season months during 2018–2022 for multiple periods of ≥3 consecutive days in some regions (Supplementary Figure, https://stacks.cdc.gov/view/cdc/153146 ). For instance, in regions 6 and 9, HRI ED rates in July 2023 exceeded the 2018–2022 95th percentile for 16 and 18 consecutive days, respectively. In the warm-season months of 2023, every HHS region experienced ≥1 day above the 95th percentile ( Table 2 ). In regions 4, 6, 7, and 9, the number of days with HRI ED visit rates exceeding the 95th percentile was higher than that in any previous year in the study period. In Region 6 alone, more than one third (37%; 56) of the days during the warm season of 2023 had daily HRI ED visit rates exceeding the 95th percentile. Regions 6 and 7 experienced days with the highest rate of HRI ED visits ever recorded in the ESSENCE system for their respective region since 2018.
In recent years, health emergencies caused by heat exposure have become more frequent and widespread in the United States ( 1 ). The severity, frequency, and duration of heat waves in 2023 in some HHS regions resulted in record-high rates of HRI ED visits during the year, which prompted CDC to issue Epidemic Information Exchange (Epi-X) public health alerts. §§§
The finding of increased risk for HRI ED visit rates among certain demographic groups in 2023, particularly among males and adults aged 18–64 years, is similar to findings reported in other studies ( 3 ). Although the lowest HRI ED visit rates occurred among persons aged <18 years, previous studies of children and adolescents in different age groups suggest that children might also be subject to the effects of heat exposure at rates similar to those among adults in some areas of the United States ( 4 ). Persons who work outdoors might regularly endure extreme heat; this group warrants particular attention because of the high prevalence of HRI ED visits observed in working-aged adults. Frontline essential workers tending to emergencies, such as firefighters, might be at particularly high risk for exposure to heat stress ( 5 ). Regional differences in rates of HRI ED visits might reflect differential acclimatization, behavioral responses, and adaptation strategies ( 1 , 6 ). Understanding the causes of these differences can help guide the development and implementation of public health interventions, such as heat action plans and issuance of heat alerts calibrated based on local epidemiologic data (e.g., HeatRisk). ¶¶¶
Effective implementation of heat mitigation strategies is associated with social determinants of health. For example, even in areas with high rates of air conditioning, such as the South and southeastern United States, persons exposed to extreme heat might have limited or no access to cooling spaces ( 1 ). Factors that affect air conditioning use and access to cooling spaces include energy costs**** and the occurrence of outages due to power grid failure ( 1 , 7 , 8 ). HHS programs that provide financial assistance for residential energy †††† and monitor the safety of persons reliant on electricity-dependent durable medical equipment in case of power outages during extreme heat §§§§ can protect populations affected by heat stress. The intersection of communities with a high proportion of groups at risk, especially those with limited access to health care, with areas that experience persistent high ambient temperatures (e.g., heat islands or lack of green spaces) could be more susceptible to the effects of heat exposure ( 1 ). Public health initiatives can be designed to help communities prepare for extreme heat conditions and complement the efforts of weather and emergency management agencies, reducing illnesses and deaths. Tools used for syndromic surveillance, including ESSENCE, local systems, and visualization dashboards, help guide and strengthen public health preparedness and response. An example is CDC’s Heat and Health Tracker ( https://ephtracking.cdc.gov/Applications/heatTracker/ ), which provides local heat and health information for communities.
Limitations
The findings in this report are subject to at least five limitations. First, NSSP data are not nationally representative, and participation can vary by HHS region. Second, although the prevalence of HRI among U.S. military veterans has been increasing ( 9 ), this analysis does not include facilities operated by U.S. Department of Veterans Affairs. In addition, the HRI ED visit rate reported by ESSENCE might not be representative of the rate in the general population because ESSENCE is not a population-based system but rather reflects the number of HRI ED visits among all-cause ED visits. Third, HRI information reported at the HHS regional level can obscure subregional variation. Fourth, estimation of HRI ED visit rates might have been affected during the COVID-19 pandemic because overall ED utilization patterns changed for specific subpopulations ( 10 ). Finally, HRI data from the ESSENCE system are based on ED visits only and do not identify cases of HRI among persons who sought treatment elsewhere, likely resulting in an underestimation of HRI prevalence.
Implications for Public Health Practice
The record-breaking temperatures of the 2023 warm-weather season had a substantial public health impact, and this trend might increase in the coming years because of climate change ( 1 ). Public health agencies rely on tools and surveillance systems to assess the adverse health effects of heat exposure. Timely mechanisms for tracking and reporting health effects, along with the ability to detect anomalous trends, especially during extreme heat emergencies, can facilitate the implementation of public health strategies to protect affected populations.
Acknowledgments
Shubhayu Saha, Paul Schramm, Division of Environmental Health Science and Practice, National Center for Environmental Health, CDC; Sue Swensen, Office of Public Health Data, Surveillance, and Technology, CDC.
Corresponding author: Ambarish Vaidyanathan, [email protected] .
1 Division of Environmental Health Science and Practice, National Center for Environmental Health, CDC; 2 Detect and Monitor Division, Office of Public Health Data, Surveillance, and Technology, CDC; 3 National Center for Environmental Health, Agency for Toxic Substances and Disease Registry, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* https://www.nasa.gov/news-release/nasa-announces-summer-2023-hottest-on-record/
† https://www.whitehouse.gov/briefing-room/statements-releases/2023/07/27/fact-sheet-president-biden-to-announce-new-actions-to-protect-workers-and-communities-from-extreme-heat
§ https://www.cdc.gov/disasters/extremeheat/index.html
¶ HRI ED visits were identified using administrative discharge diagnosis codes and free text search of the patient’s reason for visit (i.e., their chief complaint). https://knowledgerepository.syndromicsurveillance.org/heat-related-illness-v2
** https://publichealth.jmir.org/2021/6/e26303/authors
†† The dataset does not include data from American Samoa, Federated States of Micronesia, Marshall Islands, Northern Mariana Islands, Palau, Puerto Rico, or the U.S. Virgin Islands. https://www.hhs.gov/about/agencies/iea/regional-offices/index.html
§§ To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation for ED visits ≤40 and average weekly informative discharge diagnosis ≥70% complete with discharge diagnosis code formatting during January 2018–December 2023. After applying this data quality filter, a maximum of 823 ED (range = 3–823; median = 111) facilities that participate in NSSP returned one or more visits associated with HRI. https://www.cdc.gov/nssp/index.html
¶¶ 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
*** All facilities reporting HRI data to NSSP were considered to obtain the total HRI ED visits reported during January 1–December 31, 2023, across all HHS regions. During this period, HRI data were reported by a maximum of 1,238 EDs (range = 12–1,238; median = 152) that participated in NSSP and returned one or more visits associated with HRI.
††† https://www.ncei.noaa.gov/access/monitoring/monthly-report/global/202313
§§§ On June 30, 2023, and August 23, 2023, CDC issued public health alerts using the Epi-X system upon noticing high levels of heat-related ED visits.
¶¶¶ HeatRisk is a health-based heat forecast developed by the National Oceanic and Atmospheric Administration’s National Weather Service and CDC. It integrates health and temperature data to deliver a 7-day outlook for hot weather. HeatRisk uses a 5-level scale to indicate how risky the heat level is in a specific area. www.cdc.gov/HeatRisk
**** https://neada.org/wp-content/uploads/2023/07/summercoolingestPR.pdf
†††† https://www.acf.hhs.gov/ocs/programs/liheap
§§§§ https://empowerprogram.hhs.gov/
- US Global Change Research Program. The fifth national climate assessment. Washington, DC: US Global Change Research Program; 2023. https://nca2023.globalchange.gov
- Schramm PJ, Vaidyanathan A, Radhakrishnan L, Gates A, Hartnett K, Breysse P. Heat-related emergency department visits during the northwestern heat wave—United States, June 2021. MMWR Morb Mortal Wkly Rep 2021;70:1020–1. https://doi.org/10.15585/mmwr.mm7029e1 PMID:34292925
- Sun S, Weinberger KR, Nori-Sarma A, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study. BMJ 2021;375:e065653. https://doi.org/10.1136/bmj-2021-065653 PMID:34819309
- Bernstein AS, Sun S, Weinberger KR, Spangler KR, Sheffield PE, Wellenius GA. Warm season and emergency department visits to US children’s hospitals. Environ Health Perspect 2022;130:17001. https://doi.org/10.1289/EHP8083 PMID:35044241
- Kim S, Kim D-H, Lee H-H, Lee J-Y. Frequency of firefighters’ heat-related illness and its association with removing personal protective equipment and working hours. Ind Health 2019;57:370–80. https://doi.org/10.2486/indhealth.2018-0063 PMID:30210098
- Hondula DM, Balling RC Jr, Vanos JK, Georgescu M. Rising temperatures, human health, and the role of adaptation. Curr Clim Change Rep 2015;1:144–54. https://doi.org/10.1007/s40641-015-0016-4
- Mallen E, Roach M, Fox L, et al. Extreme heat exposure: access and barriers to cooling centers—Maricopa and Yuma counties, Arizona, 2010–2020. MMWR Morb Mortal Wkly Rep 2022;71:781–5. https://doi.org/10.15585/mmwr.mm7124a1 PMID:35709011
- Andresen AX, Kurtz LC, Hondula DM, Meerow S, Gall M. Understanding the social impacts of power outages in North America: a systematic review. Environ Res Lett 2023;18:053004. https://doi.org/10.1088/1748-9326/acc7b9
- Osborne TF, Veigulis ZP, Vaidyanathan A, Arreola DM, Schramm PJ. Trends in heat related illness: nationwide observational cohort at the US Department of Veteran Affairs. J Clim Change Health 2023;12:100256. https://doi.org/10.1016/j.joclim.2023.100256
- Hartnett KP, Kite-Powell A, DeVies J, et al.; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704. https://doi.org/10.15585/mmwr.mm6923e1 PMID:32525856
Abbreviations: ED = emergency department; HHS = U.S. Department of Health and Human Services; HRI = heat-related illness; NA = not applicable; Ref = referent group; RR = rate ratio. * To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation for ED visits ≤40 and average weekly informative discharge diagnosis ≥70% complete with discharge diagnosis code formatting during January 2018–December 2023. After applying this data quality filter, a maximum of 823 ED (range = 3–823; median = 111) facilities that participate in the National Syndromic Surveillance Program returned one or more visits associated with HRI. https://www.cdc.gov/nssp/index.html † HRI ED visits per 100,000 ED visits. § https://www.hhs.gov/about/agencies/iea/regional-offices/index.html ¶ Region 2 (Ref) includes New Jersey, New York, Puerto Rico, and the U.S. Virgin Islands. Puerto Rico and the U.S. Virgin Islands currently do not report data to the National Syndromic Surveillance Program.
Abbreviations: ED = emergency department; HHS = U.S. Department of Health and Human Services. * 95th percentile based on region-specific heat-related illness ED visit rate during warm-season months (May–September) during 2018–2022. † To reduce artifactual impact from changes in reporting patterns, analyses were restricted to facilities with a coefficient of variation for ED visits ≤40 and average weekly informative discharge diagnosis ≥70% complete with discharge diagnosis code formatting during January 2018–December 2023. After applying this data quality filter, a maximum of 823 ED (range = 3–823; median = 111) facilities that participate in the National Syndromic Surveillance Program returned one or more visits associated with heat-related illness. https://www.cdc.gov/nssp/index.html § https://www.hhs.gov/about/agencies/iea/regional-offices/index.html ¶ Region 2 includes New Jersey, New York, Puerto Rico, and the U.S. Virgin Islands. Puerto Rico and the U.S. Virgin Islands currently do not report data to the National Syndromic Surveillance Program.
Suggested citation for this article: Vaidyanathan A, Gates A, Brown C, Prezzato E, Bernstein A. Heat-Related Emergency Department Visits — United States, May–September 2023. MMWR Morb Mortal Wkly Rep 2024;73:324–329. DOI: http://dx.doi.org/10.15585/mmwr.mm7315a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Emergency department visit for life threatening or functioning severity
Reported Price For STEFAN MICHAEL BRETTFELD
This is the price that STEFAN MICHAEL BRETTFELD has reported for Emergency department visit for life threatening or functioning severity. We have added your insurance plan information to estimate your out-of-pocket cost. Select 'Verify Cost' to confirm with the provider.
- Input Your Info
- Insurance Plan - Select Insurance Plan - Cofinity w/WPS Statewide & First Health for WPS Health Insurance First Health HMO w/WPS Select Plus for WPS Health Plan First Health w/WPS Statewide Auxiant for BADGER UTILITY HOLDINGS LLC First Health w/WPS Statewide Auxiant for BAY-SAN COMPANY, INC. First Health w/WPS Statewide Auxiant for BEST VERSION MEDIA, LLC First Health w/WPS Statewide Auxiant for CAPRI COMMUNITIES LLC First Health w/WPS Statewide Auxiant for CHAMBERS & OWEN First Health w/WPS Statewide Auxiant for CODEWORKS, LLC First Health w/WPS Statewide Auxiant for DENTAL HEALTH PRODUCTS First Health w/WPS Statewide Auxiant for DON JACOBS MOTORS, INC. First Health w/WPS Statewide Auxiant for GROVER CORPORATION First Health w/WPS Statewide Auxiant for ILLING COMPANY INC First Health w/WPS Statewide Auxiant for MILE BLUFF MEDICAL CENTER First Health w/WPS Statewide Auxiant for NEUMAN POOLS INC First Health w/WPS Statewide Auxiant for OTTERY TRANSPORTATION INC First Health w/WPS Statewide Auxiant for PFERD, INC First Health w/WPS Statewide Auxiant for POLY VINYL COMPANY, INC First Health w/WPS Statewide Auxiant for PRICE COUNTY First Health w/WPS Statewide Auxiant for READER PRECISION SOLUTIONS INC First Health w/WPS Statewide Auxiant for T &W SUPERMARKET INC. First Health w/WPS Statewide Auxiant for TRIPLE CROWN PRODUCTS INC. First Health w/WPS Statewide Auxiant for VULCAN GLOBAL MANUFACTURING SOLUTIO First Health w/WPS Statewide Auxiant for WATERTRONICS LLC First Health w/WPS Statewide Auxiant for WESTOSHA CENTRAL HIGHSCHOOL DISTRIC First Health w/WPS Statewide for BOTANIC INNOVATIONS LLC First Health w/WPS Statewide for CABLECOM LLC First Health w/WPS Statewide for FELSS ROTAFORM LLC First Health w/WPS Statewide for MIDCON PRODUCTS INC First Health w/WPS Statewide for MTI CONNECT LLC First Health w/WPS Statewide for SCHAFFER SPECIALTY WELDING INC First Health w/WPS Statewide for STONECAST PRODUCTS INC First Health w/WPS Statewide for WATERS INDUSTRIAL SUPPLY INC First Health w/WPS Statewide for WILLOW CREEK PRESS INC First Health w/WPS Statewide for WPS Health Insurance Midlands Choice w/WPS Statewide & First Health Auxiant for CHAMBERS & OWEN Midlands Choice w/WPS Statewide & First Health for WPS Health Insurance Sagamore Plus w/WPS Statewide & First Health for WPS Health Insurance The Alliance Premier w/WPS Statewide & First Health Auxiant for CITIZENS COMMUNITY FEDERAL The Alliance Premier w/WPS Statewide & First Health Auxiant for PRICE COUNTY The Alliance Premier w/WPS Statewide & First Health Auxiant for ZIMBRICK INC The Alliance Premier w/WPS Statewide & Multiplan Auxiant for WISCONSIN PHYS SERVICE INS CORP The Alliance w/WPS Statewide & First Health Auxiant for BEST VERSION MEDIA, LLC The Alliance w/WPS Statewide & First Health Auxiant for CAPRI COMMUNITIES LLC The Alliance w/WPS Statewide & First Health Auxiant for CATALYST EXHIBITS INC The Alliance w/WPS Statewide & First Health Auxiant for CLASEN QUALITY CHOCOLATE INC. The Alliance w/WPS Statewide & First Health Auxiant for CODEWORKS, LLC The Alliance w/WPS Statewide & First Health Auxiant for COUSINS SUBMARINES INC The Alliance w/WPS Statewide & First Health Auxiant for DEWITT, LLP The Alliance w/WPS Statewide & First Health Auxiant for EASTCASTLE PLACE INC. The Alliance w/WPS Statewide & First Health Auxiant for EMPLOYER HEALTH CARE ALLIANCE COOPE The Alliance w/WPS Statewide & First Health Auxiant for ILLING COMPANY INC The Alliance w/WPS Statewide & First Health Auxiant for LINCOLN CONTRACTORS SUPPLY The Alliance w/WPS Statewide & First Health Auxiant for LOOS MACHINE & AUTOMATION The Alliance w/WPS Statewide & First Health Auxiant for METCALFE MARKETS The Alliance w/WPS Statewide & First Health Auxiant for NEUMAN POOLS INC The Alliance w/WPS Statewide & First Health Auxiant for NORTHERN METAL & ROOFING CO INC The Alliance w/WPS Statewide & First Health Auxiant for NORTHWEST COUNSELING AND GUIDANCE C The Alliance w/WPS Statewide & First Health Auxiant for PFERD, INC The Alliance w/WPS Statewide & First Health Auxiant for READER PRECISION SOLUTIONS INC The Alliance w/WPS Statewide & First Health Auxiant for SIXTEENTH ST COMM HEALTH CENTERS The Alliance w/WPS Statewide & First Health Auxiant for TRIPLE CROWN PRODUCTS INC. The Alliance w/WPS Statewide & First Health Auxiant for VULCAN GLOBAL MANUFACTURING SOLUTIO The Alliance w/WPS Statewide & First Health Auxiant for WATERTRONICS LLC The Alliance w/WPS Statewide & First Health Auxiant for WESTOSHA CENTRAL HIGHSCHOOL DISTRIC The Alliance w/WPS Statewide & First Health Auxiant for ZIMBRICK INC The Alliance w/WPS Statewide & First Health for OREGON LIVING AND REHABILITATION CENTER The Alliance w/WPS Statewide & First Health for WPS Health Insurance WAICU WPS Statewide w/First Health for WPS Health Insurance WPS Select Plus HMO w/First Health Auxiant for DAVID J FRANK LANDSCAPING WPS Select Plus HMO w/First Health for WPS Health Plan WPS Select Plus POS w/First Health for WPS Health Plan WPS Short Term Plan Statewide for WPS Health Insurance WPS Southern w/First Health for WPS Health Insurance WPS Statewide w/First Health & Cofinity for SNOWBELT HARDWOODS INCORPORATED WPS Statewide w/First Health & Cofinity for WPS Health Insurance WPS Statewide w/First Health Auxiant for BADGER UTILITY HOLDINGS LLC WPS Statewide w/First Health Auxiant for BAY-SAN COMPANY, INC. WPS Statewide w/First Health Auxiant for CHAMBERS & OWEN WPS Statewide w/First Health Auxiant for DAVID J FRANK LANDSCAPING WPS Statewide w/First Health Auxiant for DENTAL HEALTH PRODUCTS WPS Statewide w/First Health Auxiant for DON JACOBS MOTORS, INC. WPS Statewide w/First Health Auxiant for EL REY HOLDINGS LLC WPS Statewide w/First Health Auxiant for HOPPE TREE SERVICE, LLC WPS Statewide w/First Health Auxiant for MILE BLUFF MEDICAL CENTER WPS Statewide w/First Health Auxiant for OTTERY TRANSPORTATION INC WPS Statewide w/First Health Auxiant for PAGEL'S PONDEROSA DAIRY WPS Statewide w/First Health Auxiant for POLY VINYL COMPANY, INC WPS Statewide w/First Health Auxiant for PRICE COUNTY WPS Statewide w/First Health Auxiant for ROTE OIL LTD WPS Statewide w/First Health Auxiant for T &W SUPERMARKET INC. WPS Statewide w/First Health Auxiant for TOMSON'S OF APPLETON, INC WPS Statewide w/First Health for A F GELHAR COMPANY INC WPS Statewide w/First Health for ABSOLUTE CONCRETE LLC WPS Statewide w/First Health for AMERICAN FLEXPACK INC WPS Statewide w/First Health for BEST ENTERPRISES LLC WPS Statewide w/First Health for BOTANIC INNOVATIONS LLC WPS Statewide w/First Health for BRAUER AND BRAUER INC DBA FAST SIGNS WPS Statewide w/First Health for BUSHMANS INC WPS Statewide w/First Health for CABLECOM LLC WPS Statewide w/First Health for CENTRAL WISCONSIN FLEX INC WPS Statewide w/First Health for CHIPPEWA VALLEY EXCAVATING LLC WPS Statewide w/First Health for CONTRACT MANUFACTURING SERVICES LLC WPS Statewide w/First Health for COPPS INDUSTRIES INC WPS Statewide w/First Health for DARBOY STONE INC WPS Statewide w/First Health for DWYNNE R SUTHEIMER INC WPS Statewide w/First Health for E L M REPAIR AND REFRIGERATION INC WPS Statewide w/First Health for EARTH INC WPS Statewide w/First Health for EMH OF LARSEN INC WPS Statewide w/First Health for FELSS ROTAFORM LLC WPS Statewide w/First Health for FOX VALLEY PLASTIC SURGERY SC WPS Statewide w/First Health for GREAT NORTHERN INNOVATION WPS Statewide w/First Health for HARLEY DAVIDSON MOTORCYCLES OF APPLETON INC WPS Statewide w/First Health for LIBERTY TITLE AND ABSTRACT INC WPS Statewide w/First Health for MAHUTA TOOL CORP WPS Statewide w/First Health for METALS ENGINEERING INC WPS Statewide w/First Health for MEYERS ELECTRIC SERVICES INC WPS Statewide w/First Health for MIDCON PRODUCTS INC WPS Statewide w/First Health for MIDWEST AG AND COMMERCIAL CONTRACTORS LLC WPS Statewide w/First Health for MSM LTD WPS Statewide w/First Health for MTI CONNECT LLC WPS Statewide w/First Health for MUTUAL OF WAUSAU INSURANCE CORPORATION WPS Statewide w/First Health for MYRON SOIK AND SONS INC WPS Statewide w/First Health for NICOLET HARDWOODS CORPORATION WPS Statewide w/First Health for PETERSEN AUTOMOTIVE LLC WPS Statewide w/First Health for QUEST CIVIL ENGINEERS LLC WPS Statewide w/First Health for RAPCO FLEET SUPPORT INC WPS Statewide w/First Health for ROLLED THREADS UNLIMITED LLC WPS Statewide w/First Health for ROSEWOOD DAIRY INC WPS Statewide w/First Health for SCHAFFER SPECIALTY WELDING INC WPS Statewide w/First Health for SERVICES PLUS INC WPS Statewide w/First Health for SPORTS MEDICINE CENTER SC WPS Statewide w/First Health for STEVE FISCHER CONSTRUCTION WPS Statewide w/First Health for STONECAST PRODUCTS INC WPS Statewide w/First Health for SULLIVAN PRECISION PLATE LLC WPS Statewide w/First Health for TITAN INDUSTRIES INC WPS Statewide w/First Health for TOOLCRAFT MACHINING INC WPS Statewide w/First Health for TOTAL ELECTRIC SERVICE INC WPS Statewide w/First Health for TOWN OF MINOCQUA WPS Statewide w/First Health for VANKIN HOLDINGS INC DBA BULL FALLS HARLEY DAV WPS Statewide w/First Health for W HAUT SPECIALTY CO INC WPS Statewide w/First Health for WATERS INDUSTRIAL SUPPLY INC WPS Statewide w/First Health for WILLOW CREEK PRESS INC WPS Statewide w/First Health for WONDRA CONSTRUCTION INC WPS Statewide w/First Health for WPS Bronze $9450 Ded 100% Coins PPO WPS Statewide w/First Health for WPS Health Insurance My insurance plan isn't listed
- Remaining Deductible This Year $
More Information
Procedure information, stefan michael brettfeld, pricing disclaimer.
Wisconsin Physicians Service Insurance Corporation (WPS) and Turquoise Health are committed to helping patients make more informed decisions about their healthcare. This includes helping patients understand the cost of their care. Because every patient's needs are unique, we encourage you to contact the provider(s) directly for an accurate and personalized price estimate for your care. Again, this tool provides an estimate only .
In compliance with federal law, every hospital or other provider provides a list of standard charges. The list charge of a medical service is not equivalent to the actual amount paid by governmental or commercial insurance companies. WPS and Turquoise Health cannot guarantee that this rate is currently the cash rate the provider offers. The amount a patient pays is based on many factors, including health insurance, benefit plans and other applicable discounts, and the services provided based on each patient's unique needs.
Turquoise Health reviews charges quarterly to ensure the price listed matches the price listed on the provider's publicly-available website. However, please visit the provider's website or call the provider(s) directly for the latest, most accurate rate estimate.
The cash charge listed for hospitals includes hospital services only and may not contain professional fees for the physician providing the service.
A single charge may not represent a complete medical service; in general, multiple charge line items are necessary to represent all components of a service (e.g. procedure(s), supplies, and drugs).
This charge is not intended for media use and requires independent verification with the listed provider.
Please note: Customized estimates are available based on your specific benefit plan and cost-sharing by logging in to your customer portal through WPS . You may also obtain an estimate by contacting the WPS Customer Service number on your ID card. If you do not have your ID card available, you can find the applicable Customer Service number by visiting: https://www.wpshealth.com/contact/ .
Out-Of-Pocket Cost.
STEFAN MICHAEL BRETTFELD Rate
Remaining Deductible
Coinsurance
- Employer Resources
- NH Insurance Market Report
- Statewide Rates Report
- Health Costs
- Quality of Care
- Getting Health Insurance
- Managing your Cost
- Navigating the System
- Medical Providers
- Dental Providers
- Methodology for Health Costs for Consumers
- Methodology for Quality Metrics
- Connect With Us
Non-Emergency Transport, Basic Life Support
Non-emergency transport by ambulance for basic life support.
Related Procedures
Related procedures are health care services that often occur during the same day as this lead procedure.
- Emergency department visit for life threatening or functioning severity (99285)
- Complete blood cell count (red cells, white blood cell, platelets), automated test and automated differential white blood cell count (85025)
- Blood test, comprehensive group of blood chemicals (80053)
- Hospital discharge day management, more than 30 minutes (99239)
- Initial hospital inpatient care per day, typically 70 minutes (99223)
- Emergency department visit for problem of high severity (99284)
- Insertion of needle into vein for collection of blood sample (36415)
- Infectious agent detection by nucleic acid; severe acute respiratory syndrome coronavirus 2, amplified probe technique, making use of high throughput technologies as described by cms-2020-01-r (U0003)
- Amplifed dna or rna probe detection of severe acute respiratory syndrome coronavirus 2 (covid-19) antigen (87635)
- Testing for presence of drug, by chemistry analyzers (80307)
Cost Data Source
This website is for informational purposes only. NHID has made every effort to provide accurate information. Cost estimates for medical and dental procedures are based on typical payments and do not represent what your bill will be. Consult with your provider and insurer to get a personalized estimate.
NH HealthCost
- 2022 Small Group Comparison Tool
- Carrier Complaints
- Carrier Quality Measures
- Customizable Employee Toolkit
- Fully Insured (FI)
- Self-insured (SI)
- Complex Alternative Funding
- Carrier Networks & Product Offerings
- Compare Carrier Hospital Networks
- Independent Financial Ratings
- Provider Payment Reform & Value Based Payment Guide

IMAGES
VIDEO
COMMENTS
99282 - Emergency department visit for the evaluation and management of a patient, ... even if the condition has not changed and there is no short-term threat to life or function. ... especially in situations where the final diagnosis seems less than life-threatening. Per CPT: The final diagnosis for a condition does not, in and of itself ...
Presenting Problem (Severity) Self-limited or minor • Low to moderate • Moderate • High • High severity/immediate significant threat to life for physiological function ... CPT Code 99285: Emergency Department Visit \(A/B MAC Jurisdiction 15\) Author: CGS - CH Subject: A/B MAC J15
Every patient who visits the emergency department (ED) will go through triage, which allows the ED team to establish the severity of that person's condition. Triage takes into account the patient's vital signs, as well as his or her complaint. Dr. Oyler says measuring the patient's vital signs is the most crucial component of triage ...
Usually, the presenting problem(s) are of moderate severity. 99284 Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: A detailed history; A detailed examination; and Medical decision making of moderate complexity.
Highlights. In 2018, there were 143.5 million emergency department (ED) visits, representing 439 visits per 1,000 population. Fourteen percent of ED visits resulted in hospital admission (61 per 1,000 population). Circulatory and digestive system conditions were the most common reasons for these visits. The majority of ED visits (86 percent ...
Disclosing a new, life-threatening diagnosis to a patient is difficult for the physician, the patient, and the family. The disclosure provokes a wide range of reactions from both the patient and family, to which the emergency physician must respond. This interaction is further complicated by the limited time the emergency physician can spend with the patient, the strained resources of a busy ...
Emergency department visit for life-threatening or functioning severity; Emergency department visit for problem of high severity; Emergency department visit for problem of moderate severity; Critical care, first 30-74 minutes; Continuous remote monitoring of nervous system during operation, each hour. IDR Process Lags Behind Dispute Submission
Reducing avoidable emergency department (ED) visits is an important health system goal. This is a retrospective cohort study of the impact of a primary care intervention including an in-hospital, free, adult clinic for poor uninsured patients on ED visit rates and emergency severity at a nonprofit hospital.
1. INTRODUCTION. Hyperkalemia (HK) is a potentially life‐threatening disorder occurring in 1% to 10% of hospitalized and up to 2% to 3% of emergency department (ED) patients. 1 It occurs more commonly in patients with diabetes mellitus (DM), renal failure, chronic kidney disease (CKD), and heart failure (HF) 2, 3 due to renal impairment or medications that alter potassium excretion. 3, 4 ...
The severity of these symptoms and signs, along with the findings on functional lung assessment, are used to categorize asthma exacerbations as mild, moderate, severe, or life-threatening . The primary determinant of severity is percent predicted FEV 1 or PEF. The exacerbation severity determines treatment.
The Emergency Severity Index (ESI) Triage Algorithm. If you have any questions about the program you have just watched, you may call us at: (800) 424-4888 or fax (806) 743-2233. Direct your inquiries to Customer Service. Be sure to include the program number, title and speaker.
X-rays and CT scans may take 1-3 hours to be completed, depending on the number of patients who need these kinds of scans. Remember that people with life-threatening illness and injury may need them before you do. Sometimes it is necessary to consult with a specialty provider who doesn't normally work in the emergency department.
Background. Non-urgent Emergency Department (ED) visits are typically defined as visits for conditions for which a delay of several hours would not increase the likelihood of an adverse outcome. 1,2 Most studies find that at least 30% of all ED visits in the US are non-urgent, although select studies such as those using National Hospital Ambulatory Medical Survey data report lower percentages ...
A new study released today by the Centers for Disease Control and Prevention shows emergency department visits dropped by 23% for heart attacks, 20% for strokes and 10% for hyperglycemic crises in first 10 weeks after the COVID-19 public health emergency declaration.. The study's authors captured 73% of the nation's ED visits from the CDC's National Syndromic Surveillance Program and ...
Older patients are at high risk of unplanned revisits to the emergency department (ED) because of their medical complexity. To reduce the number of ED visits, we need more knowledge about the patient-level, environmental, and healthcare factors involved. The aim of this study was to describe older patients' perspectives and experiences before and after an ED visit, and to identify factors ...
not be present, depending on the severity of the exacerbation. The severity of these symptoms and signs, along with the findings on functional lung assessment, are used to catego-rize asthma exacerbations as mild, moderate, severe, or life-threatening (Table 2). The primary determinant of severity is percent predicted FEV 1 or PEF. The ...
Introduction Hyperkalemia is often managed in the emergency department (ED) and it is important to understand how ED management and post-discharge outcomes vary by hyperkalemia severity. This study was conducted to characterize ED management and post-discharge outcomes across hyperkalemia severities. Methods Adults with an ED visit with hyperkalemia (at least one serum potassium lab measure ...
Emergency department visit for problem of high severity (99284) Complete blood cell count (red cells, white blood cell, platelets), automated test and automated differential white blood cell count (85025) ... Emergency department visit for life threatening or functioning severity (99285) Injection, ketorolac tromethamine, per 15 mg (J1885)
Regarding the assessment of PEFR accuracy in the prediction of exacerbation severity among enrolled patients, PEFR after 1 h at cut-off point < 110 had 100% sensitivity and 62% specificity for the prediction of severe acute asthma with an overall accuracy of 82.9% and area under the curve was 0.81 (Tables 5 and 6); the predictors for severe exacerbation were old age, previous history of ...
The SINA expert panel recommends determining the PRAM score for asthmatic patients in the emergency department to categorize the risk of hospital admission [ 8, 16, 17 ]. •. Total score of 1-3: Low risk (<10%) of hospital admission. •. Total score of 4-7: Moderate risk (10-50%) of hospital admission. •.
CDC examined emergency department (ED) visits associated with heat-related illness (HRI) from the National Syndromic Surveillance Program and compared daily HRI ED visit rates during the warm-season months (May-September) of 2023 with those during 2018-2022. In the 2023 warm-season months, daily HRI ED visit rates peaked in several regions ...
Emergency department visit for problem of high severity (99284) Complete blood cell count (red cells, white blood cell, platelets), automated test and automated differential white blood cell count (85025) ... Emergency department visit for life threatening or functioning severity (99285) Injection, ketorolac tromethamine, per 15 mg (J1885)
Emergency department visit for life threatening or functioning severity Reported Price For STEFAN MICHAEL BRETTFELD Plan: This is the price that STEFAN MICHAEL BRETTFELD has reported for Emergency department visit for life threatening or functioning severity. We have added your insurance plan information to estimate your out-of-pocket cost.
Emergency department visit for life threatening or functioning severity (99285) Complete blood cell count (red cells, white blood cell, platelets), automated test and automated differential white blood cell count (85025) Blood test, comprehensive group of blood chemicals (80053) Hospital discharge day management, more than 30 minutes (99239)