We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Wandering Atrial Pacemaker
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Key features, clinical presentation, diagnostic evaluation, ongoing management.
- Full Chapter
- Supplementary Content
ESSENTIALS OF DIAGNOSIS
Progressive cyclic variation in P-wave morphology
Heart rate 60–100 bpm
Variation of P-wave morphology, P-P interval, and P-R interval
GENERAL CONSIDERATIONS
This rhythm is benign
This rhythm and multifocal atrial tachycardia are similar except for heart rate
The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity
Usually, it is associated with underlying lung disease
In the elderly, it may be a manifestation of sick sinus syndrome
In the young and athletic heart, it may represent enhanced vagal tone
SYMPTOMS AND SIGNS
Usually causes no symptoms and is incidentally discovered
Occasional patient may feel skipped beats
PHYSICAL EXAM FINDINGS
Variable S 1
DIFFERENTIAL DIAGNOSIS
Multifocal atrial tachycardia (heart rate > 100 bpm)
Frequent premature atrial complexes and atrial bigeminy
LABORATORY TESTS
None specific
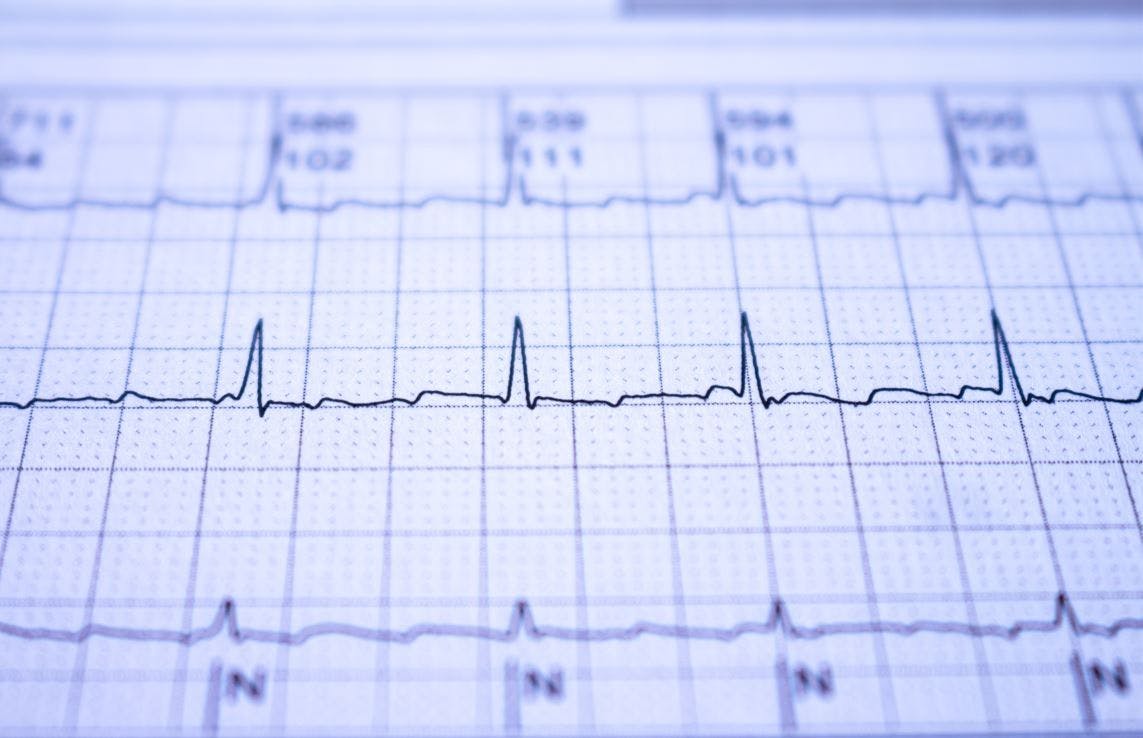
ELECTROCARDIOGRAPHY
ECG to document rhythm
CARDIOLOGY REFERRAL
Not required
MEDICATIONS
No specific treatment
Monitor and treat the underlying cause, such as sick sinus syndrome or lung disease
DIET AND ACTIVITY
No restrictions
General healthy lifestyle
Once a year if sinus node abnormality is suspected; otherwise when symptoms arise
COMPLICATIONS
May progress to sick sinus syndrome
This condition by itself is benign
PRACTICE GUIDELINES
Indications for pacemaker:
– If part of sick sinus syndrome
– If associated with documented symptomatic bradycardia
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

Thursday, March 4, 2021
Blog #200 — wandering pacemaker (vs mat).
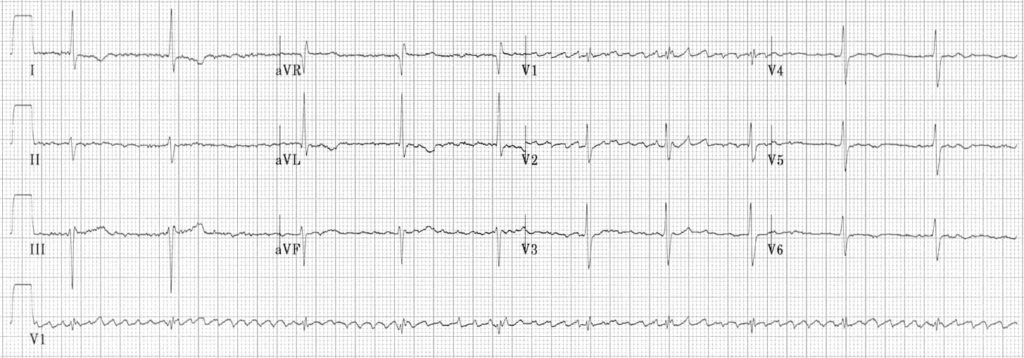
There is no clinical information is available for the ECG and 2-lead rhythm strip shown below in Figure-1 .
- HOW would you interpret this tracing?
- What treatment is likely to be needed?
====================================
Editorial Comment:
It is always challenging to interpret tracings without the benefit of clinical information. That said — this situation is common in clinical practice. My experience in this area derives from the 30 years during which I was charged with interpreting all ECGs ordered by 35 medical providers at a primary care clinic — as well periodic stints during which I interpreted hospital tracings without the benefit of any history.
- The challenge lies with having to decide which tracings in the “pile of ECGs to be interpreted” were those for which I needed to pull the medical chart ( or call the provider ) because of ECG findings of immediate potential concern.
- Obvious time constraints made it impossible to pull the chart for each ECG that I was given to read ( I’d never get anything else done if I did so ).
- I therefore became well versed in the skill of limiting the charts that I would pull to those patients whose ECGs showed findings I thought were important and potentially indicative of an acute situation that may have been overlooked.
=====================================
MY Thoughts on the ECG in Figure-1:
As always — systematic interpretation of any ECG should begin with assessing the cardiac rhythm. In general — lead II and lead V1 are the 2 best leads on a 12-lead tracing for assessing atrial activity — and we have the advantage in Figure-1 of a simultaneously-recorded 2-lead rhythm strip of both of these leads. By the Ps , Qs and 3R Approach:
- The rhythm in Figure-1 is clearly irregular .
- The QRS complex is narrow ( ie, not more than half a large box in duration = ≤0.10 second ) .
- The rate varies from 50 /minute — to just under 100 /minute.
- More than 1 P wave morphology is present . That said — P waves do appear to be related to neighboring QRS complexes, because the PR interval for the P wave shapes that we see remains constant ( See Figure-2 ) .
MY Thoughts on Figure-2:
There are 2 different P wave shapes in Figure-2 .
- The tracing begins with 3 sinus beats ( ie, RED arrows highlight 3 similar-looking upright-in-lead-II P waves — all with the same PR interval ) .
- P wave shape then changes for beats #4, 5 and 6 ( ie, BLUE arrows highlighting an almost isoelectric, if not negative P wave with fixed PR interval ) .
- The atrial focus then shifts back , with return to sinus P waves for beats #7, 8, 9 and 10 (ie, return of RED arrows highlighting similar-looking, upright P waves in lead II — albeit with variability in the R-R interval ).
- The rhythm in Figure-2 concludes with a slowing-down of the ventricular rate, as the 2nd atrial focus returns , in which the P wave is almost isoelectric (ie, BLUE arrows for beats #11 and 12 ).
BOTTOM LINE regarding Figure-1: The rhythm in Figure-2 is most consistent with a Wandering Atrial Pacemaker . This is because the change from one atrial site to the next occurs gradually over a period of several beats.
- PEARL: The reason it is uncommon ( if not rare ) in clinical practice to see a wandering atrial pacemaker — is that most providers do not pay long enough attention to beat-to-beat change in P wave morphology needed to identify gradual shift between at least 3 different atrial sites.
SUMMARY: Review of the KEY features of wandering atrial pacemaker is the theme below for our ECG Media Pearl #17 ( a 3:30 minute audio recording ).
- Written review of wandering pacemaker appears below in Figure-3 .
- Review of MAT is covered in our ECG Blog #199 .

Today’s E CG M edia P EARL # 17 ( 3:30 minutes Audio ) — What is a Wandering Atrial Pacemaker ( as opposed to MAT )?
A DDENDUM ( 3/4/2021 ) :
I received the following note from David Richley regarding today’s tracing: “I think I would use different terminology to describe this because to me the atrial pacemaker doesn’t so much ‘wander’ as ‘jump’. I would describe this as sinus arrhythmia with junctional escape rhythm at 60-65/minute every time the sinus node discharge rate slows to below that rate. I interpret the escape beats as junctional rather than atrial, because athough the P waves, ( which are initially negative in II, aVF and V4-V6 — and positive in aVR ) precede the QRS — the PR segment is very short, suggesting an AV nodal origin. However, we describe this phenomenon — I do agree that it’s likely to be completely benign.
MY Thoughts: Dave’s comment is one of the reasons why: i ) The diagnosis of wandering pacemaker requires clear demonstration of shift in the atrial pacemaker in at least 3 different sites. We only see 2 different sites here; and , ii ) The diagnosis of wandering atrial pacemaker is not common.
- It’s impossible to rule out Dave’s theory from the single tracing we have.
- That said — the BLUE arrow P wave site may or may not be of AV nodal origin ( you can see a similar, near-isoelectric P wave with short PR interval from a low atrial site ).
- I also considered the possibility of the BLUE arrow P waves representing junctional escape — but decided against it because the difference in R-R interval from what we see between beats #9-10 vs what we see between beats #10-11 is more than what I’d expect based on the cadence of rate variation I see from beats #7-10.
- Bottom Line: We both agree there is a shift in the pacemaker site in a rhythm that is likely to be benign. And, we both agree that additional monitoring would be needed for a definitive response. THANK YOU Dave!
No comments:
Post a comment.
Ectopic Supraventricular Arrhythmias
Various rhythms result from supraventricular foci (usually in the atria). Diagnosis is by electrocardiography. Many are asymptomatic and require no treatment.
(See also Overview of Arrhythmias .)
Ectopic supraventricular rhythms include
Atrial premature beats
Atrial tachycardia, multifocal atrial tachycardia, nonparoxysmal junctional tachycardia, wandering atrial pacemaker.
Atrial premature beats (APB), or premature atrial contractions (PAC), are common episodic impulses. They may occur in normal hearts with or without precipitating factors (eg, coffee, tea, alcohol, pseudoephedrine ) or may be a sign of a cardiopulmonary disorder. They are common in patients with chronic obstructive pulmonary disease (COPD). They occasionally cause palpitations.
Diagnosis is by electrocardiography (ECG—see figure Atrial premature beat ).
Atrial premature beat (APB)
Image courtesy of L. Brent Mitchell, MD.
APBs may be normally, aberrantly, or not conducted and are usually followed by a noncompensatory pause. Aberrantly conducted APBs (usually with right bundle branch block morphology) must be distinguished from premature beats of ventricular origin.
Atrial escape beats are ectopic atrial beats that emerge after long sinus pauses or sinus arrest. They may be single or multiple; escape beats from a single focus may produce a continuous rhythm (called ectopic atrial rhythm). Heart rate is typically slower, P wave morphology is typically different, and PR interval is slightly shorter than in sinus rhythm.
Atrial tachycardia is a regular rhythm caused by the consistent, rapid atrial activation from a single atrial focus. Heart rate is usually 150 to 200 beats/minute; however, with a very rapid atrial rate, nodal dysfunction, and/or digitalis toxicity, atrioventricular (AV) block may be present, and ventricular rate may be slower. Mechanisms include enhanced atrial automaticity and intra-atrial reentry.
Atrial tachycardia is the least common form (5%) of paroxysmal supraventricular tachycardia and usually occurs in patients with a structural heart disorder. Other causes include atrial irritation (eg, pericarditis
Symptoms are those of other tachycardias (eg, light-headedness, dizziness, palpitations, and rarely syncope).
Diagnosis is by electrocardiography (ECG); P waves, which differ in morphology from normal sinus P waves, precede QRS complexes but may be hidden within the preceding T wave (see figure True atrial tachycardia ).
True atrial tachycardia
Vagal maneuvers may be used to slow the heart rate, allowing visualization of P waves when they are hidden, but these maneuvers do not usually terminate the arrhythmia (demonstrating that the AV node is not an obligate part of the arrhythmia circuit).
Treatment involves managing causes and slowing ventricular response rate using a beta-blocker or calcium channel blocker. An episode may be terminated by direct current cardioversion . Pharmacologic approaches to termination and prevention of atrial tachycardia include antiarrhythmic drugs in class Ia, Ic, or III. If these noninvasive measures are ineffective, alternatives include overdrive pacing and ablation .
Multifocal atrial tachycardia (chaotic atrial tachycardia) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is > 100 beats/minute. On ECG, P-wave morphology differs from beat to beat, and there are ≥ 3 distinct P-wave morphologies. The presence of P waves distinguishes multifocal atrial tachycardia from atrial fibrillation . Except for the rate, features are the same as those of wandering atrial pacemaker. Symptoms, when they occur, are those of rapid tachycardia. Multifocal atrial tachycardia can be due to an underlying pulmonary disorder such as chronic obstructive pulmonary disease coronary artery disease , and electrolyte abnormalities such as hypokalemia . Treatment is directed at the underlying disorder.
Nonparoxysmal junctional tachycardia is caused by abnormal automaticity in the AV node or adjacent tissue, which typically follows open heart surgery, acute inferior myocardial infarction, myocarditis, or digitalis toxicity. Heart rate is 60 to 120 beats/minute; thus, symptoms are usually absent. ECG shows regular, normal-appearing QRS complexes without identifiable P waves or with retrograde P waves (inverted in the inferior leads) that occur shortly before ( < 0.1 second) or after the QRS complex. The rhythm is distinguished from paroxysmal supraventricular tachycardia by the lower heart rate and gradual onset and offset. Treatment is directed at causes.
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

- Mobile Apps
- Journal Club
- Antibiotics
- Quick Critical Care
- Residency Directory
- Recent Changes
- About WikEM
- Getting Started
- Creating & Editing
- Needed Pages
- Editorial Levels
- Contribution Score
- Elective Guide
- Citing WikEM
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Browse properties

- View source
- View history
- Create account

We need you! See something you could improve? Make an edit and help make WikEM better for everyone.
- Wandering atrial pacemaker
- 2 Clinical Features
- 3.1 Palpitations
- 4.2 Diagnosis
- 5 Management
- 6 Disposition
- 8 External Links
- 9 References
- Three or more ectopic foci within the atrial myocardium serve as the pacemaker
- Rate is less than 100bpm (in contrast to MAT )
- Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia
- Intrinsic cardiac or pulmonary disease
- Metabolic derangements
- Drug toxicity (including Digoxin )
Clinical Features
- Often seen in the extremes of age and in athletes
- Rarely causes symptoms
Differential Diagnosis
Palpitations.
- Narrow-complex tachycardias
- Wide-complex tachycardias
- Second Degree AV Block Type I (Wenckeback)
- Second Degree AV Block Type II
- Third Degree AV Block
- Premature atrial contraction
- Premature junctional contraction
- Premature ventricular contraction
- Sick sinus syndrome
- Acute coronary syndrome
- Cardiomyopathy
- Congenital heart disease
- Congestive heart failure (CHF)
- Mitral valve prolapse
- Pacemaker complication
- Pericarditis
- Myocarditis
- Valvular disease
- Panic attack
- Somatic Symptom Disorder
- Drugs of abuse (e.g. cocaine )
- Medications (e.g. digoxin , theophylline )
- Thyroid storm
- Pulmonary embolism
- Dehydration
- Pheochromocytoma

- ECG should show three distinct P wave morphologies with a ventricular rate <100bpm
- Rarely requires treatment
Disposition
- Outpatient management
- Multifocal atrial tachycardia
- Dysrhythmia
External Links
- Richard Cunningham
- fardis tavangary
- Ross Donaldson
- Privacy policy
- Disclaimers

Junctional Escape Rhythm
- Ed Burns and Robert Buttner
- Jul 19, 2021
ECG features of Junctional Escape Rhythm
- Junctional rhythm with a rate of 40-60 bpm
- QRS complexes are typically narrow (< 120 ms)
- No relationship between the QRS complexes and any preceding atrial activity (e.g. P-waves, flutter waves, fibrillatory waves)
Pacemaker cells are found at various sites throughout the conducting system, with each site capable of independently sustaining the heart rhythm. The rate of spontaneous depolarisation of pacemaker cells decreases down the conducting system:
- SA node (60-100 bpm)
- Atria (< 60 bpm)
- AV node (40-60 bpm)
- Ventricles (20-40 bpm)
Under normal conditions, subsidiary pacemakers are suppressed by the more rapid impulses from above (i.e. sinus rhythm). Junctional and ventricular escape rhythms arise when the rate of supraventricular impulses arriving at the AV node or ventricle is less than the intrinsic rate of the ectopic pacemaker.
Conditions leading to the emergence of a junctional or ventricular escape rhythm include:
- Severe sinus bradycardia
- Sinus arrest
- Sino-atrial exit block
- High-grade second degree AV block
- Third degree AV block
- Hyperkalaemia
- Drugs: beta-blocker, calcium-channel blocker or digoxin poisoning
ECG Examples
Atrial fibrillation with 3rd degree AV block and a junctional escape rhythm (“regularised AF”)
- Coarse atrial fibrillation (irregular baseline with atrial complexes at rate > 400 bpm)
- Regular narrow complex rhythm at 60 bpm
- The combination of atrial fibrillation with a regular rhythm (“regularised AF”) indicates that none of the atrial impulses are conducted to the ventricles, i.e. complete heart block is present
- The narrow complex rhythm is therefore a junctional escape rhythm
- Regularised AF is characteristically seen as a consequence of digoxin toxicity
Terminology of junctional rhythms
- Junctional bradycardia = junctional rhythm at a rate of < 40 bpm
- Junctional escape rhythm = junctional rhythm at a rate of 40-60 bpm
- Accelerated junctional rhythm = junctional rhythm at 60-100 bpm
- Junctional tachycardia = junctional rhythm at > 100 bpm
Related Topics
- Ventricular escape rhythm
Advanced Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course : Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop . Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog .
- Zimmerman FH. ECG Core Curriculum . 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations , 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine . 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care . 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG . 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Robert Buttner
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library . Twitter: @rob_buttner
I dont agree with the first example as atrial fibrillation Its more like atrial flutter with variable block
I’m confident it’s AF. I see the point, but you’d expect each flutter wave in atrial flutter to circle around the same macrore-entry circuit (e.g. tricuspid annulus). Therefore, flutter waves with (almost) always have identical morphology. It’s different here, so has to be coarse AF.
No fluther waves in II, III, Avf. That is more likely coarse a fib.
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
Wandering Atrial Pacemaker EKG Interpretation with Rhythm Strip
Ekg features, wandering atrial pacemaker ekg interpretation example.
This website is only for professional medical education. Contact your doctor for medical care. 2024 © MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us
Wandering Atrial Pacemaker ECG Interpretation with Sample Strip
Wandering atrial pacemaker rhythm strip features, authors and reviewers.
- ECG heart rhythm modules: Thomas O'Brien.
- ECG monitor simulation developer: Steve Collmann
- 12 Lead Course: Dr. Michael Mazzini, MD .
- Spanish language ECG: Breena R. Taira, MD, MPH
- Medical review: Dr. Jonathan Keroes, MD
- Medical review: Dr. Pedro Azevedo, MD, Cardiology
- Last Update: 11/8/2021
- Electrocardiography for Healthcare Professionals, 6th Edition Kathryn Booth and Thomas O'Brien ISBN10: 1265013470, ISBN13: 9781265013479 McGraw Hill, 2023
- Rapid Interpretation of EKG's, Sixth Edition Dale Dublin Cover Publishing Company
- EKG Reference Guide EKG.Academy
- 12 Lead EKG for Nurses: Simple Steps to Interpret Rhythms, Arrhythmias, Blocks, Hypertrophy, Infarcts, & Cardiac Drugs Aaron Reed Create Space Independent Publishing
- Heart Sounds and Murmurs: A Practical Guide with Audio CD-ROM 3rd Edition Elsevier-Health Sciences Division Barbara A. Erickson, PhD, RN, CCRN
- The Virtual Cardiac Patient: A Multimedia Guide to Heart Sounds, Murmurs, EKG Jonathan Keroes, David Lieberman Publisher: Lippincott Williams & Wilkin) ISBN-10: 0781784425; ISBN-13: 978-0781784429
- Project Semilla, UCLA Emergency Medicine, EKG Training Breena R. Taira, MD, MPH
- ECG Reference Guide PracticalClinicalSkills.com
This website provides professional medical education. For medical care contact your doctor. 2024 ©MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us | 1
Ectopic Supraventricular Arrhythmias
Various rhythms result from supraventricular foci (usually in the atria). Diagnosis is by electrocardiography. Many are asymptomatic and require no treatment.
(See also Overview of Arrhythmias .)
Ectopic supraventricular rhythms include
Atrial premature beats
Atrial tachycardia, multifocal atrial tachycardia, nonparoxysmal junctional tachycardia, wandering atrial pacemaker.
Atrial premature beats (APB), or premature atrial contractions (PAC), are common episodic impulses. They may occur in normal hearts with or without precipitating factors (eg, coffee, tea, alcohol, pseudoephedrine ) or may be a sign of a cardiopulmonary disorder. They are common in patients with chronic obstructive pulmonary disease (COPD). They occasionally cause palpitations.
Diagnosis is by electrocardiography (ECG—see figure Atrial premature beat ).
Atrial premature beat (APB)
Image courtesy of L. Brent Mitchell, MD.
APBs may be normally, aberrantly, or not conducted and are usually followed by a noncompensatory pause. Aberrantly conducted APBs (usually with right bundle branch block morphology) must be distinguished from premature beats of ventricular origin.
Atrial escape beats are ectopic atrial beats that emerge after long sinus pauses or sinus arrest. They may be single or multiple; escape beats from a single focus may produce a continuous rhythm (called ectopic atrial rhythm). Heart rate is typically slower, P wave morphology is typically different, and PR interval is slightly shorter than in sinus rhythm.
Atrial tachycardia is a regular rhythm caused by the consistent, rapid atrial activation from a single atrial focus. Heart rate is usually 150 to 200 beats/minute; however, with a very rapid atrial rate, nodal dysfunction, and/or digitalis toxicity, atrioventricular (AV) block may be present, and ventricular rate may be slower. Mechanisms include enhanced atrial automaticity and intra-atrial reentry.
Atrial tachycardia is the least common form (5%) of paroxysmal supraventricular tachycardia and usually occurs in patients with a structural heart disorder. Other causes include atrial irritation (eg, pericarditis
Symptoms are those of other tachycardias (eg, light-headedness, dizziness, palpitations, and rarely syncope).
Diagnosis is by electrocardiography (ECG); P waves, which differ in morphology from normal sinus P waves, precede QRS complexes but may be hidden within the preceding T wave (see figure True atrial tachycardia ).
True atrial tachycardia
Vagal maneuvers may be used to slow the heart rate, allowing visualization of P waves when they are hidden, but these maneuvers do not usually terminate the arrhythmia (demonstrating that the AV node is not an obligate part of the arrhythmia circuit).
Treatment involves managing causes and slowing ventricular response rate using a beta-blocker or calcium channel blocker. An episode may be terminated by direct current cardioversion . Pharmacologic approaches to termination and prevention of atrial tachycardia include antiarrhythmic drugs in class Ia, Ic, or III. If these noninvasive measures are ineffective, alternatives include overdrive pacing and ablation .
Multifocal atrial tachycardia (chaotic atrial tachycardia) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is > 100 beats/minute. On ECG, P-wave morphology differs from beat to beat, and there are ≥ 3 distinct P-wave morphologies. The presence of P waves distinguishes multifocal atrial tachycardia from atrial fibrillation . Except for the rate, features are the same as those of wandering atrial pacemaker. Symptoms, when they occur, are those of rapid tachycardia. Multifocal atrial tachycardia can be due to an underlying pulmonary disorder such as chronic obstructive pulmonary disease coronary artery disease , and electrolyte abnormalities such as hypokalemia . Treatment is directed at the underlying disorder.
Nonparoxysmal junctional tachycardia is caused by abnormal automaticity in the AV node or adjacent tissue, which typically follows open heart surgery, acute inferior myocardial infarction, myocarditis, or digitalis toxicity. Heart rate is 60 to 120 beats/minute; thus, symptoms are usually absent. ECG shows regular, normal-appearing QRS complexes without identifiable P waves or with retrograde P waves (inverted in the inferior leads) that occur shortly before ( < 0.1 second) or after the QRS complex. The rhythm is distinguished from paroxysmal supraventricular tachycardia by the lower heart rate and gradual onset and offset. Treatment is directed at causes.
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Neonatal and Pediatric Arrhythmias: Clinical and Electrocardiographic Aspects
Affiliations.
- 1 Paediatric Cardiology and Cardiac Arrhythmias Unit, Department of Paediatric Cardiology and Cardiac Surgery, Bambino Gesù Children's Hospital and Research Institute, Piazza Sant'Onofrio 4, Rome 00165, Italy. Electronic address: [email protected].
- 2 Paediatric Cardiology and Cardiac Arrhythmias Unit, Department of Paediatric Cardiology and Cardiac Surgery, Bambino Gesù Children's Hospital and Research Institute, Piazza Sant'Onofrio 4, Rome 00165, Italy.
- PMID: 29784491
- DOI: 10.1016/j.ccep.2018.02.008
Arrhythmias have acquired a specific identity in pediatric cardiology, but for pediatric cardiologists it has always been difficult to recognize and treat them. Changes in anatomy and physiology result in electrocardiogram features that differ from the normal adult pattern and vary according to the age of the child. Sinus arrhythmia, ectopic atrial rhythm, "wandering pacemaker," and junctional rhythm can be normal characteristics in children (15%-25% of healthy children can have these rhythms on the electrocardiogram). Tachyarrhythmias and bradyarrhythmias must be treated according to the severity of symptoms, and the patient's age and weight.
Keywords: Arrhythmias; Bradycardia; Children; ECG; Neonates; Pediatric arrhythmias; Tachycardia.
Copyright © 2018 Elsevier Inc. All rights reserved.
Publication types
- Arrhythmias, Cardiac / diagnosis*
- Arrhythmias, Cardiac / physiopathology
- Diagnosis, Differential
- Electrocardiography / methods*
- Heart Rate / physiology*
- Infant, Newborn
- Sinus Rhythm
Sinus Arrhythmia
Qrs complex, bradycardia.
- Causes of bradycardia
- Causes with narrow QRS
- Causes with wide QRS
Tachycardia
- Tachycardia Types
- Tachycardia with Narrow QRS
- Tachycardia with wide QRS
- Mechanism of formation of tachycardia
- Anatomical Malformations
Supraventricular Tachycardia (SVT)
- Characteristics
- Supraventricular Tachycardia
Atrial Flutter
Atrial fibrillation, ventricular tachycardia.
- Electrophysiological (EP)
Why is it required?
- Radiofrequency Ablation
- TBM With Hyperthermia
- A 12 Yrs Old Boy Came With Complaint That When E...
- 6 Years Boy With Attacks Of Sense Ff Drowsiness Fo...
Arrhythmias
Sinus rhythm:.
Definition: Irregular rhythm originating in the sinus node.
(P-P interval varies >0.08 sec)
Arrhythmia With Normal Heart Rate
They are seen in the following conditions:
Arrhythmia with narrow QRS,
- Accelerated junctional rhythm
Arrhythmia with wide QRS
- Accelerated junctional rhythm with aberrancy
Consider the following when looking at the QRS complex
- Association of P-waves to QRS
Narrow QRS : Infant <80 msec, Child <85 msec. It is generally supraventricular in origin. Generally requires activation through bundle of His
Wide QRS : It is often of ventricular origin. Also seen with Aberrant conduction (Rate-related versus present in sinus). There may be the presence of an accessory connection. Associated with drug effects. Seen with electrolyte imbalance.
Wide QRS of Ventricular origin : The following is supportive of ventricular origin:
- AV dissociation
Wide QRS of Aberrancy
Fixed bundle branch block
Rate-related
- Usually refractory period of right bundle is more than left bundle
Wide QRS of Accessory connection
- May be present intermittently in sinus rhythm
Wide QRS of Drug effects
- Tricyclic antidepressants
Wide QRS of Electrolytes
- Hypoxia and acidosis
It is calculated from the lowest heart rate for 6 sec in normal individuals. It is defined as less than
- 26 BPM in Adolescent
Causes of bradycardia:
Causes of bradycardia with narrow qrs:.
- Junctional escape (40-60 BPM)
Causes of Bradycardia with wide QRS:
- Escape above bifurcation of His with aberrancy
Definition: Three successive beats faster than normal for age.
- Ventricular tachycardia
Tachycardia with Narrow QRS:
- Junctional tachycardia
Tachycardia with wide QRS:
- Ventricular Fibrillation
Mechanism of formation of tachycardia:
Disorders of impulse formation
Disorders of impulse propagation
Abnormal Automaticity
Anatomical Malformations causing reentry:
Figure 1: Mechanism for re-entry
Definition:
Characteristics in children.
- BPM usually around 300
Mechanisms of Supraventricular Tachycardia:
Probable Re-entrant Mechanism
- Atrial muscle re-entry
Presence of Bypass Tracts
- Dual AV nodal pathways
Probable Abnormal Automaticity
- Junctional ectopic tachycardia
Characteristics:
- May be modified by drugs
- If WPW, may have variable QRS morphology
- Change in morphology of QRS (particularly if abnormal in sinus)
Electrophysiological (EP) Study
- Ablation of the origin of critical structures
Arrhythmias - Treatment
Depends on mechanism
- For Both: eliminate the source (radiofrequency ablation or surgery)
Radiofrequency Ablation:
- Observe effects
It causes a thermal burn. Tip temperature is approximately 70 degree Celsius
Applications:
It is used in the treatment of
- Procedure maybe excision or cryosurgery
Contributor Information and Disclosures
Partner Sites
Infection in Children - Part 3
- Kids Corner
- Diagnostic Aid
- Ask a Doctor
- Diagnostic Dilemma
- Question of the Week
- Pediatric Blogs
- Spot Diagnosis
- Grand Rounds
- Current Issue
- Advance Access
- About the Journal
- Submit Article
- Pediatric Oncall
- Medical Calculators
- Vaccine Reminder
- Pediatric Oncall Journal
- Drug Center
- Upcoming Conferences
- Conference Abstracts

- Heart Failure
- Cardiovascular Clinical Consult
- Adult Immunization
- Hepatic Disease
- Rare Disorders
- Pediatric Immunization
- Implementing The Topcon Ocular Telehealth Platform
- Weight Management
- Men's Health
- Women's Health
- Substance Use
- Kidney Disease
- Complimentary & Alternative Medicine
- Dermatology
- Endocrinology
- Oral Medicine
- Otorhinolaryngologic Diseases
- Gastrointestinal Disorders
- Musculoskeletal Disorders
- Rheumatology
- Pulmonology
Normal Sinus Rhythm With Junctional Escape Beats: ECG Findings
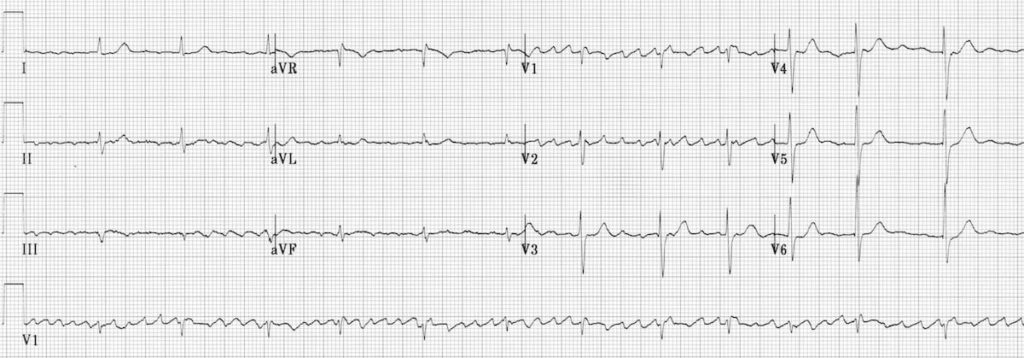
- William J. Brady, MD
- Theodore Chan, MD
A 68-year-old woman with hypertension complains of intermittent dyspnea and light-headedness. She is asymptomatic during the evaluation. Vital signs are normal, but an irregularly irregular pulse is noted on examination as well as on the telemetry monitor. The 12-lead ECG is shown here; the ECG machine printout reads "atrial fibrillation." The patient has no history of this arrhythmia.

Atrial Fibrillation May be More Common in Younger Adults than Previously Thought: Daily Dose
Your daily dose of the clinical news you may have missed.

Navigating Cardiovascular Complications of Obesity: Expert Insights for Primary Care
Listen to our latest podcast episode for details on top CVD risk factors to screen patients with obesity for, medications to help prevent CVD, and more.
New Data Suggest Atrial Fibrillation May be More Common in Younger Adults than Previously Thought
Patients with AF aged younger than 65 years have substantial comorbidity burden that may impact their future risk of mortality, reported researchers.

Primary Viewpoints Episode 4: Lp(a): The Next CVD Target?
Patrick Moriarty, MD, from the University of Kansas Medical Center, discusses the role of Lp(a) as a risk factor for cardiovascular disease and the phase 3 trials of a potential treatment.
New Research Suggests Cardiac Events are Prevalent in Older Adults Hospitalized with RSV
Nearly one-quarter of hospitalized adults aged 50 years and older with RSV experienced an acute cardiac event, according to results of a new study.

Individuals with CVD Consume More Daily Sodium than Recommended, According to New Data
ACC.24: Adults with a history of CVD consumed more than double the recommended daily sodium amount, reported researchers.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

COMMENTS
Wandering Atrial Pacemaker (WAP) is a cardiac rhythm disorder that causes irregular and variable heartbeats. Learn the Heart - Healio provides a comprehensive ECG review of this condition ...
This results in at least three different P wave morphologies, and often the PR interval may vary due to this. If the heart rate is less than 100 BPM we call this a wandering atrial pacemaker, or WAP. If it's greater than 100 BPM we call it a multifocal atrial tachycardia, or MAT for short.
Wandering atrial pacemaker (WAP) is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. This is different from normal pacemaking activity, where the sinoatrial node (SA node) is responsible for each heartbeat and keeps a steady rate and rhythm. Causes of wandering atrial pacemaker are unclear, but there may be factors leading to its ...
A wandering atrial pacemaker is a rare form of a condition called arrhythmia. That's a problem with your heartbeat. It can happen anytime, even when you're sleeping. It's usually nothing to ...
A junctional rhythm is a heart rhythm problem that can make your heartbeat too slow or too fast. If you have a junctional rhythm, you may not have any symptoms. But sometimes, this condition can make you feel faint, weak or out of breath. If symptoms interfere with your daily life, your provider may recommend treatment to regulate your heartbeat.
This rhythm and multifocal atrial tachycardia are similar except for heart rate. The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity. Usually, it is associated with underlying lung disease. In the elderly, it may be a manifestation of sick sinus syndrome.
Technically, for a rhythm to be classified as a wandering pacemaker — there should be gradual shift between at least 3 different atrial sites.Since we only see 2 different atrial sites (highlighted by RED and BLUE arrows) in Figure-2 — we would need a longer period of monitoring to prove this rhythm is a wandering pacemaker.That said — wandering pacemaker is the most logical explanation ...
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.
Wandering atrial pacemaker. Non-arrhythmic cardiac causes: Acute coronary syndrome. Cardiomyopathy. Congenital heart disease. Congestive heart failure (CHF) Mitral valve prolapse. Pacemaker complication. Pericarditis.
Whereas atrial tachycardia is due to a single ectopic focus in the atrium, wandering atrial pacemaker and MAT are due to multiple microreentry foci in the atrium. If the ventricular rate is less than 100 bpm, it is considered a wandering atrial pacemaker; if the ventricular rate is greater than 100 bpm, it is considered MAT.
ECG features of Junctional Escape Rhythm. Junctional rhythm with a rate of 40-60 bpm. QRS complexes are typically narrow (< 120 ms) No relationship between the QRS complexes and any preceding atrial activity (e.g. P-waves, flutter waves, fibrillatory waves) Mechanism. Pacemaker cells are found at various sites throughout the conducting system ...
The atrioventricular node is a separate cardiac pacemaker located in the inferior-posterior right atrium. The His bundle is a separate cardiac pacemaker located at the inferior end of the atria and ventricle. A junctional rhythm is an abnormal heart rhythm that originates from the AV node or His bundle. This activity reviews the evaluation and ...
The management of patients with atrial fibrillation and an abnormally fast ventricular response has been through the use of pharmacologic agents. In those cases where rate control cannot be achieved pharmacologically, a standard approach has been atrioventricular (AV) junctional ablation and ventricular pacemaker implantation to achieve a stable ventricular rate. Long-term ventricular pacing ...
This article is a guide for interpreting abnormal Wandering Atrial Pacemaker EKGs, including qualifying criteria and a sample EKG rhythnm strip. Wandering atrial pacemaker is an arrhythmia originating in shifting pacemaker sites from the SA node to the atria and back to the SA node. On an ECG, the p-waves reflect the pacemaker shifts by shape variations. The PRI interval may vary from one beat ...
Wandering atrial pacemaker (WAP) ( Fig. 3.12) is an atrial rhythm with multiple P-wave morphologies (three or more), often occurring in a repetitive pattern at a rate of less than 100 bpm. The pattern may be dependent on autonomic tone and the respiratory phase (with competing activation from the sinus node, AV node, and other areas in the atria).
The electrical impulses causing the atrial activity are moving or wandering. Observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular. Wandering atrial pacemaker is an arrhythmia originating in shifting pacemaker sites from the SA node to the atria and back to the SA ...
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.
Changes in anatomy and physiology result in electrocardiogram features that differ from the normal adult pattern and vary according to the age of the child. Sinus arrhythmia, ectopic atrial rhythm, "wandering pacemaker," and junctional rhythm can be normal characteristics in children (15%-25% of healthy children can have these rhythms on the ...
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury. Keywords: wandering atrial pacemaker, voltage, electrical injury, arrhythmia, ampere.
A wandering atrial pacemaker is a specific arrhythmia that can affect the heart. A condition that affects the rhythm or rate of the heartbeat is known as an arrhythmia. There are wide varieties of arrhythmia, including an irregular beat, an extra beat, and a fast or slow heart rate.
Wandering atrial pacemaker (Atrial escape) Junctional escape (40-60 BPM) Causes of Bradycardia with wide QRS: Ventricular Escape (30-40 BPM) Escape above bifurcation of His with aberrancy; Tachycardia. Definition: Three successive beats faster than normal for age. Types: Sinus tachycardia Atrial tachycardia Junctional tachycardia
A wandering atrial pacemaker and multifocal atrial tachycardia are irregularly irregular arrhythmias that differ mainly in their rate of ventricular conduct...
A 68-year-old woman with hypertension complains of intermittent dyspnea and light-headedness. She is asymptomatic during the evaluation. Vital signs are normal, but an irregularly irregular pulse is noted on examination as well as on the telemetry monitor. The 12-lead ECG is shown here; the ECG machine printout reads "atrial fibrillation." The patient has no history of this arrhythmia.